Bone pathology is any disease or disorder that affects bone. A bone pathologist specializes in a subspecialty of surgical pathology that deals with the diagnosis and feature of many bone diseases.
What are Developmental Disorders of Bone and Cartilage?
Developmental disorders of bone and cartilage are pathologies that certain individuals are born with that affect cartilage or bone.
Developmental disorders of bone and cartilage include:
- Achondroplasia
- Achondrogenesis type 2
- Brachydactyly types D and E
- Campomelic dysplasia
- Cleidocranial dysplasia
- Holt-Oram syndrome
- Hypochondroplasia
- Metaphyseal dysplasia, Schmid type
- Nail-patella syndrome
- Osteogenesis imperfecta types 1-4
- Osteopetrosis, autosomal dominant
- Osteopetrosis, infantile type
- Osteopetrosis late-onset type 2
- Osteopetrosis with renal tubular acidosis
- Thanatophoric dysplasia
- Waardenburg syndrome types 1 and 3
What is Achondroplasia?
Achondroplasia is a rare autosomal dominant genetic disorder characterized by a transmembrane mutation in the fibroblast growth factor receptor.
What is the Pathology of Achondroplasia?
The pathology of achondroplasia is:
-Etiology: The cause of achondroplasia is a point mutation.
-Genes involved: FGFR-3.
-Pathogenesis: The sequence of events that lead to achondroplasia is the gene coding for the transmembrane portion of FGFR3, which resides on the short arm of chromosome 4, resulting in achondroplasia.
How does Achondroplasia Present?
Patients with achondroplasia are typically males or females that are born with the condition. The symptoms, features, and clinical findings associated with achondroplasia become more apparent in childhood, and early teenage years. Symptoms include short stature, macrocephaly, and frontal bossing.
How is Achondroplasia Diagnosed?
Achondroplasia is diagnosed by physical examination.
How is Achondroplasia Treated?
Achondroplasia is treated by supportive management and spinal decompression.
What is the Prognosis of Achondroplasia?
The prognosis of achondroplasia is generally good. Achondroplasia is the most common non-lethal skeletal dysplasia.
What is Thanatophoric Dysplasia?
Thanatophoric dysplasia is a severe autosomal dominant skeletal disorder characterized by a disproportionately small ribcage, extremely short limbs, and folds of extra skin on the arms and legs.
What is the Pathology of Thanatophoric Dysplasia?
The pathology of thanatophoric dysplasia is:
-Etiology: The cause of thanatophoric dysplasia is a missense mutation in fibroblast growth factor receptor-3.
-Genes involved: FGFR-3.
-Pathogenesis: The sequence of events that lead to thanatophoric dysplasia is the point mutations within FGFR3 which signal negative signals to the cartilage cells.
-Histology: The histology associated with thanatophoric dysplasia shows diminished proliferation of chondrocytes and poor columnization of the zone of proliferation.
How does Thanatophoric Dysplasia Present?
Patients with thanatophoric dysplasia typically are both males and females in equal proportion. The symptoms, features, and clinical findings associated with thanatophoric dysplasia include disproportionately short arms and legs with extra folds of skin. Other signs of the disorder include a narrow chest, small ribs, underdeveloped lungs, and an enlarged head with a large forehead and wide-spaced eyes.
How is Thanatophoric Dysplasia Diagnosed?
Thanatophoric dysplasia is diagnosed by prenatal ultrasound examination or low dose fetal CT.
How is Thanatophoric Dysplasia Treated?
Thanatophoric dysplasia is treated by inpatient care, as there is no treatment available.
What is the Prognosis of Thanatophoric Dysplasia?
The prognosis of thanatophoric dysplasia is very poor. It is extremely and almost always lethal without aggressive treatment.
What is Osteogenesis Imperfecta?
Osteogenesis imperfecta is a genetic disorder of connective tissues caused by an abnormality in the synthesis or processing of type I collagen.
What is the Pathology of Osteogenesis Imperfecta?
The pathology of osteogenesis imperfecta is:
-Etiology: The cause of osteogenesis imperfecta is mutations in the COL1A1 and COL1A2 genes.
-Genes involved: COL1A1 and COL1A2.
-Pathogenesis: The sequence of events that lead to osteogenesis imperfecta is the loss of function mutations like stop mutations that lead to haploinsufficiency.
-Histology: The histology associated with osteogenesis imperfecta shows crowded osteocytes within the bone.
How does Osteogenesis Imperfecta Present?
Patients with osteogenesis imperfecta typically affect both males and females present at any age depending upon the severity of the presenting symptoms. The symptoms, features, and clinical findings associated with osteogenesis imperfecta include blue sclera, short stature, loose joints, hearing loss, breathing problems, and teeth problems.
How Is Osteogenesis Imperfecta Diagnosed?
Osteogenesis imperfecta is diagnosed based on clinical features, family history, and genetic tests.
How Is Osteogenesis Imperfecta Treated?
