Oral pathology is the specialty of dentistry and discipline of pathology that deals with the nature, identification, and management of diseases affecting the oral and maxillofacial regions.
What are Dental Caries?
Dental caries may be defined as a bacterial disease of calcified tissues of teeth and is characterized by demineralization of the inorganic and destruction of the organic substance of the tooth.
What is the Pathology of Dental Caries?
The pathology of dental caries is:
-Etiology: The causing factors of dental caries are bacteria, time, susceptible tooth surface, and fermentable carbohydrates.
-Genes involved: DEFB1.
-Pathogenesis: The sequence of events that lead to dental caries include enamel decay that may progress.
How does Dental Caries Present?
Patients with dental carries typically affect both males and females present at the age range of 10 years and above. Symptoms of dental caries are usually localized to the mouth. It includes holes in the surface of a tooth, pain when chewing, and sensitivity.
How are Dental Caries Diagnosed?
The diagnosis of carious lesions has been primarily a visual process, based principally on clinical inspection and review of radiographs.
How are Dental Caries Treated?
Dental caries are treated by fluoride treatments, fillings, crowns. root canals, tooth extractions.
What is the Prognosis of Dental Caries?
Dental caries prognosis depends on the health of the patient, maintenance of oral hygiene, and the extent and severity of dental caries. Overall the prognosis is fair.
What is Gingivitis?
Gingivitis is an inflammation of the gums, usually caused by a bacterial infection.
What is the Pathology of Gingivitis?
The pathology of gingivitis is:
-Etiology: The cause of gingivitis is poor oral hygiene.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to gingivitis are bacterial plaque, which acts to initiate the body’s host response. This, in turn, can lead to the destruction of the gingival tissues, which may progress to the destruction of the periodontal attachment apparatus.
-Morphology: The morphology associated with gingivitis shows red and puffy gums, that bleed easily when the person brushes their teeth.
How does Gingivitis Present?
Patients with gingivitis typically affect children aged 3-6 years old, but may involve many ages. The symptoms, features, and clinical findings associated with gingivitis include swollen gums, and halitosis.
How is Gingivitis Diagnosed?
Gingivitis is diagnosed based on clinical assessment data acquired during a comprehensive periodontal exam.
How is Gingivitis Treated?
Gingivitis is treated with scaling, root planing, curettage, mouth washes containing chlorhexidine or hydrogen peroxide, and flossing.
What is the Prognosis of Gingivitis?
The prognosis of gingivitis is good.
What is Periodontitis?
Periodontitis is defined as an inflammatory disease of supporting tissues of teeth caused by specific microorganisms or groups of specific microorganisms.
What is the Pathology of Periodontitis?
The pathology of periodontitis is:
-Etiology: The cause of periodontitis is plaque formation.
-Pathogenesis: The sequence of events that lead to periodontitis is the rapid tissue destruction followed by some repair and prolonged intervening periods of disease remission.
-Morphology: The morphology associated with periodontitis is unclear.
How does Periodontitis Present?
Patients with periodontitis typically affect females and males present at the age range of 30 years and above. The symptoms, features, and clinical findings associated with periodontitis include swollen gums, and bad breath.
How is Peridontitis Diagnosed?
Periodontitis is diagnosed through periodontal examination.
How is periodontitis is Treated?
Periodontitis is treated by professionally cleaning the pockets around teeth to prevent damage to the surrounding bone. Advanced cases may require surgery.
What is the Prognosis of Periodontitis?
The prognosis of periodontitis is considered fair.
What are Inflammatory and Reactive Lesions of the Oral Cavity?
Inflammatory and Reactive Lesions of the Oral Cavity include:
- Aphthous ulcers
- Fibrous proliferative lesions
What are Aphthous Ulcers?
Aphthous ulcers are small, shallow lesions that develop on the soft tissues in your mouth or at the base of your gums.
What is the Pathology of Aphthous Ulcer?
The pathology of aphthous ulcer is:
-Etiology: The cause of aphthous ulcer is stress.
