Vascular pathology is any disease or disorder that affects the vascular system.
Vascular pathology includes:
- Vascular anomalies
- Vascular wall response to Injury
- Hypertensive vascular disease
- Arteriosclerosis
- Atherosclerosis
- Aneurysms
- Dissections
- Vasculitis
- Disorders of blood vessel
- Vein abnormalities
- Lymphatic abnormalities
- Vascular tumors
What are Vascular Anomalies?
Vascular anomalies are conditions are characterized by abnormal communication between the veins and the arteries.
Examples of vascular anomalies include:
- Berry aneurysms (see aneurysms)
- Arteriovenous fistulas
- Fibromuscular dysplasia
What are Arteriovenous Fistulas?
Arteriovenous fistulas are abnormal communication between the artery and the vein.
What is the Pathology of Arteriovenous Fistula?
The pathology of arteriovenous fistulas is:
-Etiology: The cause of arteriovenous fistulas is an injury where the two blood vessels are close to each other, can be congenital or rupture of aneurysms.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to arteriovenous fistula is when there is a condition or injury that causes a tear of either of the blood vessels that are close to each other and when healing begins, a connection between the two is created, causing blood to mix.
-Morphology: The morphology associated with arteriovenous fistulas shows a complete connection between the vein and the artery, and blood flows directly from the artery to the vein.
-Histology: Arterial and venous tissue.
How does Arteriovenous Fistula Present?
Patients with arteriovenous fistula typically are female at the age range from birth to adulthood. The symptoms, features, and clinical findings associated with an arteriovenous fistula include swelling of the part of the body with the affected vessels, low blood pressure, fatigue, heart failure, bulging veins, and a purplish color is noted.
How is Arteriovenous Fistula Diagnosed?
Arteriovenous fistula is diagnosed by physical examination, history taking, auscultation to hear any humming sound of the vessels, duplex ultrasound, CT scan, and MRI.
How is Arteriovenous Fistula Treated?
An arteriovenous fistula is treated by catheter embolization, ultrasound-guided compression, or surgery depending on the size and location of the fistula.
What is the Prognosis of Arteriovenous Fistula?
The prognosis of the arteriovenous fistula is good since it has a low mortality rate and with appropriate treatment.
What is Fibromuscular Dysplasia?
Fibromuscular dysplasia is a condition of the blood vessel that mostly affects the large arteries and is characterized by twisting, enlarging, and narrowing of the blood vessels.
What is the Pathology of Fibromuscular Dysplasia?
The pathology of fibromuscular dysplasia is:
-Etiology: The cause of fibromuscular dysplasia is unknown but can be predisposed by hormonal changes, genetics, and smoking.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to fibromuscular dysplasia is when blood vessels are weakened and movement as blood flow continues, it causes the blood vessels to twist several times and the weak walls of the blood vessels begin to bulge as the other part that has been deprived of blood begins to narrow due to its loss of function.
-Morphology: The morphology associated with fibromuscular dysplasia shows stenosis, bead-like appearance due to twisting, swelling.
-Histology: The histology associated with fibromuscular dysplasia shows collagen in the intima, thickened fibromuscular ridges, medial dysplasia, adventitial dysplasia, and intimal fibroplasia.
How does Fibromuscular Dysplasia Present?
Patients with fibromuscular dysplasia are typically females between 20-50 years old. The symptoms, features, and clinical findings associated with fibromuscular dysplasia include headache, dizziness, neck pain, weakness, numbness, intermittent leg claudication, and hypertension.
How is Fibromuscular Dysplasia Diagnosed?
Fibromuscular dysplasia is diagnosed by physical examination, history taking, cerebrovascular ultrasonography, CT scan, and MRI angiogram.
How is Fibromuscular Dysplasia Treated?
Fibromuscular dysplasia is treated by managing the symptoms as they present since there is no clear cause of the disease. Diuretics and antihypertensives may be helpful.
What is the Prognosis of Fibromuscular Dysplasia?
The prognosis of fibromuscular dysplasia is generally good. If cranial arteries are involved, then the prognosis worsens.
What is the Vascular Wall Response to Injury?
The vascular wall response to injury is a condition of the blood vessels that is characterized by endothelial cell loss or dysfunction triggers the recruitment of smooth muscle cells, which proliferate; and an associated increase in the synthesis of matrix products resulting in intimal thickening.
What is Hypertensive Vascular Disease?
Hypertensive vascular disease is also known as hypertension is a condition in which the blood pressure is elevated more than normal above 140/90 mmHg.
Hypertensive vascular disease includes:
- Essential hypertension
- Primary hypertension
- Secondary hypertension
What is Essential Hypertension?
Essential hypertension is a condition that is characterized by a rise in blood pressure but the cause is idiopathic.
What is the Pathology of Essential Hypertension?
The pathology of essential hypertension is:
-Etiology: The cause of essential hypertension is idiopathic but can be initiated by genetic factors, environmental factors, advanced age, increased alcohol intake.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to Essential hypertension is not clearly illustrated but the factors that lead to it are genetics, environmental factors, increased vascular resistance.
-Morphology: NA.
-Histology: NA.
How does Essential Hypertension Present?
Patients with essential hypertension typically all gender present at the age range of young adulthood to the elderly. The symptoms, features, and clinical findings associated with crucial hypertension include severe headache, increased blood pressure, nosebleed, dyspnea, blood in urine, and fatigue.
How is Essential Hypertension Diagnosed?
Essential hypertension is diagnosed by history taking, monitoring of the vital signs.
How is Essential Hypertension Treated?
Essential hypertension is treated by regular exercise, stress management, weight loss, reduce or cessation of alcohol intake.
What is the Prognosis of Essential Hypertension?
The prognosis of essential hypertension is good due.
What is Primary Hypertension?
Primary hypertension is a form of high blood pressure that occurs as a result of factors that are not medical related ed family history.
What is the Pathology of Primary Hypertension?
The pathology of primary hypertension is:
-Etiology: The cause of primary hypertension is smoking, alcohol intake, obesity, stress, inactivity, old age.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to primary hypertension is not fully clear but factors that lead to it are high plasma level of catecholamines, an increase in blood volume, arterial overfilling, arteriolar constriction, and increased cardiac output.
-Morphology: NA.
-Histology: NA.
How does Primary Hypertension Present?
Patients with primary hypertension typically are female that are 20 to 60 years old. The symptoms, features, and clinical findings associated with primary hypertension include irregular heartbeat, dizziness, fatigue, dyspnea: severe headaches, visual disturbances, and chest pain.
How is Primary Hypertension Diagnosed?
Primary hypertension is diagnosed by monitoring of the blood pressure and history taking.
How is Primary Hypertension Treated?
Primary hypertension is treated by cessation of alcohol intake, maintaining a healthy weight, avoid smoking.
What is the Prognosis of Primary Hypertension?
The prognosis of primary hypertension is good, with a low mortality rate if one adheres to medication.
What is Secondary Hypertension?
Secondary hypertension is an increase in blood pressure that is caused by underlying conditions
What is the Pathology of Secondary Hypertension?
The pathology of secondary hypertension is:
-Etiology: The cause of secondary hypertension may be due to renal diseases, neurologic diseases, endocrine disorders, and cardiovascular diseases.
-Genes involved: NA.
-Pathogenesis: The sequence of events that lead to secondary hypertension are caused by the underlying disease that the patient is having. These conditions cause increased vascular resistance of the blood vessels by either causing the formation of plaques in the blood vessels walls or narrowing the blood vessels leading to increased blood pressure.
-Morphology: NA.
-Histology: NA.
How does Secondary Hypertension Present?
Patients with secondary hypertension typically affect both males and females but during the ageless than 45 men are more affected than from 45years female are affected more present at the age range of from young age to above 65 years. The symptoms, features, and clinical findings associated with secondary hypertension include hypokalemia, apneic episodes, chest pain, severe headache.
How is Secondary Hypertension Diagnosed?
Secondary hypertension is diagnosed by measuring the blood pressure, physical examination and history taking,
How is Secondary Hypertension Treated?
Secondary hypertension is treated modification of the lifestyle, and antihypertensives.
What is the Prognosis of Secondary Hypertension?
The prognosis of secondary hypertension is good since it has a low mortality rate.
What is Arteriosclerosis?
Arteriosclerosis is medically defined as the hardening of the small arteries and the arterioles characterized by arterial wall thickening and loss of elasticity.
What is the Pathology of Arteriosclerosis?
The pathology of arteriosclerosis is:
-Etiology: The cause of arteriosclerosis is modifiable and non-modifiable genetic abnormalities, family history, increasing age male gender, hyperlipidemia, hypertension, diabetes, obesity, cigarette smoking, and inflammation.
-Genes involved: NA.
-Pathogenesis: The sequence of events that lead to arteriosclerosis are endothelial injury leading to increased permeability, leukocyte adhesion, and thrombosis later accumulation of in the vessel wall leading to platelet adhesion. Monocyte adhesion to the endothelium, migration into the intima, and differentiation into macrophages and foam cells ensues. Lipid accumulation within the macrophages stimulates inflammatory cytokine release which enduces smooth muscle cell proliferation.
-Morphology: The morphology associated with arteriosclerosis shows intimal lesions containing plaques filled, fibrous cap with smooth muscle cells, macrophages, and fatty streaks.
-Histology: The histology associated with arteriosclerosis shows abnormal arterial lumens that may be partially obstructed by plaque with intimal wall thickening.
How does Arteriosclerosis Present?
Patients with arteriosclerosis typically are older males. The symptoms, features, and clinical findings associated with are not seen but they occur once the plague is dislodged or ruptured.