Osteogenesis imperfecta is treated through fracture care, physical therapy, and surgical procedures.
What is the Prognosis of Osteogenesis Imperfecta?
The prognosis of osteogenesis imperfecta is good. An individual can live a normal lifespan.
What is Osteopetrosis?
Osteopetrosis is a rare, hereditary, diffuse, and symmetric skeletal sclerosis caused by osteoclast dysfunction.
What is the Pathology of Osteopetrosis?
The pathology of osteopetrosis is:
-Etiology: The cause of osteopetrosis is osteoclastic dysfunction resulting from gene mutations in at least 8 different genes.
-Genes involved: TCIRG1, CLCN7, OSTM1, PLEKHM1, SNX10, TNFSF11 and TNFRSF11A.
-Pathogenesis: The sequence of events that lead to osteopetrosis is osteoclast dysfunction.
-Histology: The histology associated with osteopetrosis shows primarily woven bone, central core of cartilage with dense and irregular bony trabeculae, often abundant osteoclasts, and reduced marrow space.
How does Osteopetrosis Present?
Patients with osteopetrosis typically affect both males and females presenting at infancy or adulthood. The symptoms, features, and clinical findings associated with osteopetrosis include brittle bone, bone sclerosis, bone marrow failure, and extramedullary hematopoiesis.
How is Osteopetrosis Diagnosed?
Osteopetrosis is diagnosed by a thorough clinical evaluation, detailed patient history, and an X-ray.
How is Osteopetrosis Treated?
Osteopetrosis is treated by bone marrow transplantation.
What is the Prognosis of Osteopetrosis?
The prognosis of osteopetrosis is poor with shortened life expectancy.
What is Osteopenia?
Osteopenia is a decrease in bone mineral density below normal reference values, yet not low enough to meet the diagnostic criteria to be considered osteoporotic.
What is the Pathology of Osteopenia?
The pathology of osteopenia is:
-Etiology: The etiology of osteopenia is aging.
-Genes involved: There are no genetic factors involved in osteopenia.
-Pathogenesis: The sequence of events that lead to osteopenia occurs secondary to uncoupling of osteoclast-osteoblast activity, resulting in a quantitative decrease in bone mass.
How does Osteopenia Present?
Patients with osteopenia typically affect females 4 times more than males present in the post-menopausal age group. The symptoms, features, and clinical findings associated with osteopenia are not appreciable, except for an increased propensity of getting fractures in severe cases.
How is Osteopenia Diagnosed?
Osteopenia is diagnosed by the DXA scans.
How is Osteopenia Treated?
Osteopenia is treated with calcium supplements, a healthy diet, and exercise.
What is the Prognosis of Osteopenia?
The prognosis of osteopenia is good if diet and exercise recommendations are followed.
What is Osteoporosis?
Osteoporosis is defined as low bone mineral density caused by altered bone microstructure, ultimately predisposing patients to low-impact, fragility fractures.
What is the Pathology of Osteoporosis?
The pathology of osteoporosis is:
-Etiology: The cause of osteoporosis is dietary factors.
-Genes involved: ESR1, LRP5, SOST, OPG, RANK, and RANKL.
-Pathogenesis: The sequence of events that lead to osteoporosis is an imbalance between bone resorption and bone formation.
-Histology: The histology associated with osteoporosis shows markedly thinned trabeculae, decreased osteon size, and enlarged Haversian canal and marrow spaces.
How does Osteoporosis Present?
Patients with osteoporosis typically affect women between 50-70 years of age. The symptoms, features, and clinical findings associated with osteoporosis show stooped postures, back pain, fragile bone, and fractures.
How is Osteoporosis Diagnosed?
Osteoporosis is diagnosed by conventional radiography and bone mineral density.
How is Osteoporosis Treated?
Osteoporosis is treated by lifestyle modifications along with medications such as calcium and vitamin D supplements.
What is the Prognosis of Osteoporosis?
The prognosis of osteoporosis is good if bone loss is detected in the early phases and proper intervention is undertaken.
What is Paget Disease of the Bone?
Paget disease of the bone is a condition involving cellular remodeling and deformity of one or more bones.
What is the Pathology of Paget Disease of the Bone?
The pathology of Paget disease of the bone is:
-Etiology: The cause of Paget disease of the bone is unknown.
-Genes involved: SQSTM1 and RANK.
-Pathogenesis: The sequence of events that lead to Paget disease of the bone involves an increase in osteoclastic resorption of bone.
-Histology: The histology associated with Paget disease of the bone shows primarily woven bone, a focal mosaic pattern of lamellar bone, resembling a jigsaw puzzle with prominent irregular cement lines.
How does Paget Disease of the Bone Present?
Patients with Paget disease of the bone typically affect males more than females over 55 years of age. The symptoms, features, and clinical findings associated with Paget disease of the bone include bone pain.
How is Paget Disease of the Bone Diagnosed?
Paget disease of the bone is diagnosed usually by elevated alkaline phosphatase in the blood.
