Ear pathology is any disease or disorder that affects the ear.
What is Inflammation of the Ear?
Inflammation of the ear are inflammatory processes involving the ear that are typically due to bacterial or viral infections. Inflammation of the ear can occur in the middle ear, the part of ear just behind an eardrum, as well as the outer and inner ear. They can be chronic or acute. Acute ear infections are painful, but short in duration and chronic ear infections either don’t clear up or recur many times, they can cause damage to the middle and inner ear which is infrequently permanent.
Examples of inflammation of the ear includes:
Acute otitis media
Chronic otitis media
Otitis externa
Malignant otitis externa
Swimmers ear
What is Acute Otitis Media?
Acute otitis media is an infectious disease of the middle ear. Acute otitis media is usually a complication of eustachian tube dysfunction that occurs during a viral upper respiratory tract infection.
What is the Pathology of Acute Otitis Media?
The pathology of acute otitis media is:
-Etiology: The cause of acute otitis media is most commonly Streptococcus pneumoniae. Acute otitis media may also be caused by Haemophilus influenzae, and Moraxella catarrhalis. Acute otitis media may also be caused by fungi or Pneumocystis in immunocompromised individuals.
-Pathogenesis: The sequence of events that lead to acute otitis media involve a complication of eustachian tube during an acute viral upper respiratory tract infection.
-Morphology: The morphology of acute otitis media include hyperemic, opaque, and bulging tympanic membrane with limited mobility. Acute otitis media may cause purulent otorrhea and small fragments of soft or rubbery granulation tissue.
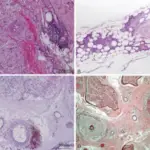
-Histology: The histology associated with acute otitis media shows acute inflammatory cells, haphazard glandular metaplasia with cilia, and hemorrhage. Cholesterol granulomas, and reactive bone formation may also be observed.
How does Acute Otitis Media Present?
Patients with acute otitis media typically are either male or female children. The symptoms, features, and clinical findings associated with acute otitis media include earache, irritability, fussiness, fever, drainage from the ear that is thick, yellow, or bloody, loss of appetite, and vomiting.
How is Acute Otitis Media Diagnosed?
Acute otitis media is diagnosed by physical examination of the ear to check for bulging of the tympanic membrane, new onset of otorrhea or erythema.
How is Acute Otitis Media Treated?
Acute otitis media is treated with antibiotics which typically include amoxicillin, or combination of amoxicillin and clavulanate.
What is the Prognosis of Acute Otitis Media?
The prognosis of acute otitis media is good. However, there are rare complications which include mastoiditis, labyrinthitis, meningitis, or abscess.
Chronic Otitis Media?
Chronic otitis media is a long term infection of the middle ear for more than six weeks.
What is the Pathology of Chronic Otitis Media?
The pathology of chronic otitis media is:
-Etiology: The cause of chronic otitis media is recurrent or persistent discharge (otorrhea) through a perforation in the tympanic membrane, which can lead to thickening of the middle ear mucosa and mucosal polyps. Chronic otitis media may also be a complication of persistent acute otitis media.
-Pathogenesis: The sequence of events that lead to chronic otitis media is that the middle ear can become inflamed or infected when the eustachian tube becomes blocked. Chronic otitis media results from persistent atelectasis or tympanic perforation, recurrent infection, and chronic effusion.
-Histology: The histology associated with chronic otitis media shows granulation tissue that may be soft or fibrous, and they may contain hemorrhage or cholesterol.
How does Chronic Otitis Media Present?
Patients with chronic otitis media typically are children. The symptoms, features, and clinical findings associated with chronic otitis media include popping, ringing, or a feeling of fullness or pressure in the ear. Children may rub their ears trying to relieve pressure.
How is Chronic Otitis Media Diagnosed?
Chronic otitis media is diagnosed by doing a physical exam, particularly an ear exam. Other tests may include hearing tests, tympanometry, tympanocentesis, or blood tests.
How is Chronic Otitis Media Treated?
Chronic otitis media may be treated with surgery called tympanoplasty with mastoidectomy. There are no medicines that will cure this disease and the primary goal of surgery for chronic otitis media is to remove all infection.
What is the Prognosis of Chronic Otitis Media?