How is Arteriosclerosis Diagnosed?
Arteriosclerosis is diagnosed arteriogram, lipid profile tests, chest x-rays, echocardiogram, and the exercise stress test.
How is Arteriosclerosis Treated?
Arteriosclerosis is treated by a change of lifestyle, healthy diet, exercise, anticoagulants, angioplasty, and potentially coronary stent placement.
What is the Prognosis of Arteriosclerosis?
The prognosis of arteriosclerosis depends on the location and degree of arteriosclerosis.
What is Monckeberg Medial Sclerosis?
Monckeberg medial sclerosis is the calcification of the tunica media of large and medium-sized muscular arteries.
What is the Pathology of Monckeberg Medial Sclerosis?
The pathology of Monckeberg medial sclerosis is:
-Etiology: The cause of Monckeberg medial sclerosis is the deposition of calcium salts.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to monckeberg medial sclerosis is not fully known, but factors like advancing in age and chronic renal diseases lead to sclerosis.
-Morphology: The morphology associated with monckeberg medial sclerosis shows pipestem-like rigid tubes without causing narrowing of the lumen.
-Histology: The histology associated with Monckerberg medial sclerosis shows calcium salts deposition in the tunica media.
How does Monckeberg Medial Sclerosis Present?
Patients with Monckeberg medial sclerosis are typically males that present at the age of around 50 years old. The symptoms, features, and clinical findings associated with Monckeberg medial sclerosis include ulcer formation, heart attacks, stroke, and medial mesenteric occlusions.
How is Monckerberg Medial Sclerosis Diagnosed?
Monckerberge medial sclerosis is diagnosed by ultrasound, x-rays, and ankle-brachial plexus index.
How is Monckerberg Medial Sclerosis Treated?
Mokerberge medial sclerosis is treated with low doses of vitamin D, calcimimetics, and magnesium biphosphate.
What is the Prognosis of Mokergberg Medial Sclerosis?
The prognosis of Monckerberg medial sclerosis is fair.
What Is Atherosclerosis?
Atherosclerosis is the hardening and thickening of the large arteries due to the presence of fatty plaques in the arteries. Modifiable risk factors for atherosclerosis include diabetes, hyperlipidemia, hypertension, and smoking.
What is the Pathology of Atherosclerosis?
The pathology of atherosclerosis is:
-Etiology: The cause of atherosclerosis is can be modifiable or non-modifiable, and these are the significant risk factors cause there is no specific cause of atherosclerosis include obesity, genetics, age, gender, and many others.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to atherosclerosis has two theories. The Reaction-to-injury hypothesis, and the monoclonal theory. Reaction to injury shows that damage to the endothelial cells causes adherence of the platelets to the affected area, and smooth muscle cells are formed driving the growth of new vessels. The monoclonal theory shows that the formation of new cells is caused by mutation due to the presence of substances that lead to the formation of new cells.
-Morphology: The morphology associated with atherosclerosis shows intimal thickening, fatty streaks, gelatinous lesions.
-Histology: The histology associated with atherosclerosis shows closely-packed foam cells, lipid-containing elongated smooth muscle.
How does Artherosclerosis Present?
Patients with atherosclerosis typically are males present at the age range of 20 years and above. The symptoms, features, and clinical findings associated with atherosclerosis often occur when the plaque dislodges or ruptures and it may lead to stroke, chest pain angina pectoris, slurred speech.
How is Artherosclerosis Diagnosed?
Artherosclerosis is diagnosed by chest x-ray, angiogram, lipid profile tests, doppler sounds, blood tests, stress tests.
How is Artherosclerosis Treated?
Artherosclerosis is treated by anticoagulants, statins, antihypertensives, angioplasty, stent placement, fibrinolytic therapy, coronary artery bypass surgery.
What is the Prognosis of Atherosclerosis?
The prognosis of atherosclerosis is fair and if it is noted early there are good recovery chances but if it is noted late it can lead to death.
What are Aneurysms?
Aneurysms are abnormal dilation of blood vessels that are permanent and are caused by weakening or injury to the blood vessels and can be congenital or acquired.
Examples of aneurysms include:
- Berry aneurysms
- Abdominal aortic aneurysm
- Thoracic aortic aneurysm
What are Berry Aneurysms?
Berry aneurysms have weakened blood vessels that are mostly located in the circle of willis at the base of the brain.
What is the Pathology of Berry Aneurysms?
The pathology of berry aneurysms is:
-Etiology: The cause of berry aneurysms is the thickening of the walls of the blood vessels caused by smoking, hypertension, old age over 40 years, and familial inheritance.
-Genes involved: Unknown.
Pathogenesis: The sequence of events that lead to berry aneurysms results from the outpouchings in the blood vessel wall due to genetic factors and/or acquired illness.
-Morphology: The morphology associated with berry aneurysms are saccular, bright red with a shiny surface and a thin translucent wall, and are 2mms to 2cm.
-Histology: The histology associated with berry aneurysms shows dilated vessels.
How does Berry Aneurysms Present?
Patients with berry aneurysms are typically female at the age range of young adulthood to middle age. The symptoms, features, and clinical findings associated with berry aneurysms are blurred vision, drooping eyelids, weakness, or pain behind the eye. When they rupture, they cause severe headache, stiff neck, confusion, increased intracranial pressure coma and may lead to death.
How is Berry Aneurysms Diagnosed?
Berry aneurysms are diagnosed history taking and physical examination, CT scan, angiography.
How is Berry Aneurysms Treated?
Berry aneurysms are treated by endovascular coiling, surgical clipping.
What is the Prognosis of Berry Aneurysms?
The prognosis of berry aneurysms is poor if it ruptures because on sustains a permanent neurological deficit.
What is an Abdominal Aortic Aneurysm?
An abdominal aortic aneurysm is a permanent localized dilatation of the abdominal aorta.
What is the Pathology of Abdominal Aortic Aneurysm?
The pathology of an abdominal aortic aneurysm is:
-Etiology: The cause of an abdominal aortic aneurysm is smoking, hypertension, advanced age, inflammation.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to the abdominal aortic aneurysm is after an inflammatory process, there is the breakdown of the elastic elements of the blood vessels that cause it to weaken and dilatation occurs due to the weakness of the blood vessels.
-Morphology: The morphology associated with abdominal aortic aneurysm shows dilated blood vessels that are more than 30 mm.
-Histology: Abnormal aortic vessel.
How does Abdominal Aortic Aneurysm Present?
Patients with abdominal aortic aneurysms are typically males at the age range of 60 years old. The symptoms, features, and clinical findings associated with abdominal aortic aneurysm include lower leg tingling, abnormal abdominal sounds.
How is Abdominal Aortic Aneurysm Diagnosed?
An abdominal aortic aneurysm is diagnosed by clinical presentation, physical examination, and ultrasound.
How is Abdominal Aortic Aneurysm Treated?
An abdominal aortic aneurysm is treated by open surgery, endovascular stent grafting, and close follow-up.
What is the Prognosis of Abdominal Aortic Aneurysm?
The prognosis of abdominal aortic aneurysm is poor if diagnosed late due to the high chances of rupture, but it has a good prognosis after treatment if diagnosed early.
What is a Thoracic Aortic Aneurysm?
Thoracic aortic aneurysm is a weakening of the upper part of the aorta.
What is the Pathology of Thoracic Aortic Aneurysm?
The pathology of thoracic aortic aneurysm is:
-Etiology: The cause of a thoracic aortic aneurysm is advanced age, genetics, smoking, hypertension, trauma, and mostly atherosclerosis.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to a thoracic aortic aneurysm depends on whether it is the ascending or the descending aorta. The ascending aorta sclerosis causes the aneurysm formation while the descending aortic aneurysm is caused by atherosclerosis.
-Morphology: Unknown.
-Histology: Abnormal aortic vasculature.
How does Thoracic Aortic Aneurysm Present?
Patients with thoracic aortic aneurysms are typically male at the age range of 50-70 years old. The symptoms, features, and clinical findings associated with thoracic aortic aneurysms include back pain, hemoptysis, hematemesis
How is Thoracic Aortic Aneurysm Diagnosed?
A thoracic aortic aneurysm is diagnosed by chest x-ray, MRI, ECG, echo, CT contrast, ascending g aortogram, and contrast angiography.
How is Thoracic Aortic Aneurysm Treated?
Thoracic aortic aneurysms are treated by management of the symptoms, smoking cessation, control of the modifiable risk factors, Dacron graft, or other stent-graft.
What is the Prognosis of Thoracic Aortic Aneurysm?
The prognosis of a thoracic aortic aneurysm is poor if rupturing occurs but generally has a survival rate of 1 year if it is not treated early.
What is an Aortic Dissection?
An aortic dissection is an accumulation of blood in between the wall of the aorta and the blood in between can travel and spread longitudinally.
What is the Pathology of Aortic Dissection?
The pathology of aortic dissection is:
-Etiology: The cause of aortic dissection is uncontrolled high blood pressure, aortic aneurysm, atherosclerosis, aortic valve defects, and aortic coarctation.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to aortic dissection are inflammation of the aortic wall that triggers apoptosis of the smooth muscles of the blood vessels, aortic media degeneration, disruption of the elastin fibers, and finally, dissection occurs.
-Morphology: The morphology associated with aortic dissection shows the presence of blood in between the walls of the blood vessels.
-Histology: Abnormal aortic tissue that is ruptured and hemorrhagic.
How does Aortic Dissection Present?
Patients with aortic dissection typically are both male and present at the age range of reproductive years in females while in the male it is at the age of 60 years. The symptoms, features, and clinical findings associated with aortic dissection include severe chest pain, neck or jaw pain, cerebral vascular accident, dyspnea, hemoptysis, and dysphagia.