How is Paget Disease of the Bone Treated?
Paget disease of the bone is treated with bisphosphonates, calcitonin, supplements such as Vitamin D and calcium, NSAIDs, and acetaminophen for pain management.
What is the Prognosis of Paget Disease of the Bone?
The prognosis of Paget disease of the bone is progressive and slowly worsens with time, although people may remain minimally symptomatic.
What is Osteomalacia?
Osteomalacia is a disease characterized by the softening of the bones caused by impaired bone metabolism primarily due to inadequate levels of available phosphate, calcium, and vitamin D, or because of resorption of calcium.
What is the Pathology of Osteomalacia?
The pathology of osteomalacia is:
-Etiology: The cause of osteomalacia is vitamin D deficiency.
-Genes involved: FGF-23, PHEX mutations.
-Pathogenesis: The sequence of events that lead to osteomalacia is the coordinated process of bone remodeling.
-Histology: The histology associated with osteomalacia shows a wide, noncalcified matrix surrounding disorganized bone trabeculae.
How does Osteomalacia Present?
Patients with osteomalacia typically affect both males and females in their adulthood. The symptoms, features, and clinical findings associated with osteomalacia include diffuse body pains, muscle weakness, and fragility of the bones.
How is Osteomalacia Diagnosed?
Osteomalacia is diagnosed by biopsy of a long bone or iliac crest.
How is Osteomalacia Treated?
Osteomalacia is treated by administration of vitamin D3.
What is the Prognosis of Osteomalacia?
The prognosis of osteomalacia is good.
What is Rickets?
Rickets is a condition characterized by a defect in mineralization of the epiphyseal plates.
What is the Pathology of Rickets?
The pathology of rickets is:
-Etiology: The cause of rickets is vitamin D deficiency.
-Genes involved: PHEX, FGF-23, and VDR.
-Pathogenesis: The sequence of events that lead to rickets involves decreased availability of phosphorus and calcium to mineralize the skeletal matrix, leading to growth plate disorganization and accumulation of under mineralized osteoid.
-Histology: The histology associated with rickets shows thickened, poorly defined growth plates, particularly on the metaphyseal side, tongues of uncalcified cartilage may extend into metaphysis, wide osteoid seams.
How does Rickets Present?
Patients with rickets typically affect males and females present at the age range of 2 and above. The symptoms, features, and clinical findings associated with rickets include bone tenderness, bowed legs or knock knees, thickened wrists and ankles, and breastbone projection.
How is Rickets Diagnosed?
Rickets is diagnosed by blood tests showing serum calcium, serum phosphorous, and serum alkaline phosphatase levels, bone density scan, or radiography.
How is Rickets Treated?
Rickets is treated by use of vitamin D along with exposure to sunlight.
What is the Prognosis of Rickets?
The prognosis of rickets is generally good. However, a complete recovery can take some time.
What is Hyperparathyroidism?
Hyperparathyroidism is an increase in parathyroid hormone levels in the blood.
What is the Pathology of Hyperparathyroidism?
The pathology of hyperparathyroidism is:
-Etiology: The cause of hyperparathyroidism is increased parathyroid or parathyroid like hormones.
-Genes involved: MEN1, CDC73, or CASR gene.
-Pathogenesis: The sequence of events that lead to hyperparathyroidism is the excessive secretion of PTH due to a disorder of the parathyroid glands.
-Histology: The histology associated with hyperparathyroidism shows osteoblastic and osteoclastic activity, cysts, hemosiderin-laden macrophages.
How does Hyperparathyroidism Present?
Patients with hyperparathyroidism typically affect women in the age range of 50 years. The symptoms, features, and clinical findings associated with hyperparathyroidism include weakness and fatigue, depression, bone pain, muscle soreness, decreased appetite, feelings of nausea and vomiting, constipation, pancreatitis, polyuria, polydipsia, cognitive impairment, kidney stones, vertigo, and osteopenia or osteoporosis.
How is Hyperparathyroidism Diagnosed?
Hyperparathyroidism is diagnosed by PTH immunoassay, or biopsy.
How is Hyperparathyroidism Treated?
Hyperparathyroidism is treated by surgical interventions such as parathyroidectomy.
What is the Prognosis of Hyperparathyroidism?
The prognosis of hyperparathyroidism is usually excellent, and most people are cured after successful parathyroidectomy.
What is Renal Osteodystrophy?
Renal osteodystrophy is a broad term that incorporates all the biochemical abnormalities and skeletal manifestations in patients suffering from chronic kidney disease or end-stage renal disease.
What is the Pathology of Renal Osteodystrophy?
The pathology of renal osteodystrophy is:
-Etiology: The cause of renal osteodystrophy in chronic kidney disease and secondary hyperparathyroidism.
-Genes involved: PTHR1.
-Pathogenesis: The sequence of events that lead to renal osteodystrophy result from hyperparathyroidism secondary to hyperphosphatemia combined with hypocalcemia, both of which are due to decreased excretion of phosphate by the damaged kidney.