The prognosis of chronic otitis media is good.
What is Otitis Externa?
Otitis externa is an inflammation or infection of the external auditory canal, the auricle, or both.
What is the Pathology of Otitis Externa?
The pathology of otitis externa is inflammation of the external ear canal, ear pain, which can be severe, itchiness in the ear canal. a discharge of liquid or pus from the ear, and some degree of temporary hearing loss.
-Etiology: The cause of otitis externa is typically a bacterial infection.
-Pathogenesis: The sequence of events that lead to otitis externa is by a bacterial infection, although the condition can also be caused by irritation, fungal infections, or allergies. There are a number of things that can make patients more likely to develop otitis externa including damaging the skin inside their ear or regularly getting water in their ear.
How does Otitis Externa Present?
Patients with otitis externa typically are females that present at the age range of 45 to 75 years old. The symptoms, features, and clinical findings associated with otitis externa include ear pain, itching and irritation in and around an ear canal, redness and swelling of an outer ear and ear canal, a feeling of pressure and fullness inside the ear. Scaly skin in and around an ear canal may also be appreciated.
How is Otitis Externa Diagnosed?
Otitis externa is diagnosed clinically based on signs and symptoms of canal inflammation. Presentation can range from mild discomfort, itching, and minimal edema to severe pain, complete canal obstruction, and involvement of the pinna and surrounding skin.
How is Otitis Externa Treated?
Otitis externa is treated effectively with ear drops.
What is the Prognosis of Otitis Externa?
The prognosis of otitis externa is good. In most cases the symptoms will start to improve within a few days of starting treatment.
What is Malignant Otitis Externa?
Malignant otitis externa is a potentially fatal external otitis due to Pseudomonas aeruginosa.
What is the Pathology of Malignant Otitis Externa?
The pathology of malignant otitis externa is:
-Etiology: The cause of malignant otitis externa Pseudomonas aeruginosa.
-Pathogenesis: The sequence of events that lead to malignant otitis externa is an infection that affects the external ear.
-Histology: The histology associated with malignant otitis externa shows ulcerated or necrotic epithelium with pseudoepitheliomatous hyperplasia. A mixed inflammatory infiltrate may be present.
How does Malignant Otitis Externa Present?
Patients with malignant otitis externa typically are female present at the age range of older adults. The symptoms, features, and clinical findings associated with malignant otitis externa include pain and headache, more severe than clinical signs would suggest, and foul-smelling greenish-yellow drainage from the ear.
How is Malignant Otitis Externa Diagnosed?
Malignant otitis externa is diagnosed with a physical exam. Ear drainage may be obtained and sent for microbial analysis.
How is Malignant Otitis Externa Treated?
Malignant otitis externa is treated with surgical debridement and antibiotics. Hyperbaric oxygen may also be used.
What is the Prognosis of Malignant Otitis Externa?
The prognosis of malignant otitis externa is poor.
What is Swimmer’s Ear?
Swimmers ear is a bacterial infection typically caused by water that stays in the outer ear canal for a long period of time, providing a moist environment for bacteria to grow.
What is the Pathology of Swimmer’s Ear?
The pathology of swimmer’s ear is:
-Etiology: The cause of swimmer’s ear is swimming in unclean water.
-Pathogenesis: The sequence of events that lead to swimmer’s ear is when water stays in the ear canal for a long period of time.
How does Swimmer’s Ear Present?
Patients with swimmers’ ears typically are either male or female, of all age ranges. The symptoms, features, and clinical findings associated with swimmer’s ear include redness of the outer ear, swelling, pain, and a pressure-plugged-up feeling in the ear.
How is Swimmer’s Ear Diagnosed?
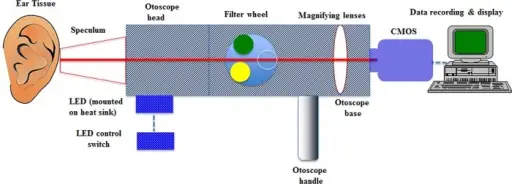
Swimmer’s ear is diagnosed with a physical exam using an otoscope. Any fluid drainage may be sent for microbial tests.
How is Swimmer’s Ear Treated?
Swimmer’s ear is treated by taking antibiotic ear drops.