How Is Aortic Dissection Diagnosed?
Aortic dissection is diagnosed by history and physical examination, electrocardiography, complete blood count, chest radiography, MRI,
How is Aortic Dissection Treated?
Aortic dissection is treated by endovascular repair, antihypertensives, pain management, and placement of a dacron graft.
What is the Prognosis of Aortic Dissection?
The prognosis of aortic dissection is poor since it has a high mortality rate because diagnosis is often made when reprinted has occurred, and the damage is irreparable.
What is Vasculitis?
Vasculitis is inflammation of the walls of the blood vessels.
Examples of vasculitis include:
- Infectious vasculitis
- Noninfectious vasculitis
What is infectious vasculitis?
Infectious vasculitis is inflammation of the walls of the blood vessels caused by direct infection, bacterial infection, and viral infection.
What is the Pathology of Infectious Vasculitis?
The pathology of infectious vasculitis is:
-Etiology: The cause of infectious vasculitis is a bacterial infection mostly aspergillus and the mucor species.
-Genes involved: NA.
-Pathogenesis: The sequence of events that lead to infectious vasculitis is triggered by immune complex deposition, antineutrophilic cytoplasmic antibodies, and also anti-endothelial cells antibodies.
-Morphology: NA.
-Histology: Infected vasculature.
How does Infectious Vasculitis Present?
Patients with infectious vasculitis typically affect men and children present at the age range of 50 years old. The symptoms, features, and clinical findings associated with infectious vasculitis include headache, fever, weight loss, fatigue, and general malaise.
How Infectious Vasculitis Diagnosed?
Infectious vasculitis is diagnosed complete blood count, erythrocyte sedimentation rate, liver function tests, chest radiography, urinalysis.
How is Infectious Vasculitis Treated?
Infectious vasculitis may be treated by corticosteroids and surgery.
What is the Prognosis of Infectious Vasculitis?
The prognosis of infectious vasculitis is good if treated properly and quickly.
What is Noninfectious Vasculitis?
Noninfectious vasculitis is autoimmune disorders-causing vascular inflammations.
Examples of noninfectious vasculitis include:
- Antiendothelial Cell Antibodies Vasculitis
- Antineutrophil Cytoplasmic Antibodies Vasculitis
- Behcet Disease
- Churg-Strauss Syndrome
- Immune Complex-Associated Vasculitis
- Giant Cell (Temporal) Arteritis
- Granulomatosis with Polyangiitis
- Kawasaki Disease
- Microscopic Polyangiitis
- Polyarteritis Nodosa
- Takayasu Arteritis
- Thromboangiitis Obliterans (Buerger Disease)
What is Antiendothelial Cell Antibodies Vasculitis?
Antiendothelial cell antibodies vasculitis is an inflammatory disease caused by the reaction of the antibodies to the endothelial cells.
What is the Pathology of Anti endothelial cell Antibodies Vasculitis?
The pathology of anti endothelial cell antibodies vasculitis is:
-Etiology: The cause of anti endothelia ell antibodies vasculitis is not very clear.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to anti endothelial cell antibodies vasculitis Autoantibodies
against endothelial antigens in circulation the adhesiveness of leucocytes to endothelial cells.
-Morphology: Unknown.
-Histology: Abnormal vasculature.
How does Anti Endothelial Cell Antibodies Vasculitis Present?
Patients with anti endothelial cell antibodies vasculitis are typically females around 40 years old. The symptoms, features, and clinical findings associated with anti endothelial cells antibodies vasculitis include hypertension and fatigue.
How is Anti Endothelial Cells Antibodies Vasculitis Diagnosed?
Anti endothelial cells antibodies are diagnosed in blood tests and imaging.
How is Anti Endothelial Cells Antibodies Vasculitis Treated?
Anti endothelial cells vasculitis is treated by glucocorticoids.
What is the Prognosis of Antiendothelial Cell Antibodies Vasculitis?
The prognosis of anti endothelial cell antibodies vasculitis is poor.
What is Antineutrophil Cytoplasmic Antibodies Vasculitis?
Antineutrophil cytoplasmic antibodies vasculitis is an autoimmune disease of the small blood vessels that are directed to the damage of certain proteins in the blood vessels.
What is the Pathology of Antineutrophilic Cytoplasmic Antibodies Vasculitis?
The pathology of antineutrophilic cytoplasmic antibodies vasculitis is:
-Etiology: The cause of anti-neutrophilic cytoplasmic antibodies vasculitis is the presence of the antibodies.
-Genes involved: HLA genes.
-Pathogenesis: The sequence of events that lead to antineutrophilic cytoplasmic antibodies vasculitis is not known but two mechanisms are involved. theory of molecular mimicry and the theory of defective apoptosis.
-Morphology: The morphology associated with anti-neutrophilic cytoplasmic antibodies shows pauci-immune necrotizing crescentic glomerulonephritis.
-Histology: Vasculature with proteinaceous deposition.
How does Anti-neutrophilic Cytoplasmic Antibodies Present?
Patients with anti-neutrophilic cytoplasmic antibodies typically are middle aged adults. The symptoms, features, and clinical findings associated with anti-neutrophilic cytoplasmic antibodies include proteinuria, hematuria, high blood pressure, fatigue, respiratory failure, tracheal inflammation.
How are Anti-neutrophilic Cytoplasmic Antibodies Diagnosed?
Anti-neutrophilic cytoplasmic antibodies are diagnosed by microscopy, urinalysis, kidney function tests, creatinine levels, and blood tests.
How is Anti-neutrophilic Cytoplasmic Antibodies Treated?
Anti-neutrophilic cytoplasmic antibodies are treated by glucocorticoids, cyclophosphamides, plasma exchange therapy.
What is the Prognosis of Anti-neutrophilic Cytoplasmic Antibodies?
The prognosis of antineutrophilic cytoplasmic antibodies is poor since it has a high mortality rate of 90%
What is Behcet Disease?
Behcet disease is a form of vasculitis that is chronic, a relapsing-remitting disease characterized by urogenital, uveitis, and oral ulceration.
What is the Pathology of Behcet’s Disease?
The pathology of Behcet’s disease is:
-Etiology: The cause of behcet’s disease is not fully known but there is the involvement of the immune system where it starts to attack its cells.
-Genes involved: HLA-B51, HLA-B5.
-Pathogenesis: The sequence of events that lead to behcet’s disease is not fully understood bit like that cause there is an autoimmune involvement where the body attacks its cells.
-Morphology: NA.
-Histology: The histology associated with behcet’s disease depends on the type of lesion involved. It can show dense neutrophilic infiltration, perivascular lymphocytic infiltration, lymphocytes and macrophages, and also T-cell populations.
How does Behcet Disease Present?
Patients with Behcet’s disease typically males between 20-50 years old. The symptoms, features, and clinical findings associated with Behcet’s disease include oral lesions, ocular lesion, urogenital lesions, and cutaneous lesions.
How is Behcet Disease Diagnosed?
Behcet disease is diagnosed physical examination, chest x-ray, ESR, rheumatoid factor.
How is Behcet Disease Treated?
Behcet disease is treated according to the symptoms presented by intravenous immunosuppressants, corticosteroids, and anticoagulants in case of thrombosis.
What is the Prognosis of Behcet Disease?
The prognosis of behcet’s disease is fair due to its low mortality rate. There is however a risk of blindness.
What is Churg-Strauss Syndrome?
Churg-Strauss Syndrome is a disease of inflamed blood vessels.
What is the Pathology of Churg-Strauss Syndrome?
The pathology of churg-strauss syndrome is:
-Etiology: The cause of Churg-Strauss syndrome is not fully known but the factors that can accelerate the occurrence are gene mutation and environmental factors.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to churg-strauss syndrome is not known for now but it is associated with granuloma formation, eosinophilia infiltration.
-Morphology: NA.
-Histology: The histology associated with Churg-Strauss shows tissue eosinophilia, extravascular granulomas,
How does Churg-Strauss Syndrome Present?
Patients with Churg-Strauss syndrome typically are females above 40 years old. The symptoms, features, and clinical findings associated with Churg-Strauss syndrome are weight loss due to appetite loss, joint and muscle pain, GIT bleeding and abdominal pain, rash and skin sores, tingling sensation on your hands, and feet, fever, and malaise.
How is Churg-Strauss Syndrome Diagnosed?
Churg-Strauss syndrome is diagnosed by blood tests, imaging, a biopsy of the affected tissue and erythrocyte sedimentation rate levels.
How is Churg-Strauss Syndrome Treated?
Churg-Strauss syndrome is treated by immunosuppressors and corticosteroids.
What is the Prognosis of Churg-Strauss Syndrome?
The prognosis of Churg-Strauss syndrome is fair because the survival rate increases when one undergoes treatment.
What is Immune Complex-Associated Vasculitis?
Immune complex-associated vasculitis is a disease that occurs as a result of the accumulation of the immune complexes in the blood vessels causing them to become inflamed it’s mostly seen in immunological disorders.
What is the Pathology of Immune Complex- Associated Vasculitis?
The pathology of immune complex-associated vasculitis is:
-Etiology: The cause of immune complex-associated vasculitis may be due to an infection, medication, autoimmune disorders,
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to immune complex-associated vasculitis accumulates the immunoglobulins in the blood vessels.
-Morphology: NA.
-Histology: The histology associated with immune complex-associated vasculitis is the presence of infiltrating leucocytes and fibrinoid necrosis.
How does Immune Complex-Associated Vasculitis Present?