-Histology: The histology associated with renal osteodystrophy shows high bone turnover and low bone turnover states.
How does Renal Osteodystrophy Present?
Patients with renal osteodystrophy typically affect males and females present at the age range of 40 and above. The symptoms, features, and clinical findings associated with renal osteodystrophy include bone pain, joint pain, bone deformation, and bone fracture.
How is Renal Osteodystrophy Diagnosed?
Renal Osteodystrophy is diagnosed by bone biopsy.
How is Renal Osteodystrophy Treated?
Renal Osteodystrophy is treated with phosphate binders, vitamin D compounds, and calcimimetics.
What is the Prognosis of Renal Osteodystrophy?
The prognosis of renal osteodystrophy is generally good after kidney transplantation.
What are Bone Fractures?
Bone fractures are a medical condition in which there is a partial or complete break in the continuity of a bone.
Types of fractures include:
- Simple fractures
- Compound fractures
- Displaced fractures
- Stress fractures
- Greenstick fractures
- Pathologic fractures
What are Simple Fractures?
Simple fractures are those in which the overlying skin is intact.
What are Compound Fractures?
Compound fractures are a type of bone fracture caused by high-energy trauma.
What are Displaced Fractures?
Displaced fractures are a type of fracture, in the bone that snaps into two or more parts and moves so that the two ends are not lined up straight.
What are Stress Fractures?
A stress fracture is a fatigue-induced bone fracture caused by repeated stress over time.
What are Greenstick Fractures?
A greenstick fracture is a fracture in a young, soft bone in which the bone bends and breaks.
What are Pathologic Fractures?
Pathologic fractures are bone fractures caused by weakness of the bone structure, usually, due to an underlying pathology that leads to decreased mechanical resistance to normal mechanical loads.
How do Fractures Heal?
Fractures heal by the following steps:
- Hematoma formation
- Fibrocartilaginous callus formation
- Bony callus formation
- Bone remodeling
What is Osteonecrosis?
Osteonecrosis is a degenerative bone condition characterized by the death of cellular components of the bone secondary to an interruption of the subchondral blood supply.
What is the Pathology of Osteonecrosis?
The pathology of osteonecrosis is:
-Etiology: The causes of osteonecrosis are bone fractures, joint dislocations, alcoholism, and the use of high-dose steroids.
-Genes involved: ADH2, ADH3, ALDH2 and P450E1.
-Pathogenesis: The sequence of events that lead to osteonecrosis involves the death of cellular elements of the bone marrow.
-Histology: The histology associated with osteonecrosis shows dead trabeculae stain deeper blue than non necrotic bone.
How does Osteonecrosis Present?
Patients with osteonecrosis typically affect both males and females 30-50 years of age. The symptoms, features, and clinical findings associated with osteonecrosis include pain and discomfort in a joint which increases over time.
How is Osteonecrosis Diagnosed?
Osteonecrosis is diagnosed by bone scintigraphy and MRI.
How is Osteonecrosis Treated?
Osteonecrosis is treated by NSAIDs, physiotherapy, and surgery.
What is the Prognosis of Osteonecrosis?
The prognosis of osteonecrosis is good. Most people fully recover from osteonecrosis and are eventually able to use the affected joint without pain.
What is Osteomyelitis?
Osteomyelitis is a serious infection of the bone that can be either acute or chronic. It is an inflammatory process involving the bone and its structures caused by pyogenic organisms that spread through the bloodstream, fractures, or surgery.
Types of osteomyelitis include:
- Pyogenic osteomyelitis
- Mycobacterial osteomyelitis
- Skeletal syphilis
What is Pyogenic Osteomyelitis?
Pyogenic osteomyelitis is an inflammation of the bone caused by an infecting organism.
What is the Pathology of Pyogenic Osteomyelitis?
The pathology of pyogenic osteomyelitis is:
-Etiology: The cause of pyogenic osteomyelitis is Staphylococcus aureus.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pyogenic osteomyelitis occurs both by direct routes and by hematogenous spread from an infection of the skin, urogenital tract, lung, or upper respiratory tract.
-Histology: The histology associated with pyogenic osteomyelitis shows neutrophils, lymphocytes, and plasma cells with bone necrosis and reactive new bone formation.
How does Pyogenic Osteomyelitis Present?
Patients with pyogenic osteomyelitis typically affect males more than females both young and old. The symptoms, features, and clinical findings associated with pyogenic osteomyelitis include pain in a specific bone with overlying redness, fever, weakness, and inability to walk especially in children with acute bacterial osteomyelitis.
How is Pyogenic Osteomyelitis Diagnosed?
The diagnosis of pyogenic osteomyelitis is through radiographs, MRI, and CT scans.
How is Pyogenic Osteomyelitis Treated?
Pyogenic osteomyelitis is treated by prolonged antibiotic therapy for weeks or months.
What is the Prognosis of Pyogenic Osteomyelitis?