What is the Prognosis of Swimmer’s Ear?
The prognosis of swimmer’s ear is good. With proper treatment from a healthcare provider, a swimmer’s ear often clears up in 7 to 10 days.
What are Cholesteatomas?
Cholesteatomas are skin-lined cysts in the ear.
What is the Pathology of Cholesteatomas?
The pathology of cholesteatomas is:
-Etiology: The cause of cholesteatomas is a chronic ear infection, colds, sinus infections, allergies, or an abnormal functioning eustachian tube.
-Pathogenesis: The sequence of events that lead to cholesteatomas is an infection in the middle ear which may affect the eustachian tube. If the eustachian tube is not working correctly, pressure build up within the middle ear can pull part of the eardrum the wrong way. This pulling of the eardrum may create a cyst or sac that fills with skin cells.
-Histology: The histology associated with cholesteatomas shows keratinized stratified squamous epithelium with granulation tissue. A chronic inflammatory infiltrate and keratin debris may also be appreciated.
How do Cholesteatomas Present?
Patients with cholesteatomas typically are males in their 20s or 30s. The symptoms, features, and clinical findings associated with cholesteatomas include a feeling of pressure, a bump in the ear, and possibly ear drainage. Cholesteatomas are usually painless.
How are Cholesteatomas Diagnosed?
Cholesteatomas are diagnosed by a physical exam to look for a visible deposit of skin cells or a large mass in the ear.
How are Cholesteatomas Treated?
Cholesteatomas are treated with a surgical treatment.
What is the Prognosis of Cholesteatomas?
The prognosis of cholesteatomas is fair.
What is Otosclerosis?
Otosclerosis is abnormal bone growth inside the ear.
What is the Pathology of Otosclerosis?
The pathology of otosclerosis is:
-Etiology: The cause of otosclerosis is unknown, but it is associated with measles virus.
-Pathogenesis: The sequence of events that lead to otosclerosis is when one of the bones in the middle ear, the stapes, becomes stuck in place. If the bones are unable to vibrate, sound is unable to travel through the ear and hearing becomes impaired.
-Histology: The histology associated with otosclerosis shows initially bone resorption and replacement by cellular fibrovascular tissue. Immature bone deposits may be present.
How does Otosclerosis Present?
Patients with otosclerosis typically are middle aged females. The symptoms, features, and clinical findings associated with otosclerosis include tinnitus, progressive gradual conductive hearing loss, and dizziness.
How is Otosclerosis Diagnosed?
Otosclerosis is diagnosed using tuning forks and hearing tests.
How is Otosclerosis Treated?
Otosclerosis is treated with stapedectomy which is a correction of fixation of footplate of stapes.
What is the Prognosis of Otosclerosis?
The prognosis of otosclerosis is fair. Otosclerosis may cause mild to severe hearing loss. Otosclerosis rarely causes complete deafness if treated.
What is Tinnitus?
Tinnitus is ringing in the ears.
What is the Pathology of Tinnitus?
The pathology of tinnitus is:
-Etiology: The cause of tinnitus is unknown, but is associated with ear injury, ear infections, medications, and age-related hearing loss.
-Pathogenesis: Unknown.
How does Tinnitus Present?
Patients with tinnitus are typically older adults. The symptoms, features, and clinical findings associated with tinnitus include ringing in the ear.
How is Tinnitus Diagnosed?
Tinnitus is diagnosed based on the patient’s description of the symptoms alone.
How is Tinnitus Treated?
Tinnitus is treated by addressing the possible underlying causes which include medication assessment, treating blood pressure, and earwax removal.
What is the Prognosis of Tinnitus?
The prognosis of tinnitus is good. Most tinnitus is mild and self resolves.
What is Meniere’s Disease?
Meniere’s disease is a feeling of vertigo, hearing loss, tinnitus, and sensation of ear fullness.
What is the Pathology of Meniere’s Disease?
The pathology of Meniere’s disease is:
-Etiology: The cause of Meniere’s disease is a distension of the membranous labyrinth by the endolymph.
-Pathogenesis: The sequence of events that lead to Meniere’s disease is inner ear pressure abnormalities or abnormal cochlear neurons.
How does Meniere’s Disease Present?