Patients with immune complex-associated vasculitis typically are males. The symptoms, features, and clinical findings associated with immune complex-associated vasculitis include palpable purpura which are cutaneous palpable lesions in the lower extremities,
How is Immune Complex-Associated Vasculitis Diagnosed?
Immune complex-associated vasculitis is diagnosed with x-rays, CT-scan, ultrasounds, and MRI.
How is Immune Complex-Associated Vasculitis Treated?
Immune complex-associated vasculitis is treated through corticosteroids and immunosuppressors.
What is the Prognosis of Immune Complex-Associated Vasculitis?
The prognosis of immune complex-associated vasculitis is good since it has a low mortality rate and one can recover in months.
What is Giant Cell Arteritis?
Giant cell (temporal) arteritis is a disease caused by the T-ell immune response that affects the large temporal arteries characterized by inflammation.
What is the Pathology of Giant Cell Arteritis?
The pathology of giant cell (temporal) arteritis is:
-Etiology: The cause of Giant Cell (Temporal) Arteritis is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to giant cell (temporal) arteritis is not well known but it is characterized by intimal hyperplasia and luminal obstruction leading to ischemia and finally swelling of the blood vessels occurs.
-Morphology: The morphology associated with giant cell (temporal) arteritis shows nodular intimal thickening, lymphocytes, and macrophages, with multinucleated giant cells
-Histology: The histology associated with giant cell (temporal) arteritis shows thickened intima, laminal necrosis, giant cells, and lumen occlusion.
How does Giant Cell (Temporal) Arteritis Present?
Patients with giant cell (temporal) arteritis typically are females present at the age range of 65-80 years. The symptoms, features, and clinical findings associated with the giant cell (temporal) arteritis include headache, tenderness of the scalp, anorexia, weight loss, fatigue, tongue claudication anemia, fever, diplopia, enlarged blood vessels.
How is Giant Cell (Temporal) Arteritis Diagnosed?
Giant cell (temporal) arteritis is diagnosed with a biopsy, ESR, ultrasound, and doppler.
How is Giant Cell (Temporal) Arteritis Treated?
Giant cell (temporal) arteritis is treated with steroids, prednisolone.
What is the Prognosis of Giant Cell (Temporal) Arteritis?
The prognosis of giant cell temporal arteritis is good since they respond well to treatment. However, there is a chance of vision loss.
What is Granulomatosis with Polyangiitis?
Granulomatosis with polyangiitis is also known as inflammation of the blood vessels and the most affected blood vessels are those in the ears, lungs, kidneys, nose, and throat. Granulomatosis with polyangiitis is also known as Wegener’s granulomatosis with necrotizing vasculitis.
What is the Pathology of Granulomatosis with Polyangiitis?
The pathology of granulomatosis with polyangiitis is:
-Etiology: The cause of granulomatosis with polyangiitis is unknown but there is the involvement of anti-neutrophilic cytoplasmic antibodies.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to granulomatosis with polyangiitis is not fully understood
-Morphology: NA.
-Histology: The histology associated with granulomatosis with polyangiitis shows multinucleated giant cells, segmental necrotizing lesions, with crescent formation.
How does Granulomatosis with Polyangiitis Present?
Patients with granulomatosis with polyangiitis typically are both males and present at the age range of 40-60 years old. The symptoms, features, and clinical findings associated with granulomatosis with polyangiitis include fever, weight loss, asthenia, sinusitis, chronic otitis media alveolar hemorrhage, and saddle nose deformity.
How is Granulomatosis with Polyangiitis Diagnosed?
Granulomatosis with polyangiitis is diagnosed by biopsy, chest radiography, urinalysis, physical examination, and ANCA assay.
How is Granulomatosis with Polyangiitis Treated?
Granulomatosis with polyangiitis is treated by immunosuppressors, plasma exchange, corticosteroids, and cytotoxic agents.
What is the Prognosis of Granulomatosis with Polyangiitis?
The prognosis of granulomatosis with polyangiitis is poor.
What is Kawasaki Disease?
Kawasaki disease is also known as mucocutaneous lymph node syndrome. Kawasaki disease is an acute illness characterized by inflammation of blood vessels in the whole body.
What is the Pathology of Kawasaki Disease?
The pathology of kawasaki disease is:
-Etiology: The cause of kawasaki disease is unknown but the possible causes considered are infectious, genetic, toxic, and immunological factors.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to Kawasaki disease is not known but there is the involvement of the immunopathologic mechanism after the inflammatory process has occurred
-Morphology: The morphology associated with Kawasaki disease shows a dense accumulation of macrophages and
-Histology: The histology associated with Kawasaki disease shows lymphocytes and mononuclear cells, pustules with small intraepidermal, edema of the papillary dermis, and subcorneal abscesses.
How does Kawasaki Disease Present?
Patients with Kawasaki disease typically are pediatric males. The symptoms, features, and clinical findings associated with Kawasaki disease include abnormal appearing tounge, skin rashes, rhinorrhea, vomiting, diarrhea, arthritis, arthralgia, and irritability.
How is Kawasaki Disease Diagnosed?
Kawasaki disease is diagnosed using electrocardiograph, chest x-ray, and physical examination.
How is Kawasaki Disease Treated?
Kawasaki disease is treated by Asprin and the dosage depends on the stage of the disease.
What is the Prognosis of Kawasaki Disease?
The prognosis of Kawasaki disease is fair since the treated child can recover in ten days.
What is Microscopic Polyangiitis?
Microscopic polyangiitis is another form of necrotizing vasculitis that generally affects capillaries, as well as small arterioles and venules.
What is the Pathology of Microscopic Polyangiitis?
The pathology of microscopic polyangiitis is:
-Etiology: The cause of microscopic polyangiitis is not well understood but there is the involvement of the inflammatory response.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to microscopic polyangiitis is not well known but there is the involvement of ANCA which is an autoimmune response
-Morphology: NA.
-Histology: The histology associated with microscopic polyangiitis shows segmental fibrinoid necrosis, focal transmural necrotizing lesions; granulomatous inflammation is absent.
How does Microscopic Polyangiitis Present?
Patients with microscopic polyangiitis typically are males that present at the age range of 50 years old. The symptoms, features, and clinical findings associated with microscopic polyangiitis include hemoptysis, hematuria, proteinuria, abdominal pain or bleeding, muscle pain or weakness, and palpable cutaneous purpura.
How is Microscopic Polyangiitis Diagnosed?
Microscopic polyangiitis is diagnosed by physical examination, renal function tests, chest radiography, GIT endoscopy.
How is Microscopic Polyangiitis Treated?
Microscopic polyangiitis is treated with corticosteroids, immunosuppressors, and intravenous immunoglobulin.
What is the Prognosis of Microscopic Polyangiitis?
The prognosis of microscopic polyangiitis is good since it has a reasonable survival rate of 90%.
What is Polyarteritis Nodosa?
Polyarteritis nodosa is a necrotizing and systemic vasculitis relating to multiple organs and tissues’ small and medium-sized muscular arteries.
What is the Pathology of Polyarteritis Nodosa?
The pathology of polyarteritis nodosa is:
-Etiology: The cause of polyarteritis nodosa is genetic factors, other conditions such as hepatitis B.
-Genes involved: CECR1(ADA2).
-Pathogenesis: The sequence of events that lead to polyarteritis nodosa are not well known. Believed to be due to Inflammation of the medium-sized muscular arteries. Originate at the vessel, intima progresses to comprise the whole arterial wall, destroying the entire elastic lamina, resulting in fibrinoid necrosis, aneurysms, and sometimes thrombi.
-Morphology: The morphology associated with polyarteritis nodosa shows necrotizing inflammation of arteries.
-Histology: The histology associated with polyarteritis nodosa shows neutrophils, eosinophils, and mononuclear cells present at the site of the lesion.
How does Polyarteritis Nodosa Present?
Patients with polyarteritis nodosa typically affect men more often than women present at an age range of 20 to 40. The symptoms, features, and clinical findings associated with polyarteritis nodosa include fever of unknown cause, malaise, weight loss, bloody stool, abdominal pain, and hypertension.
How is Polyarteritis Nodosa Diagnosed?
Polyarteritis nodosa is diagnosed through the clinical presentation. Imaging studies- angiography disclose stenoses and larger aneurysms. Laboratory studies- establish the systemic nature of the condition, elevated ESR, Hepatitis B surface antigen test, proteinuria.
How is Polyarteritis Nodosa Treated?
Polyarteritis nodosa is treated through medical care, corticosteroid therapy, cyclophosphamide therapy.
What is the Prognosis of Polyarteritis Nodosa?
The prognosis of polyarteritis nodosa is good in cutaneous PAN without systemic involvement.
What is Takayasu Arteritis?
Takayasu arteritis is a granulomatous vasculitis affecting the medium and larger arteries.
What is the Pathology of Takayasu Arteritis?
The pathology of takayasu arteritis is:
-Etiology: The cause of takayasu arteritis is unknown.
-Genes involved: HLA haplotype A24-B52-DR2.
-Pathogenesis: The sequence of events that lead to takayasu arteritis are unknown.
-Morphology: The morphology associated with takayasu arteritis shows asymmetrical thickening of the aortic.
-Histology: The histology associated with takayasu arteritis shows mononuclear inflammation.
How does Takayasu Arteritis Present?
Patients with takayasu arteritis typically common in female present at age range of below 40 years. The symptoms, features, and clinical findings associated with takayasu arteritis include upper extremity weaker pulses, low blood pressure, ocular disturbances, finger numbness, and neurological defects.
How is Takayasu Arteritis Diagnosed?
Takayasu arteritis is diagnosed through clinical presentation. Imaging studies may show arteriographic narrowing.