The prognosis of pyogenic osteomyelitis is good with aggressive treatment however, there is a chance of recurrence of the infection.
What is Mycobacterial Osteomyelitis?
Mycobacterial osteomyelitis is the infection of the bone or the bone marrow by mycobacterium tuberculosis.
What is the Pathology of Mycobacterial Osteomyelitis?
The pathology of Mycobacterial osteomyelitis is:
-Etiology: The cause of mycobacterial osteomyelitis is Mycobacterium tuberculosis
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to mycobacterial osteomyelitis involves the infection of the bone marrow caused by both nonspecific and specific agents.
-Histology: The histology associated with mycobacterial osteomyelitis shows dense infiltration of leukocytes, granulation tissue, and bone sequester.
How does Mycobacterial Osteomyelitis Present?
Patients with mycobacterial osteomyelitis typically affect males more than females both in childhood and adulthood. The symptoms, features, and clinical findings associated with mycobacterial osteomyelitis include pain in a specific bone with overlying redness, fever, weakness, and inability to walk especially in children with acute bacterial osteomyelitis.
How is Mycobacterial Osteomyelitis Diagnosed?
Mycobacterial osteomyelitis is diagnosed by symptoms and laboratory tests such as CRP and ESR further supported by medical imaging and bone biopsy.
How is Mycobacterial Osteomyelitis Treated?
Mycobacterial osteomyelitis is treated by prolonged antibiotic therapy, often in conjunction with surgical intervention, particularly for spinal tuberculosis.
What is the Prognosis of Mycobacterial Osteomyelitis?
The prognosis of mycobacterial osteomyelitis is good with aggressive treatment.
What is Skeletal Syphilis?
Skeletal syphilis or osseous syphilis bony involvement by Treponema pallidum.
What is the Pathology of Skeletal Syphilis?
The pathology of skeletal syphilis is:
-Etiology: The cause of skeletal syphilis is bacterium treponema pallidum
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to skeletal syphilis involves a tiny organism called treponema.
-Histology: The histology associated with skeletal syphilis shows interstitial inflammation, endothelial swelling, irregular acanthosis, elongated rete ridges, a vacuolar pattern with lymphocytic infiltration.
How does Skeletal Syphilis Present?
Patients with skeletal syphilis typically affect males 20-50 years of age. The symptoms, features, and clinical findings associated with skeletal syphilis include periostitis, osteitis, osteomyelitis, and osteolysis.
How is Skeletal Syphilis Diagnosed?
Skeletal syphilis is diagnosed by dark-field microscopy and serological tests.
How is Skeletal Syphilis Treated?
Skeletal syphilis is treated by penicillin which is the drug of choice.
What is the Prognosis of Skeletal Syphilis?
The prognosis of skeletal syphilis is variable.
What are Bone Tumors?
Bone tumors are an abnormal growth of tissue in bone, traditionally classified as benign or malignant.
Examples of bone tumors include:
- Osteoid osteoma
- Osteoblastoma
- Osteosarcoma
What is an Osteoid Osteoma?
Osteoid osteoma is a benign bone tumor that arises from osteoblasts and some components of osteoclasts.
What is the Pathology of Osteoid Osteoma?
The pathology of osteoid osteoma is:
-Etiology: The cause of osteoid osteoma remains uncertain.
-Genes involved: YWHAH and PDGF-B.
-Pathogenesis: The sequence of events that lead to osteoid osteoma occurs when certain cells divide uncontrollably, forming a small mass of bone and other tissue.
-Histology: The histology associated with osteoid osteoma shows small, yellow to the red nidus of osteoid and woven bone with interconnected trabeculae, and background and rim of highly vascularized, fibrous connective tissue.
How does Osteoid Osteoma Present?
Patients with osteoid osteoma typically affect males 3 times more than females in 20-30 years of age. The symptoms, features, and clinical findings associated with osteoid osteoma include dull pain that escalates to severe at night or slight pain, rising to become severe even at night-time, affecting sleep quality, limping, muscle atrophy, bowing deformity, swelling, increased or decreased bone growth.
How is Osteoid Osteoma Diagnosed?
Osteoid osteoma is diagnosed by radiographs.
How is Osteoid Osteoma Treated?
Osteoid osteoma is treated by conservative management with NSAIDs.
What is the Prognosis of Osteoid Osteoma?
The prognosis of osteoid osteoma is good since it is a benign process with no potential for malignant degeneration.
What is an Osteoblastoma?
Osteoblastoma is a rare benign bone-forming neoplasm which produces woven bone spicules, which are bordered by prominent osteoblasts.
What is the Pathology of Osteoblastoma?
The pathology of osteoblastoma is:
-Etiology: The cause of osteoblastoma is unknown.
-Genes involved: MDM2, TP53, and PNCA.
-Pathogenesis: The sequence of events that lead to osteoblastoma expresses Runx2 and osterix, transcription factors involved in osteoblastic differentiation.