Patients with Meniere’s disease are typically females in their 40s to 60s. The symptoms, features, and clinical findings associated with Meniere’s disease include tinnitus, intermittent episodic vertigo, fluctuating hearing loss, and ear fullness.
How is Meniere’s Disease Diagnosed?
Meniere’s disease is diagnosed by a hearing test, and specialized physical exam maneuvers.
How is Meniere’s Disease Treated?
Meniere’s disease is treated with diuretics, dietary modification, and vasodilators.
What is the Prognosis of Meniere’s Disease?
The prognosis of Meniere’s disease is fair. There is 70% improvement after therapy.
What is Granulomatosis with Polyangiitis?
Granulomatosis with polyangiitis is a systemic necrotizing vasculitis that typically involves the upper respiratory tract, lungs, and kidneys.
What is the Pathology of Granulomatosis with Polyangiitis?
The pathology of granulomatosis with polyangiitis is:
-Etiology: The cause of granulomatosis with polyangiitis is an abnormal type of circulating antibody called antineutrophil cytoplasmic antibodies (ANCAs). These antibodies attack small and medium-sized blood vessels.
-Pathogenesis: The sequence of events that lead to granulomatosis with polyangiitis is when an initial inflammation-causing event provokes an abnormal immune system reaction which causes granulomas and constricted inflamed blood vessels.
-Histology: The histology associated with granulomatosis with polyangiitis shows granulomatous inflammation, necrosis, and vasculitis.
How does Granulomatosis with Polyangiitis Present?
Patients with granulomatosis with polyangiitis typically are adults 40 to 60 years old. The symptoms, features, and clinical findings associated with granulomatosis with polyangiitis include rhinitis, a runny and stuffy nose, cough which may include blood, ear infections, joint aches, loss of appetite, malaise, or a general feeling of being unwell, nosebleeds, shortness of breath, sinusitis, skin sores, swelling of joints, eye pain, burning sensation in the eyes, eye redness, vision problems, fever, weakness often due to anemia, unintended weight loss, and blood in the urine.
How is Granulomatosis with Polyangiitis Diagnosed?
Granulomatosis with polyangiitis is diagnosed by lab tests to check for signs of inflammation, anti-neutrophil cytoplasmic antibodies, anemia, or signs that kidneys aren’t properly filtering waste products from the blood. Urine tests can reveal whether urine contains red blood cells or has too much protein, which might indicate that the disease is affecting kidneys. CT or MRI can help determine which blood vessels and organs are affected. A biopsy can confirm a diagnosis of granulomatosis with polyangiitis.
How is Granulomatosis with Polyangiitis Treated?
Granulomatosis with polyangiitis is treated with corticosteroids. Immunosuppressive drugs may cause long term remission and reverse hearing loss and facial palsy.
What is the Prognosis of Granulomatosis with Polyangiitis?
The prognosis of granulomatosis with polyangiitis is fair. Granulomatosis with polyangiitis can lead to a rapidly progressive glomerulonephritis, a syndrome of the kidney that, if left untreated, rapidly progresses into acute renal, or kidney failure. About 75 % of people with the condition go on to develop kidney disease.
What are Tumors of the Ear?
Tumors of the ear are skin cancers that affect the ear, and benign tumors of the nerve of hearing (acoustic neuromas).
Examples of tumors of the ear include:
Basal cell carcinoma
Squamous cell carcinoma
Schwannoma
What is Basal Cell Carcinoma of the Ear?
Basal cell carcinoma of the ear is a nest of basaloid cells with peripheral palisading associated with a fibromyxoid stroma.
What is the Pathology of Basal Cell Carcinoma of the Ear?
The pathology of basal cell carcinoma of the ear is:
-Etiology: The cause of basal cell carcinoma of the ear is typically UV radiation.
-Genes involved: TP53, PTCH1, SMO, CDKN2A, RAS.
-Pathogenesis: The sequence of events that lead to basal cell carcinoma of the ear is UV radiation induced carcinogenesis, mutations in TP53 gene, PTCH1 gene mutations, and activating mutations in SMO gene and other genes including mutations in the CDKN2A gene and RAS genes.
-Histology: The histology associated with basal cell carcinoma of the ear shows basophilic palisading groups of cells.