How is Takayasu Arteritis Treated?
Takayasu arteritis is treated through medical care such as corticosteroid therapy, cytotoxic agents, and biologic agents such as tocilizumab.
What is the Prognosis of Takayasu Arteritis?
The prognosis of takayasu arteritis is fair with a five-year survival rate of 60%.
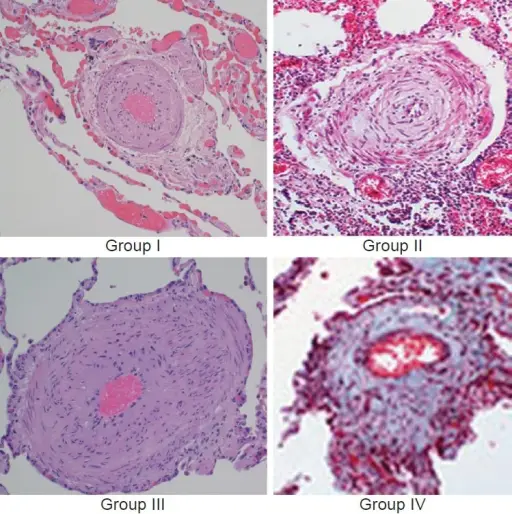
What is Thromboangiitis Obliterans?
Thromboangiitis obliterans aka Buerger disease is an inflammatory vasculopathy, leading to vascular inadequacy.
What is the Pathology of Thromboangiitis Obliterans?
The pathology of thromboangiitis obliterans (Buerger disease) is:
-Etiology: The cause of thromboangiitis obliterans (buerger disease) is related to tobacco use.
-Genes involved: HLA-A9 and HLA-B5.
-Pathogenesis: The sequence of events that lead to thromboangiitis obliterans (buerger disease) is as the result of immunologic spectacle leading to vasodysfunction as well as inflammatory thrombi.
-Morphology: The morphology associated with thromboangiitis obliterans (buerger disease) shows vasculitis of medium-sized and small arteries.
-Histology: The histology associated with thromboangiitis obliterans (buerger disease) shows polymorphonuclear leukocyte (PMN)-predominant inflammatory cellular.
How does Thromboangiitis Obliterans Present?
Patients with thromboangiitis obliterans (Buerger disease) are typically males that smoke. The symptoms, features, and clinical findings associated with thromboangiitis obliterans (buerger disease) include distal digit frank gangrene, ischemic rest pain, leg/feet and arms claudication. And feet infection.
How is Thromboangiitis Obliterans Diagnosed?
Thromboangiitis obliterans (buerger disease) is diagnosed through imaging studies- Arteriography shows nonatherosclerotic, segmental occlusive lesions.
How is Thromboangiitis Obliterans Treated?
Thromboangiitis obliterans (Buerger disease) is treated through cessation of tobacco use, hyperbaric oxygen therapy, pharmacologic therapy- iloprost, oral NSAIDs, narcotic analgesics, and potentially surgical care such as revascularization, and sympathectomy.
What is the Prognosis of Thromboangiitis Obliterans?
The prognosis of thromboangiitis obliterans (Buerger disease) is good, with death from the condition being rare.
What are Disorders of Blood Vessels?
Disorders of blood vessels are the conditions of the vessels that affect their structure and functionality.
Examples of disorders of blood vessel include:
- Raynaud phenomenon
- Myocardial vessel vasospasm
What is Raynaud Phenomenon?
Raynaud phenomenon is paroxysmal pallor or cyanosis and vasospasm to the fingers and toes and usually occurs in response to stress or cold exposure.
What is the Pathology of Raynaud Phenomenon?
The pathology of raynaud phenomenon is:
-Etiology: The cause of raynaud phenomenon is unknown, cold exposure association.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to raynaud phenomenon is unknown associated with cold exposure.
-Morphology: The morphology associated with raynaud phenomenon shows pallor, cyanosis and hyperemia of the digit.
-Histology: Vasculature abnormality.
How does Raynaud Phenomenon Present?
Patients with raynaud phenomenon typically slightly higher in females at age range of 14 years old. The symptoms, features, and clinical findings associated with raynaud phenomenon include pain and numbness, pallor, cyanosis, hyperemia, digital ulcers, and calcinosis cutis.
How is Raynaud Phenomenon Diagnosed?
Raynaud phenomenon is diagnosed through clinical presentation. Imaging studies- MRI arteriography, thermography, and isotope studies. Laboratory tests such as CBC count, BUN, creatine level, prothrombin time, and activated partial thromboplastin time.
How is Raynaud Phenomenon Treated?
Raynaud phenomenon is treated through education, cessation of vasoconstricting agents. Pharmacologic therapy such as prostacyclin analogs and calcium channel blockers.
What is the Prognosis of Raynaud Phenomenon?
The prognosis of raynaud phenomenon is good.
What is Myocardial Vessel Vasospasm?
Myocardial vessel vasospasm is a blood vessel disorder characterized by extreme constriction of arteries or arterioles that may cause ischemia.
What is the Pathology of Myocardial Vessel Vasospasm?
The pathology of myocardial vessel vasospasm is:
-Etiology: The cause of myocardial vessel vasospasm is idiopathic.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to myocardial vessel vasospasm unknown.
-Morphology: Unknown.
-Histology: NA.
How does Myocardial Vessel Vasospasm Present?
Patients with myocardial vessel vasospasm typically common in males present at age range of 50-years-old. The symptoms, features, and clinical findings associated with myocardial vessel vasospasm include retrosternal pain, arrhythmias, rales, peripheral edema, jugular venous distention and extra heart sounds.
How is Myocardial Vessel Vasospasm Diagnosed?
Myocardial vessel vasospasm is diagnosed through laboratory studies-serum chemistry, lipid profiles and magnesium levels imaging, echocardiography, perfusion imaging. Coronary angiography shows central spasm.
How is Myocardial Vessel Vasospasm Treated?
Myocardial vessel vasospasm is treated through medical therapy nitrate therapy, calcium channel blockers. Surgical intervention includes percutaneous surgical revascularization.
What is the Prognosis of Myocardial Vessel Vasospasm?
The prognosis of myocardial vessel vasospasm is fair, with significant morbidity but low mortality.
What are Vein Abnormalities?
Vein abnormalities are the pathology of the venous system affecting their function and structure.
Examples of vein abnormalities include:
- Varicose veins
- Phlebothrombosis
- Thrombophlebitis
- Vena cava syndromes
What are Varicose Veins?
Varicose veins are tortuous and permanently dilated superficial veins of the lower extremities.
What is the Pathology of Varicose Veins?
The pathology of varicose veins is:
-Etiology: The cause of varicose veins is familial factors, venous hypertension, hormonal effects on smooth muscle, obesity, chronic constipation.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to varicose veins are as a result of familial tendency toward premature varicosities, increased venous pressures leading to venous stasis, and pedal edema
-Morphology: The morphology associated with varicose veins shows dilated, tortuous,
elongated and nodular of the affected vein.
-Histology: The histology associated with varicose veins shows inconstant fibromuscular thickening of the vein wall.
How does Varicose Veins Present?
Patients with varicose veins are typically older females. The symptoms, features, and clinical findings associated with varicose veins include thrombosis, congestion, pain, ulcerations, ill healing lesions and edema in the extremity.
How is Varicose Veins Diagnosed?
Varicose veins is diagnosed through medical therapy and surgical- stab phlebectomy, excision of small saphenous vein, and endovenous laser treatment.
How is Varicose Veins Treated?
Varicose veins is treated through physical exam and duplex ultrasonography.
What is the Prognosis of Varicose Veins?
The prognosis of varicose veins is good proper treatment arrests the progression of the condition.
What is Phlebothrombosis?
Phlebothrombosis is a clot occurrence within a vein, which is not related to the venous wall inflammation.
What is the Pathology of Phlebothrombosis?
The pathology of phlebothrombosis is:
-Etiology: The cause of phlebothrombosis is inactivity, malignancy, use of oestrogen-containing compounds, cardiac failure, and postoperative state.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to phlebothrombosis results from initiated triad of changes: endothelial injury, change in the composition of blood and venous stasis.
-Morphology: The morphology associated with phlebothrombosis shows affected area firm and distended.
-Histology: The histology associated with phlebothrombosis shows thick-walled fibrous vein.
How does Phlebothrombosis Present?
Patients with phlebothrombosis are typically females in there forties or above. The symptoms, features, and clinical findings associated with phlebothrombosis include distal edema, superficial vein dilation, heat, tenderness, redness, swelling, pain, and cyanosis.
How is Phlebothrombosis Diagnosed?
Phlebothrombosis is diagnosed through clinical presentations. Imaging such as venous duplex ultrasonography may be helpful.
How is Phlebothrombosis Treated?
Phlebothrombosis is treated through limited activity of the affected part, moist heat application. Medical therapy- anticoagulants and antibiotics.
What is the Prognosis of Phlebothrombosis?
The prognosis of phlebothrombosis is good in case of local effect of the condition and worse in case of systemic effects.
What is Thrombophlebitis?
Thrombophlebitis is formation and presence of a blood clot in the presence of inflammation of the venous wall and injury.
What is the Pathology of Thrombophlebitis?
The pathology of thrombophlebitis is:
-Etiology: The cause of thrombophlebitis is hereditary factor deficiency, is inactivity, malignancy, use of estrogen-containing compounds, cardiac failure, and the postoperative state.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to thrombophlebitis results from initiated triad of changes: endothelial injury, change in the composition of blood and venous stasis.
-Morphology: The morphology associated with thrombophlebitis shows affected area firm and distended.
