Mycosis fungoides is a lymphoma of skin-homing CD4+ T-helper cells presenting in the skin.
What is the Pathology of Mycosis Fungoides?
The pathology of mycosis fungoides is:
-Etiology: The cause of mycosis fungoides is unknown.
-Genes involved: None.
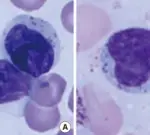
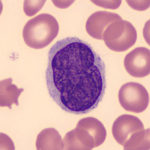
-Pathogenesis: The sequence of events that lead to mycosis fungoides involve proliferating cells that are clonal populations of CD4+ T-helper cells that home to the skin due to expression of cutaneous lymphocyte antigen. The neoplastic cells have clonal T-cell receptor gene rearrangements and may express aberrant combinations of T-cell surface antigens.
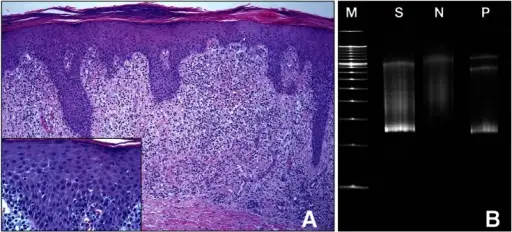
-Histology: The histology associated with mycosis fungoides shows the presence of atypical cells that form band-like aggregates with the superficial dermis and invade the epidermis as single cells and small clusters. These cells have markedly infolded nuclear membranes, imparting a convoluted or cerebriform contour.
How does Mycosis Fungoides Present?
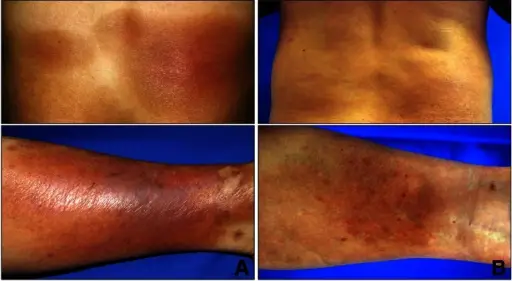
Patients with mycosis fungoides typically affect patients older than age 40 but may occur at any age and is frequently seen in men than women. The symptoms, features, and clinical findings associated with mycosis fungoides include lesions involving truncal areas and include scaly, red brown patches; raised scaling plaques and fungating nodules. Lesions may affect numerous body surfaces including the trunk, extremities, face and scalp.
How is Mycosis Fungoides Diagnosed?
Mycosis fungoides is diagnosed mainly through exclusion correlating clinical, histologic and molecular data. Smear, flow cytometry and clonality testing may be helpful.
How is Mycosis Fungoides Treated?
Mycosis fungoides is treated depending on the stage of the skin lesions. For early skin lesions, steroids or UV light is used. For advanced skin lesions, aggressive systemic chemotherapy is indicated.
What is the Prognosis of Mycosis Fungoides?
The prognosis of mycosis fungoides is fair with a median survival for early stages of ≥ 20 years and median survival of late stages of the disease of around 5 years.