How does Basal Cell Carcinoma of the Ear Present?
Patients with basal cell carcinoma of the ear typically are male present at the age range of middle aged adults with increasing incidence with age. The symptoms, features, and clinical findings associated with basal cell carcinoma of the ear include a nodular variant that usually presents as a pearly pink or flesh colored papule or nodule with arborizing and branching vessels. The borders of basal cell carcinomas are typically rolled.
How is Basal Cell Carcinoma of the Ear Diagnosed?
Basal cell carcinoma of the ear is diagnosed by clinical features, dermatoscopy, and histological features.
How is Basal Cell Carcinoma of the Ear Treated?
Basal cell carcinoma of the ear is treated by surgery.
What is the Prognosis of Basal Cell Carcinoma of the Ear?
The prognosis of basal cell carcinoma of the ear is fair.
What is Squamous Cell Carcinoma of the Ear?
Squamous cell carcinoma of the ear is a form of skin cancer that develops within the middle and outer layer of skin in the ear canal. This condition is life-threatening as the tumor can spread to the brain and the nerves around the ear.
What is the Pathology of Squamous Cell Carcinoma of the Ear?
The pathology of squamous cell carcinoma of the ear is:
-Etiology: The cause of squamous cell carcinoma of the ear is from prolonged exposure to ultraviolet (UV) radiation.
-Genes: XP xeroderma pigmentosum (XP).
-Pathogenesis: The sequence of events that lead to squamous cell carcinoma of the ear is propagation of genetic aberrations and malignant growth.
-Histology: The histology associated with squamous cell carcinoma of the ear shows infiltrative malignant cells with keratinization, and intercellular bridges.
How does Squamous Cell Carcinoma of the Ear Present?
Patients with squamous cell carcinoma of the ear typically are male present at the age range of 50s and 60s that spend an increased amount of time exposed to the sun. The symptoms, features, and clinical findings associated with squamous cell carcinoma of the ear include long standing chronic otitis media with sudden onset of pain, otorrhea, and hemorrhage. Most squamous cell carcinomas will grow and spread if untreated.
How is Squamous Cell Carcinoma of the Ear Diagnosed?
Squamous cell carcinoma of the ear is diagnosed by a physical examination and biopsy.
How is Squamous Cell Carcinoma of the Ear Treated?
Squamous cell carcinoma of the ear is treated by a radical surgery with or without radiation therapy or chemotherapy.
What is the Prognosis of Squamous Cell Carcinoma of the Ear?
The prognosis of squamous cell carcinoma of the ear is poor if untreated.
What is Schwannoma of the Ear?
Schwannoma of the ear is a neoplasm originating from Schwann cells.
What is the Pathology of Schwannoma of the Ear?
The pathology of schwannoma of the ear is:
-Etiology: The cause of schwannoma of the ear is not known.
-Genes: In most cases schwannomas occur spontaneously. Genetic disorders such as neurofibromatosis 2 (NF2), schwannomatosis, and Carney complex can cause schwannomas.
-Pathogenesis: The sequence of events that lead to schwannoma of the ear is tumor development from the schwann cells in the peripheral nervous system or cranial nerves.
-Histology: The histology associated with schwannoma of the ear shows interlacing fascicles of spindle cells with indistinct cytoplasmic borders, elongated and twisted nuclei. There is a biphasic population of Antoni A (cellular) and Antoni B (hypocellular, myxoid) patterns. Verocay bodies which are whorling or palisading of nuclei may also be appreciated.
How does Schwannoma of the Ear Present?
Patients with schwannoma of the ear typically are female present at the age range of 30s to 60s. The symptoms, features, and clinical findings associated with schwannoma of the ear include sensorineural hearing issues, tinnitus, and balance disturbances.
How is Schwannoma of the Ear Diagnosed?
Schwannoma of the ear may be diagnosed utilizing magnetic resonance imaging (MRI), computerized tomography (CT), X-rays, and ultrasounds. Balance, and hearing tests may also be utilized. Biopsy is confirmatory.
How is Schwannoma of the Ear Treated?
Schwannoma of the ear may be treated by excision.
What is the Prognosis of Schwannoma of the Ear?
The prognosis of schwannoma of the ear is fair.