-Histology: The histology associated with osteoblastoma shows anastomosing woven bone trabeculae, lined by a single but prominent layer of osteoblasts, and intervening hypervascular, hypocellular intertrabecular spaces.
How does Osteoblastoma Present?
Patients with osteoblastoma typically affect males more than females in 20-30 years of age. The symptoms, features, and clinical findings associated with osteoblastoma include pain of several months in duration.
How is Osteoblastoma Diagnosed?
Osteoblastoma is diagnosed by X-ray, MRI, and CT scan.
How is Osteoblastoma Treated?
Osteoblastoma is treated by surgical excision.
What is the Prognosis of Osteoblastoma?
The prognosis of osteoblastoma is excellent, with most patients cured following the initial surgical treatment.
What is an Osteosarcoma?
Osteosarcoma is a high-grade malignant primary central sarcoma of bone characterized by the presence of an osteoid extracellular matrix.
What is the Pathology of Osteosarcoma?
The pathology of osteosarcoma is:
-Etiology: The cause of osteosarcoma is unknown.
-Genes involved: TP53, RB1.
-Pathogenesis: The sequence of events that lead to osteosarcoma occurs when a healthy bone cell develops changes in its DNA.
-Histology: The histology associated with osteosarcoma shows sarcomatous tumor cells that produce malignant bone or osteoid.
How does Osteosarcoma Present?
Patients with osteosarcoma typically affect males more than females in childhood and adulthood. The symptoms, features, and clinical findings associated with osteosarcoma include pain that may be worse at night, maybe intermittent and of varying intensity, and may have been occurring for a long time.
How is Osteosarcoma Diagnosed?
Osteosarcoma is diagnosed by MRI, CT scan, and PET scan.
How is Osteosarcoma Treated?
Osteosarcoma is treated by a combination of chemotherapy and surgery.
What is the Prognosis of Osteosarcoma?
The prognosis of osteosarcoma is variable depending upon the stage of the tumor. Stage 1 has an excellent prognosis. Stage 2 has a poor prognosis.
What are Cartilage Tumors?
Cartilage tumors, also known as chondrogenic tumors, are a type of bone tumor that develops in cartilage and are divided into non-cancerous, cancerous, and intermediate locally aggressive types.
Examples of cartilage-forming tumors include:
- Chordomas
- Osteochondromas
- Chondrosarcomas
What are Chordomas?
Chondroma is a benign cartilaginous tumor, which is encapsulated with a lobular growing pattern.
What is the Pathology of Chondromas?
The pathology of chondromas is:
-Etiology: The cause of chondromas is unknown.
-Genes involved: IDH1, IDH2.
-Pathogenesis: The sequence of events that lead to chondromas involves mutations in IDH1 and IDH2 resulting in increased levels of the oncometabolite D-2-hydroxyglutarate (D-2-HG.) D-2-HG competitively inhibits alpha-ketoglutarate-dependent enzymes.
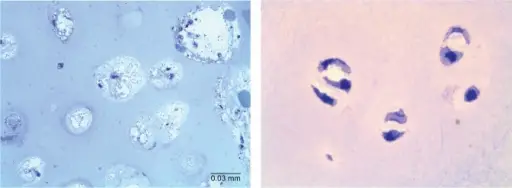
-Histology: The histology associated with chondromas shows plump tumor cells with fine punctate calcification.
How does Chondromas Present?
Patients with chondromas typically affect both males and females between 5-80 years of age. The symptoms, features, and clinical findings associated with chondromas are often nonspecific and found as a result of a pathologic fracture/trauma or localized versus radiating pain.
How is Chondromas Diagnosed?
Chondromas are diagnosed by radiography, CT scan, and MRI.
How is Chondromas Treated?
Chondroma is treated by surgically scraped out of the bone.
What is the Prognosis of Chondromas?
The prognosis of chondromas is good since it is self-limiting, and recurrence is rare.
What are Osteochondromas?
Osteochondromas are an overgrowth of cartilage and bone that happens at the end of the bone near the growth plate.
What is the Pathology of Osteochondromas?
The pathology of osteochondromas is:
-Etiology: The cause of osteochondromas is associated with loss of function mutations in EXT1 (8q24) and EXT2.
-Genes involved: EXT1, EXT2.
-Pathogenesis: The sequence of events that lead to osteochondromas involves abnormal outgrowth of bone and cartilage, associated with the aberrant development of the growth plate.
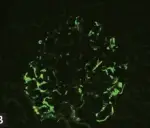
-Histology: The histology associated with osteochondromas shows a cap composed of mature hyaline cartilage with an overlying fibrous perichondrium.
How does Osteochondromas Present?
Patients with osteochondromas typically affect males in the first two decades of life. The symptoms, features, and clinical findings associated with osteochondromas include a hard immobile painless palpable mass, adjacent muscle soreness, and pressure or irritation with heavy exercising.
How is Osteochondromas Diagnosed?
Osteochondromas are diagnosed by radiography, CT scan, MRI, as well as biopsy of the lesion.