-Histology: The histology associated with thrombophlebitis shows thick-walled fibrous, and vein, fibroblastic proliferation, and mononuclear inflammatory cells.
How does Thrombophlebitis Present?
Patients with thrombophlebitis are more commonly females, and the age range is 30 to 50 years old. The symptoms, features, and clinical findings associated with thrombophlebitis include distal edema, superficial vein dilation, heat, tenderness, redness, swelling, pain and cyanosis.
How is Thrombophlebitis Diagnosed?
Thrombophlebitis is diagnosed clinical presentation, CBC count, aPTT, prothrombin time, protein S level, and antithrombin level for evaluation of factor-related hypercoagulability. Imaging studies such as venous duplex ultrasonography may be helpful.
How is Thrombophlebitis Treated?
Thrombophlebitis is treated through medical care such as low molecular weight heparin, NSAID therapy. Surgical care may also be needed.
What is the Prognosis of Thrombophlebitis?
The prognosis of thrombophlebitis is good with proper management.
What are Vena Cava Syndromes?
Vena cava syndromes are due to compression of the vena cava.
Examples of vena cava syndromes include:
- Superior vena cava syndrome
- Inferior vena cava syndrome
What is Superior Vena Cava Syndrome?
Superior vena cava syndrome may be due to compression of the superior vena cava by a neoplasm.
What is the Pathology of Superior Vena Cava Syndrome?
The pathology of superior vena cava syndrome is:
-Etiology: The cause of superior vena cava syndrome is malignant mediastinal growths.
-Genes involved: NA.
-Pathogenesis: The sequence of events that lead to superior vena cava syndrome are as the result of consequent obstruction of superior vena cava by neoplastic invasion producing specific clinical manifestation.
-Morphology: Congested face.
-Histology: NA.
How does Superior Vena Cava Syndrome Present?
Patients with superior vena cava syndrome typically are males that present at an age range of 40 to 60 years old. The symptoms, features, and clinical findings associated with superior vena cava syndrome include cyanosis, head, arms, and neck vein dilatation.
How is Superior Vena Cava Syndrome Diagnosed?
Superior vena cava syndrome is diagnosed through imaging studies such as chest radiography, CT scan, MRI, and venography.
How is Superior Vena Cava Syndrome Treated?
Superior vena cava syndrome is treated through medical care which include chemotherapy, and oxygen supplementation. Surgical care may also be needed.
What is the Prognosis of Superior Vena Cava Syndrome?
The prognosis of superior vena cava syndrome is good. With proper management it is not associated with any mortality.
What is Inferior Vena Cava Syndrome?
Inferior vena cava syndrome is the condition caused by compression or invasion of the inferior vena cava wall and/or thrombus from iliac or femoral vein.
What is the Pathology of Inferior Vena Cava Syndrome?
The pathology of inferior vena cava syndrome is:
-Etiology: The cause of inferior vena cava syndrome is neoplasms, thrombus
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to inferior vena cava syndrome are as the result of consequent obstruction of inferior vena cava by neoplastic invasion and a thrombus producing the clinical manifestation.
-Morphology: Unknown.
-Histology: Unknown.
How does Inferior Vena Cava Syndrome Present?
Patients with inferior vena cava syndrome are typically more common in males within an age range of 40 to 60 years old. The symptoms, features, and clinical findings associated with inferior vena cava syndrome include edema of the leg, abdominal superficial collateral veins distension.
How is Inferior Vena Cava Syndrome Diagnosed?
Inferior vena cava syndrome is diagnosed through imaging studies such as chest radiography, CT scan, MRI, and venography.
How is Inferior Vena Cava Syndrome Treated?
Inferior vena cava syndrome is treated through medical care which may include chemotherapy and oxygen supplementation. Surgical care like a surgical bypass may be helpful.
What is the Prognosis of Inferior Vena Cava Syndrome?
The prognosis of inferior vena cava syndrome is good. With proper management, it is not associated with any mortality.
What are Lymphatic Abnormalities?
Lymphatic abnormalities are disorders affecting the lymphatic vessels, secondary development allied with cancer, and inflammation.
Examples of lymphatic abnormalities include:
- Lymphedema
- Lymphangitis
What is Lymphedema?
Lymphedema is an atypical protein-rich fluid collection in the interstitium resultant of obstruction of lymphatic drainage.
What is the Pathology of Lymphedema?
The pathology of lymphedema is:
-Etiology: The cause of lymphedema is tumors, associated with lymphatic system, surgical procedures severing lymphatic connections, and familiar factors.
-Genes involved: NA.
-Pathogenesis: The sequence of events that lead to lymphedema is a result of congenital peripheral lymphatics aplasia or hypoplasia or by valvular incompetence in case of primary lymphedema. Acquired blockade to the lymph nodes or by local lymphatic channels disturbance producing the clinical manifestation.
-Morphology: The morphology associated with lymphedema shows diffuse dermal edema.
-Histology: The histology associated with lymphedema shows hyperkeratosis, acanthosis, parakeratosis.
How does Lymphedema Present?
Patients with lymphedema are typically common in females. The symptoms, features, and clinical findings associated with lymphedema include, among others, swelling of the extremity, fatigue, fevers, daily activity impairment, recurrent cellulitis, microbial infection, and chills.
How is Lymphedema Diagnosed?
Lymphedema is diagnosed through the clinical presentation, physical examination. Laboratory studies-LFTs, BUN/Creatinine levels, urinalysis, and CBC count. Imaging studies such as plain radiographs, CT-scan, MRI-malignancy, ultrasonography may be helpful.
How is Lymphedema Treated?
Lymphedema is treated through medical care- pharmacotherapy benzopyrones, retinoidlike agents, anthelmintic agents, and antibiotics. Non-pharmacotherapy elevating affected limb, weight loss, avoiding trauma. Palliative surgical care.
What is the Prognosis of Lymphedema?
The prognosis of lymphedema is good.
What is Lymphangitis?
Lymphangitis is the lymphatic channels inflammation that arises due to distal site infection of the channel.
What is the Pathology of Lymphangitis?
The pathology of lymphangitis is:
-Etiology: The cause of lymphangitis is bacterial infection may include group A beta-hemolytic streptococci.
-Genes involved: NA.
-Pathogenesis: The sequence of events that lead to lymphangitis due to local inflammation and consequent infection. The infection or inflammation then spreads proximally to regional lymph nodes where the bacterial proliferate initiating a cascaded inflammatory process.
-Morphology: Unknown.
-Histology: Dilated lymphatic vessels.
How does Lymphangitis Present?
Patients with lymphangitis typically slightly higher in males present at age range of any age. The symptoms, features, and clinical findings associated with lymphangitis include erythematous, irregular linear streaks tender and warm, swollen and tender lymph node.
How is Lymphangitis Diagnosed?
Lymphangitis is diagnosed through the clinical presentation, blood culture, and CBC count, and imaging studies.
How is Lymphangitis Treated?
Lymphangitis is treated through medical therapy such as antimicrobial agent, anti-inflammatory, raise and immobilize affected areas.
What is the Prognosis of Lymphangitis?
The prognosis of lymphangitis is good with uncomplicated lymphangitis.
What are Vascular Tumors?
Vascular tumors are a spectrum from the benign hemangiomas, infrequently metastasized intermediate lesions, to fairly rare, highly malignant lesions.
Examples of vascular tumors include:
- Benign tumors and tumor-like lesions of the vasculature
- Borderline tumors of the vasculature
- Malignant tumors of the vasculature
What are Benign Tumors and Tumor-Like Lesions of the Vasculature?
Benign tumors and tumor-like lesions of the vasculature are neoplasms displaying endothelial cell differentiation, appearing to be resulting from cells that surround blood vessels.
Benign tumors and tumor-Like lesions of the vasculature include:
- Bacillary angiomatosis
- Hemangiomas
- Glomus tumor
- Lymphangiomas
- Vascular ectasias
What is Bacillary Angiomatosis?
Bacillary angiomatosis is an opportunistic ailment of immunocompromised persons displaying as vascular proliferations caused by Bartonella Henselae and Bartonella Quintana gram-negative bacilli.
What is Hemangioma?
Hemangioma is tumor acknowledged by speedy endothelial cell proliferation at early infancy, trailed by involution over time.
Examples of hemangiomas include:
- Capillary hemangiomas
- Cavernous hemangiomas
- Juvenile hemangiomas
- Pyogenic granulomas
What are Capillary Hemangiomas?
Capillary hemangiomas are the most common type of benign tumors composed of blood-filled vessels, mostly on the skin, subcutaneous tissues, oral cavities mucous membranes.
What is the Pathology of Capillary Hemangiomas?
The pathology of capillary hemangiomas is:
-Etiology: The cause of capillary hemangiomas is hamartomatous proliferations
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to capillary hemangiomas, thought to result from vascular endothelial cells hamartomatous propagations.
-Morphology: The morphology associated with capillary hemangiomas shows varying in size, bright red to blue, and slightly raised lesion.
-Histology: The histology associated with capillary hemangiomas shows lobulated, unencapsulated aggregates, and flattened endothelium.
How does Capillary Hemangiomas Present?
Patients with capillary hemangiomas are typically females more than males that are young. The symptoms, features, and clinical findings associated with capillary hemangiomas include red spot growing, ptosis eyelid.
How is Capillary Hemangiomas Diagnosed?
Capillary hemangiomas is diagnosed through laboratory studies such as positive factor VIII immunohistochemical staining. Imaging studies include ultrasonography indicates irregular lesion contour, CT scan, and MRI.
How is Capillary Hemangiomas Treated?