How is Osteochondromas Treated?
Osteochondromas are treated by surgical excision.
What is the Prognosis of Osteochondromas?
The prognosis of osteochondromas is good with malignant transformation occurring in <2% of patients.
What are Chondrosarcomas?
Chondrosarcoma is a type of bone cancer that develops in cartilage cells.
What is the Pathology of Chondrosarcomas?
The pathology of chondrosarcomas is:
-Etiology: The cause of chondrosarcomas is unknown.
-Genes involved: IDH, CDKN2A, and COL2A1.
-Pathogenesis: The sequence of events that lead to chondrosarcomas are the chromosomal anomalies detected in some types of chondrosarcomas including 9p21, 10, 13q14, and 17p13.
-Histology: The histology associated with chondrosarcomas shows recognizable lacunae, often containing binucleated or multinucleated chondrocytes.
How do Chondrosarcomas Present?
Patients with chondrosarcomas typically affect middle-aged males. The symptoms, features, and clinical findings associated with chondrosarcomas include back or thigh pain, sciatica, bladder symptoms, and unilateral edema.
How are Chondrosarcomas Diagnosed?
Chondrosarcomas are diagnosed by imaging studies (X-ray, CT scan, MRI) in combination with biopsy specimens.
How is Chondrosarcomas Treated?
Chondrosarcomas are treated by wide surgical resection.
What is the Prognosis of Chondrosarcomas?
The prognosis of chondrosarcomas is poor.
What are Tumors of Bone or Cartilage of Unknown Origin?
Tumors of bone or cartilage of unknown origin are those tumors that originate elsewhere in the body with their location unknown but finally invade bone.
Examples of bone or cartilage of unknown origin include:
- Aneurysmal bone cyst
- Ewing sarcoma family tumors
- Giant cell tumor
What is an Aneurysmal Bone Cyst?
An aneurysmal bone cyst is a non-cancerous bone tumor composed of multiple varying sizes of spaces in a bone that is filled with blood.
What is The Ewing Family of Tumors?
The Ewing family of tumors is a group of cancers that includes Ewing sarcoma, extraosseous Ewing tumors, primitive neuroectodermal tumors (PNET).
What is Ewing Sarcoma?
Ewing sarcoma is a malignant, distinctive small round cell sarcoma associated with a t(11:22) translocation and most commonly occurs in the diaphysis of long bones.
What is the Pathology of Ewing Sarcoma?
The pathology of Ewing sarcoma is:
-Etiology: The cause of Ewing sarcoma is not exactly known.
-Genes involved: EWSR1-FLI1 fusion.
-Pathogenesis: The sequence of events that lead to Ewing sarcoma is due to t(11:22) translocation which leads to the formation of a fusion protein (EWS-FLI1).
-Histology: The histology associated with Ewing sarcoma shows small round cells with an increased nuclear-cytoplasmic ratio that represents a family of small round blue cell tumors.
How does Ewing Sarcoma Present?
Patients with Ewing sarcoma typically affect males more than females in less than 20 years of age. The symptoms, features, and clinical findings associated with Ewing sarcoma include intermittent fevers, anemia, leukocytosis, increased sedimentation rate, and other symptoms of inflammatory systemic illness.
How is Ewing Sarcoma Diagnosed?
Ewing sarcoma is diagnosed by integration of clinical, radiographic, immunohistochemical, and molecular information.
How is Ewing Sarcoma Treated?
Ewing sarcoma is treated by multidrug chemotherapy such as vincristine, cyclophosphamide, doxorubicin, etoposide, or ifosfamide.
What is the Prognosis of Ewing Sarcoma?
The prognosis of Ewing sarcoma is fair.
What is Giant Cell Tumor?
Giant cell tumors are benign, aggressive tumors typically found in the epiphysis of long bones, most commonly at the distal femur and proximal tibia.
What is the Pathology of a Giant Cell Tumor?
The pathology of a giant cell tumor is:
-Etiology: The cause of giant cell tumors is not fully understood yet.
-Genes involved: G34W mutation of H3F3A gene.
-Pathogenesis: The sequence of events that lead to a giant cell tumor is the metastatic lesions often noted to have alterations in c-Myc oncogene or p53.
-Histology: The histology associated with giant cell tumors shows highly cellular lesions composed of a large number of nonneoplastic osteoclast-like giant cells, between which mononuclear neoplastic cells are embedded.
How does Giant Cell Tumor Present?
Patients with giant cell tumors typically affect both males and females at 35 years of age. The symptoms, features, and clinical findings associated with giant cell tumors include pain and limited range of motion caused by the tumor’s proximity to the joint space. Swelling may occur, as well, if the tumor has been growing for a long time.
How is a Giant Cell Tumor Diagnosed?
Giant cell tumor diagnosis is suggested by X-ray, CT scan, and MRI.
How is Giant Cell Tumor Treated?
Giant cell tumor is treated by curettage and high-speed drilling with local adjuvants.
What is the Prognosis of a Giant Cell Tumor?
The prognosis of giant cell tumors is fair.
What Lesions are Similar to Primary Bone Neoplasms?
Lesions that are similar to primary bone neoplasms are described as follows.
Examples of lesions are similar to primary bone neoplasms include:
- Fibrous cortical defect
- Fibrous dysplasia
- Nonossifying fibroma
What are Fibrous Cortical Defects?
Fibrous cortical defects are benign bony lesions and are a type of fibroxanthoma, histologically identical to the larger non-ossifying fibroma (NOF).
What is the Pathology of Fibrous Cortical Defects?
The pathology of fibrous cortical defects is:
-Etiology: The cause of fibrous cortical defects remains obscure.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to fibrous cortical defects results from periosteal injury or secondary to abnormalities at the epiphyseal plate.
-Histology: The histology associated with fibrous cortical defects shows lesions to be highly cellular containing spindle-shaped cells on a background of stromal tissue in a prominent storiform pattern.
How does Fibrous Cortical Defects Present?
Patients with fibrous cortical defects typically affect males between 2-15 years of age. The symptoms, features, and clinical findings associated with fibrous cortical defects include mild swelling and tenderness to the touch.
How are Fibrous Cortical Defects Diagnosed?
Fibrous cortical defects are diagnosed by imaging scans such as MRI, CT scan, and bone scan.
How are Fibrous Cortical Defects Treated?
Fibrous cortical defects are usually self-limiting, therefore no treatment, biopsy, or even follow-up is required in typical cases.
What is the Prognosis of Fibrous Cortical Defects?
The prognosis of fibrous cortical defects is excellent in those unusual cases where patients require curettage and bone graft.
What are Fibrous Dysplasias?
Fibrous dysplasia is a disorder where normal bone and marrow are replaced with fibrous tissue, resulting in the formation of bone that is weak and prone to expansion.
What is the Pathology of Fibrous Dysplasias?
The pathology of fibrous dysplasias is:
-Etiology: The cause of fibrous dysplasias has been linked with a missense mutation in the GNAS1 gene on chromosome 20.
-Genes involved: GNAS1.
-Pathogenesis: The sequence of events that lead to fibrous dysplasias involves the replacement of normal bone and bone marrow by fibro-osseous lesions.
-Histology: The histology associated with fibrous dysplasias shows anastomosing and branching irregular trabeculae of woven bone without osteoblastic rimming.
How does Fibrous Dysplasias Present?
Patients with fibrous dysplasias typically affect both males and females in the first three decades of life. The symptoms, features, and clinical findings associated with fibrous dysplasias include limp, pain, and/or pathologic fractures.
How are Fibrous Dysplasias Diagnosed?
Fibrous dysplasias is diagnosed by radiologic imaging and biopsy.
How are Fibrous Dysplasias Treated?
Fibrous dysplasias are treated by usually symptomatic management, or surgery in cases with a fracture or bony deformity.
What is the Prognosis of Fibrous Dysplasias?
The prognosis of fibrous dysplasias is widely variable as the disorder itself and is based on the bones affected, whether other structures such as nerves are affected, and whether fractures occur.
What are Nonossifying Fibromas?
Nonossifying fibromas are benign fibrohistiocytic tumors arising in the metaphysis of long bones of skeletally immature individuals, composed of bland fibroblastic proliferation mixed with osteoclast-like giant cells.
What is the Pathology of Nonossifying Fibromas?
The pathology of nonossifying fibromas is:
-Etiology: The cause of nonossifying fibromas is germline mutations resulting in activation of the KRAS-MAPK pathway.
-Genes involved: KRAS and FGFR1.
-Pathogenesis: The sequence of events that lead to nonossifying fibromas is the mutually exclusive hotspot mutations in KRAS and FGFR1.
-Histology: The histology associated with nonossifying fibromas shows bland, spindle-shaped fibroblasts arranged in a storiform pattern, interspersed with osteoclast-like multinucleated giant cells.
How does Nonossifying Fibromas Present?
Patients with nonossifying fibromas typically affect both males and females in the second decade of life. The symptoms, features, and clinical findings associated with nonossifying fibromas include pain, mild swelling, and soreness.
How are Nonossifying Fibromas Diagnosed?
Nonossifying fibromas are diagnosed by radiological and histopathological findings.
How are Nonossifying Fibromas Treated?
Nonossifying fibromas usually requires no treatment.
What is the Prognosis of Nonossifying Fibromas?
The prognosis of nonossifying fibromas is excellent, local recurrence is rare but reported.
How do Metastatic Tumors Affect Bone?
Metastatic tumors are the most common types of malignancies that affect the bones. Cancer that originates in one area of the body, such as an organ, gland, or tissue, and then spreads to the bone is called metastatic bone disease.
The most common cancers that spread to bone include:
- Breast cancer
- Lung cancer
- Thyroid cancer
- Kidney cancer
- Prostate cancer