Capillary hemangiomas is treated through medical care such as corticosteroid therapy, propranolol therapy, interferon alfa therapy, and timolol therapy. Surgical care may also be useful.
What is the Prognosis of Capillary Hemangiomas?
The prognosis of capillary hemangiomas is good. Lesions may resolve on there own.
What are Cavernous Hemangiomas?
Cavernous hemangiomas are benign tumors composed of blood-filled vessels that are more infiltrative, often involving deep structures.
What is the Pathology of Cavernous Hemangiomas?
The pathology of cavernous hemangiomas is:
-Etiology: Unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to cavernous hemangiomas, thought to result from vascular endothelial cells hamartomatous propagations.
-Morphology: The morphology associated with cavernous hemangiomas shows a red-blue, soft, spongy mass 1 to 2 cm in diameter.
-Histology: The histology associated with cavernous hemangiomas shows unencapsulated, large cavernous blood-filled vascular spaces separated by connective tissue stroma.
How does Cavernous Hemangiomas Present?
Patients with cavernous hemangiomas are more commonly in females that present at an age range of 30 to 40 years old. The symptoms, features, and clinical findings associated with cavernous hemangiomas include painless, slowly advancing protrusion. Change of visual acuity in case of eye involvement, and diplopia.
How is Cavernous Hemangiomas Diagnosed?
Cavernous hemangiomas is diagnosed through imaging studies such as CT scan, and ultrasound.
How is Cavernous Hemangiomas Treated?
Cavernous hemangiomas is treated through surgical care for cosmetic purposes.
What is the Prognosis of Cavernous Hemangiomas?
The prognosis of cavernous hemangiomas is good. Most require no intervention.
What are Juvenile Hemangiomas?
Juvenile hemangiomas are benign vascular neoplasms with characteristic clinical progression manifested by early proliferation and then tailed by spontaneous involution.
What is the Pathology of Juvenile Hemangiomas?
The pathology of juvenile hemangiomas is:
-Etiology: The cause of juvenile hemangiomas is unknown.
-Genes involved: VEGFR1
-Pathogenesis: The sequence of events that lead to juvenile hemangiomas not well elucidated
-Morphology: The morphology associated with juvenile hemangiomas shows the quantity of fibrofatty tissue.
-Histology: The histology associated with juvenile hemangiomas shows nonencapsulated masses plump endothelial cells.
How does Juvenile Hemangiomas Present?
Patients with juvenile hemangiomas, typically females, are more affected than males present at birth to 9 years old. The symptoms, features, and clinical findings associated with juvenile hemangiomas include blanching of skin, red/crimson macule, shallow ulceration.
How is Juvenile Hemangiomas Diagnosed?
Juvenile hemangiomas is diagnosed through the clinical presentation, laboratory studies. Skin biopsy is diagnostic.
How is Juvenile Hemangiomas Treated?
Juvenile hemangiomas is treated through medical care such as propranolol and corticosteroid therapy. Surgical interventions such as laser surgery and surgical excision.
What is the Prognosis of Juvenile Hemangiomas?
The prognosis of juvenile hemangiomas is good.
What are Pyogenic Granulomas?
Pyogenic granulomas are polypoid type of capillary hemangioma arises as a swiftly growing exophytic red nodule attached by a stalk to the skin, gingival or oral mucosa.
What is the Pathology of Pyogenic Granulomas?
The pathology of pyogenic granulomas is:
-Etiology: The cause of pyogenic granulomas is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to pyogenic granulomas is vascular proliferation.
-Morphology: The morphology associated with pyogenic granulomas shows extensive edema, resemblance of exuberant granulation tissue.
-Histology: The histology associated with pyogenic granulomas shows inflammatory infiltrate.
How does Pyogenic Granulomas Present?
Patients with pyogenic granulomas typically more commonly males around 20 years old. The symptoms, features, and clinical findings associated with pyogenic granulomas include painless glistening red papule.
How is Pyogenic Granulomas Diagnosed?
Pyogenic granulomas is diagnosed through imaging studies such as sonography and CT scan.
How is Pyogenic Granulomas Treated?
Pyogenic granulomas are treated through medical therapy which include topical, systemic beta-adrenergic receptor antagonists. Surgical excision may also be considered.
What is the Prognosis of Pyogenic Granulomas?
The prognosis of pyogenic granulomas is fair.
What is a Glomus Tumor?
Glomus tumor is also known as glomangioma, a painful benign growth originating from specialized smooth muscle cells of glomus bodies, arteriovenous structures tangled in thermoregulation.
What is the Pathology of Glomus Tumor?
The pathology of glomus tumor is:
-Etiology: The cause of glomus tumor is glomus cells proliferation.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to glomus tumor not well known as event of glomus cell propagation is unknown.
-Morphology: The morphology associated with glomus tumor shows solitary well-circumscribed nodules lesion.
-Histology: The histology associated with glomus tumor shows unvaryingly round, trivial, glomus cells having pale eosinophilic cytoplasm.
How does Glomus Tumor Present?
Patients with glomus tumor typically have no sex predilection and present at age range of 20 to 40 years old. The symptoms, features, and clinical findings associated with glomus tumor include trivial, blue/red papules or nodules at the distal extremities.
How is Glomus Tumor Diagnosed?
Glomus tumor is diagnosed through clinical presentation and histologic findings.
How is Glomus Tumor Treated?
Glomus tumor is treated through surgical excision.
What is the Prognosis of Glomus Tumor?
The prognosis of glomus tumor is good with proper management surgical excision.
What are Lymphangiomas?
Lymphangiomas are benign lymphatic counterpart of hemangiomas, rare, hamartomatous, inborn malformations of the lymphatic system.
Examples of lymphangiomas include:
- Capillary lymphangiomas
- Cavernous lymphangiomas
What are Capillary Lymphangiomas?
Capillary lymphangiomas are also known as simple lymphangiomas, and are composed of small, lymphatic vessels located at the epidermis.
What is the Pathology of Capillary Lymphangiomas?
The pathology of capillary lymphangiomas is:
-Etiology: The cause of capillary lymphangiomas is an idiopathic associated lymphatic blockage.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to capillary lymphangiomas is not clearly understood.
-Morphology: The morphology associated with capillary lymphangiomas shows a little raised or sometimes pedunculated lesions up to 1 to 2 cm in diameter that occur predominantly in the head, neck, and axillary subcutaneous tissues.
-Histology: The histology associated with capillary lymphangiomas shows acanthosis and hyperkeratosis.
How does Capillary Lymphangiomas Present?
Patients with capillary lymphangiomas typically have no sex predilection, and present at an age range of infancy to 5 years old. The symptoms, features, and clinical findings associated with capillary lymphangiomas include trivial clusters of blisters on the skin prone to bleeding.
How is Capillary Lymphangiomas Diagnosed?
Capillary lymphangiomas is diagnosed through imaging studies which include ultrasound, MRI, CT scan, and biopsy.
How is Capillary Lymphangiomas Treated?
Capillary lymphangiomas is treated through medical care. Surgical excision may also be beneficial.
What is the Prognosis of Capillary Lymphangiomas?
The prognosis of capillary lymphangiomas is good with proper complete surgical excision.
What are Cavernous Lymphangiomas?
Cavernous lymphangiomas are types of lymhangiomas that are classically found on the neck, and axilla.
What is the Pathology of Cavernous Lymphangiomas?
The pathology of cavernous lymphangiomas is:
-Etiology: The cause of cavernous lymphangiomas is idiopathic associated lymphatic blockage.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to cavernous lymphangiomas not clearly understood, results from lymphatic system blockage during fetus deployments.
-Morphology: The morphology associated with cavernous lymphangiomas shows dilated lymphatics.
-Histology: The histology associated with cavernous lymphangiomas shows enormously dilated lymphatic spaces lined by endothelial cells.
How do Cavernous Lymphangiomas Present?
Patients with cavernous lymphangiomas typically have no sex predilection and present at an age range of infancy to 5 years old. The symptoms, features, and clinical findings associated with cavernous lymphangiomas include rubbery subcutaneous nodules.
How are Cavernous Lymphangiomas Diagnosed?
Cavernous lymphangiomas is diagnosed through imaging studies such as ultrasound, MRI, and CT scan. Biopsy may also be useful.
How is Cavernous Lymphangiomas Treated?
Cavernous lymphangiomas is treated through surgical excision.
What is the Prognosis of Cavernous Lymphangiomas?
The prognosis of cavernous lymphangiomas is good with proper management.
What are Vascular Ectasias?
Vascular ectasias are dilations of the vascular system rather than the neoplasm of existing vessels.
Examples of vascular ectasias include:
- Nevus flammeus
- Spider telangiectasias
- Hereditary hemorrhagic telangiectasia
What is Nevus Flammeus?
Nevus flammeus is a capillary malformation presenting a red or pink patch on a newborn’s skin.
What is the Pathology of Nevus Flammeus?
The pathology of nevus flammeus is:
-Etiology: The cause of nevus flammeus is unknown, familiar case associated.
-Genes involved: RASA1and EPHB4.
-Pathogenesis: The sequence of events that lead to nevus flammeus is not clearly understood.
-Morphology: The morphology associated with nevus flammeus shows the red or pink patch
-Histology: Abnormal vasculature.
How does Nevus Flammeus Present?
Patients with nevus flammeus typically have no gender preference present at age range of birth. The symptoms, features, and clinical findings associated with nevus flammeus include a light pink, deep purple flat lesion at the neck or head and a painless macule.
How is Nevus Flammeus Diagnosed?
Nevus flammeus is diagnosed through clinical presentation. Imaging studies- Ultrasound, CT scan, and MRI depict the associated superficial or deep tissue anomalies.
How is Nevus Flammeus Treated?
Nevus flammeus is treated through laser treatment and reassurance.
What is the Prognosis of Nevus Flammeus?
The prognosis of nevus flammeus is good. The condition is benign, and they regress spontaneously.
What is Spider Telangiectasias?
Spider telangiectasias is a general shape resembling that of a spider non-neoplastic vascular lesion.
What is the Pathology of Spider Telangiectasias?
The pathology of spider telangiectasias is: study of prominent bunches of injured small blood vessels in the skin. blue, red, or purple tortious bulging lines (spider-like appearance).
-Etiology: The cause of spider telangiectasias is aberrations in the vascular plexus.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to spider telangiectasias remains unknown.
-Morphology: The morphology associated with spider telangiectasias shows red, blue, or purple tortious lines
-Histology: Unknown.
How does Spider Telangiectasias Present?
Patients with spider telangiectasias typically more common in females than males present at age range of 30 to 50 years. The symptoms, features, and clinical findings associated with spider telangiectasias include purple, red or blue spider veins.
How is Spider Telangiectasias Diagnosed?
Spider telangiectasias is diagnosed grounded on history and examination, magnetic resonance venography (MRV) for mapping of venous system.
How is Spider Telangiectasias Treated?
Spider telangiectasias is treated through assurance, micro phlebectomy, sclerotherapy, laser treatment and thermocoagulation.
What is the Prognosis of Spider Telangiectasias?
The prognosis of spider telangiectasias is good. The condition is generally harmless.
What is Hereditary Hemorrhagic Telangiectasia?
Hereditary hemorrhagic telangiectasia is a rare condition that is characterized by numerous arteriovenous malformations.
What is the Pathology of Hereditary Hemorrhagic Telangiectasia?
The pathology of hereditary hemorrhagic telangiectasia is:
-Etiology: The cause of hereditary hemorrhagic telangiectasia is autosomal dominant syndrome that is instigated by gene mutations encoding components of the TGF-β signaling pathway of endothelial cells.
-Genes involved: ACVRL1, ENG, SMAD4.
-Pathogenesis: The sequence of events that lead to hereditary hemorrhagic telangiectasia are the result of defects in a TGF-β superfamily receptor. Advances of atypical vasculature cause clinical manifestation.
-Morphology: Numerous arteriovenous malformations lacking prevailing capillaries, resulting in arteries and veins direct connections.
-Histology: Numerous arteriovenous malformations lacking prevailing capillaries, resulting in arteries and veins direct connections.
How does Hereditary Hemorrhagic Telangiectasia Present?
Patients with hereditary hemorrhagic telangiectasia typically common in males over 15 years old. The symptoms, features, and clinical findings associated with hereditary hemorrhagic telangiectasia include epistaxis, anemia, telangiectases, and pulmonary hypertension.
How is Hereditary Hemorrhagic Telangiectasia Diagnosed?
Hereditary hemorrhagic telangiectasia is diagnosed through CBC count, coagulation studies, genetic tests, oximetry, and ABGs. Imaging- radiography, helical CT, MRI, angiography.
How is Hereditary Hemorrhagic Telangiectasia Treated?
Hereditary hemorrhagic telangiectasia is treated surgical and medical care of the symptoms.
What is the Prognosis of Hereditary Hemorrhagic Telangiectasia?
The prognosis of hereditary hemorrhagic telangiectasia is fair.
What are Borderline Tumors of the Vasculature?
Borderline tumors of the vasculature are regularly locally aggressive lesions, having the propensity to distant metastases.
Borderline tumors of the vasculature include:
- Hemangioendothelioma
- Kaposi sarcoma
What is Hemangioendothelioma?
Hemangioendothelioma is a rare spectrum of vascular tumors with characteristics intermediate between those of benign, well-differentiated hemangiomas and aggressively malignant angiosarcomas.
What is the Pathology of Hemangioendothelioma?
The pathology of hemangioendothelioma is:
-Etiology: The cause of hemangioendothelioma is genetic factor.
-Genes involved: ERPINE1-FOSB gen
-Pathogenesis: The sequence of events that lead to hemangioendothelioma; the lesion arises in the lower limbs soft tissue and less often in the trunk and upper limbs. There is t(7;19)(q22;q13) chromosomal translocation causing SERPINE1-FOSB gene union in the recurrent alteration.
-Morphology: The morphology associated with hemangioendothelioma shows nodular masses
-Histology: The histology associated with hemangioendothelioma shows cells that are plump/cuboidal and not well-defined vascular channels.
How does Hemangioendothelioma Present?
Patients with hemangioendothelioma typically have male predominance present at age range of 30 years. The symptoms, features, and clinical findings associated with hemangioendothelioma include pain, swelling round tumor, weight loss, walking difficulties, skin lumps, fever, and troubled breathing.
How is Hemangioendothelioma Diagnosed?
Hemangioendothelioma is diagnosed laboratory studies-biopsy. Imaging-CT scan, MRI, X-ray and PET scan.
How Hemangioendothelioma Treated?
Hemangioendothelioma is treated through surgical excision and radiotherapy.
What is the Prognosis of Hemangioendothelioma?
The prognosis of hemangioendothelioma is fair. Associated with recurrence and tendency to metastasize
What is Kaposi Sarcoma?
Kaposi sarcoma is a vascular neoplasm caused by Kaposi sarcoma herpesvirus (KSHV) (human herpesvirus-8, HHV-8)
What is the Pathology Kaposi Sarcoma?
The pathology of kaposi sarcoma is:
-Etiology: The cause of kaposi sarcoma is Kaposi sarcoma herpesvirus
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to kaposi sarcoma as the result of KSHV and altered T cell immunity. KSHV cause the lytic and latent infections at endothelial cells. Infected cells, KSHV-encoded proteins disturb usual cellular propagation controls by synthesis of cyclin D, viral homologue.
-Morphology: The morphology associated with kaposi sarcoma shows pink, red, or purple macules.
-Histology: The histology associated with kaposi sarcoma shows erupted erythrocytes, hemosiderin-laden macrophages, spindle cells proliferation.
How does Kaposi Sarcoma Present?
Patients with Kaposi sarcoma are typically males or females with HIV. The symptoms, features, and clinical findings associated with kaposi sarcoma include among others, pink, red, or purple macules, raised plaques, hemoptysis, dyspnea.
How is Kaposi Sarcoma Diagnosed?
Kaposi sarcoma is diagnosed through laboratory studies to check for CD4 lymphocyte counts. Imaging studies such as radiography, bronchoscopy, esophagogastroduodenoscopy (EGD)/colonoscopy. Biopsy is diagnostic.
How is Kaposi Sarcoma Treated?
Kaposi sarcoma is treated through medical care which may include antiretroviral therapy, radiation therapy laser therapy, cryotherapy, topical retinoids. Surgical excision may be helpful.
What is the Prognosis of Kaposi Sarcoma?
The prognosis of Kaposi sarcoma is poor.
What are Malignant tumors of the vasculature?
Malignant tumors of the vasculature are tumors that are highly destructive with the potential to recur, and significant distant metastasis.
Malignant tumors of the vasculature include:
- Angiosarcoma
- Hemangiopericytoma
What is Angiosarcoma?
Angiosarcoma is a malignant endothelial tumor ranging from extremely differentiated growths similar to hemangiomas to anaplastic lesions complex.
What is the Pathology of Angiosarcoma?
The pathology of angiosarcoma is:
-Etiology: The cause of angiosarcoma is unknown associated with the genetic factor.
-Genes involved: KDR, TP53, and PIK3CA.
-Pathogenesis: The sequence of events that lead to angiosarcoma are as the result of KDR, TP53, and PIK3CA genetic mutations.
-Morphology: The morphology associated with angiosarcoma shows small, sharply demarcated, asymptomatic red nodules.
-Histology: The histology associated with angiosarcoma shows plump atypical endothelial cells.
How does Angiosarcoma Present?
Patients with angiosarcoma typically have no gender preference present at age range of 20 to 70 years. The symptoms, features, and clinical findings associated with angiosarcoma include; extremity growing mass and demarcated, asymptomatic red nodules.
How is Angiosarcoma Diagnosed?
Angiosarcoma is diagnosed through laboratory studies profound thrombocytopenia. Imaging studies such as MRI or CT scans can show the extent of the disease. Biopsy is diagnostic.
How is Angiosarcoma Treated?
Angiosarcoma is treated through medical care which may include anthracycline-based regimens, paclitaxel, gemcitabine-based regimens. Radiotherapy and surgical care may be beneficial.
What is the Prognosis of Angiosarcoma?
The prognosis of angiosarcoma is poor 5-year survival rates are about 30%.
What is Hemangiopericytoma?
Hemangiopericytoma is a rare metastasis tumor derived from pericytes surrounding the blood vessels.
What is the Pathology of Hemangiopericytoma?
The pathology of hemangiopericytoma is:
-Etiology: The cause of hemangiopericytoma is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to hemangiopericytoma unknown.
-Morphology: Nodule.
-Histology: Blood vessels with prominent smooth muscle.
How does Hemangiopericytoma Present?
Patients with hemangiopericytoma typically more common in males. The symptoms, features, and clinical findings associated with hemangiopericytoma include among others, pain mass-related, temperature elevation, constipation vascular disease-allied symptoms, and difficulty breathing.
How is Hemangiopericytoma Diagnosed?
Hemangiopericytoma is diagnosed through biopsy and pathological examination.
How is Hemangiopericytoma Treated?
Hemangiopericytoma is treated through surgical excision.
What is the Prognosis of Hemangiopericytoma?
The prognosis of hemangiopericytoma is fair.