-Pathogenesis: The sequence of events that lead to aphthous ulcer varies based on underlying medical conditions and environmental exposures. Predisposing factors implicated so far in the development of aphthous ulcers are: trauma, smoking cessation, stress, hormonal disorders, and food hypersensitivities
-Morphology: The morphology associated with shows the ulcers (aphthae, canker sores, or mouth sores) are normally shallow and begin as pale yellow in color, generally turning grey as the condition develops. They may be ringed with red or appear fully red when inflamed.
How does an aphthous ulcer Present?
Patients with aphthous typically affect males and females present at the age range of 25 and above. The symptoms, features, and clinical findings associated with aphthous ulcer include
small sores in the mouth that are round or oval, white, grey, or pale yellow with a red edge or border. A painful sore or sores that appear alone or in clusters inside your mouth.
How is Aphthous Ulcer Diagnosed?
Aphthous ulcer is diagnosed based on the history and clinical presentation. In patients with severe recurrent aphthous ulcers or canker sores, the clinical picture should guide laboratory testing.
How is Aphthous Ulcer Treated?
Aphthous ulcer is treated by the use of an antiseptic mouthwash e.g. containing chlorhexidine. In rare cases, a doctor may prescribe topical or oral antibiotics, such as tetracycline or minocycline.
What is the Prognosis of Aphthous Ulcer?
The prognosis of an aphthous ulcer is usually good. Minor aphthous ulcers are usually self-limiting, with the usual duration being about 10-14 days without any active treatment. Major aphthous ulcers can last up to about a month.
What are Fibrous Proliferative Lesions?
Fibrous proliferative lesions are characterized by the replacement of normal tissues by a fibrous matrix with various degrees of mineralization and ossification.
Examples of fibrous proliferative lesions include:
- Irritation fibromas
- Peripheral giant cell granulomas
- Pyogenic granulomas
- Peripheral ossifying fibromas
What is an Irritation Fibroma?
Irritation fibromas are fibrous nodules of the oral cavity, often considered to be reactive hyperplasia secondary to trauma or other local sources of irritation.
What is the Pathology of Irritation Fibroma?
The pathology of irritation fibroma is:
-Etiology: The cause of irritation fibroma is usually due to chronic irritation such as Cheek or lip biting. Rubbing from a rough tooth. Dentures or other dental prostheses.
-Pathogenesis: The sequence of events that lead to irritation occurs in response to local irritation or trauma and is characterized by the proliferation of collagenous connective tissue and blood vessels
How does Irritation Fibroma Present?
Patients with irritation fibroma typically affect females present at the age range of 40-60 years. The symptoms, features, and clinical findings associated with irritation fibromas include that irritation fibromas usually manifest an exophytic, firm, and asymptomatic nodule with a pink or flesh-colored and smooth surface. The nodule often has a well-defined boundary. It is slow-growing and rarely exceeds 1.5 cm in diameter.
How is irritation fibroma Diagnosed?
Irritation Fibroma is diagnosed clinically through biopsy
How is Irritation Fibroma Treated?
Irritation Fibroma is treated by surgical excision
What is the Prognosis of Irritation Fibroma?
The prognosis of irritation fibroma is usually very good.
What is Peripheral giant cell granuloma?
Peripheral giant cell granuloma is an oral pathologic condition that appears in the mouth as an overgrowth of tissue due to irritation or trauma.
What is the Pathology of Peripheral Giant Cell Granuloma?
The pathology of peripheral giant cell granuloma is:
-Etiology: The cause of peripheral giant cell granuloma is unknown, although local irritation due to dental plaque or calculus, periodontal disease, poor dental restorations, ill-fitting dental appliances, or dental extractions has been suggested to contribute to the development of the lesion.
-Pathogenesis: The sequence of events that lead to peripheral giant cell granuloma presumably arises from the periodontal ligament and thus occurs exclusively on the gingiva, usually between the permanent molars and incisors. The mandible and maxilla are involved at an almost equal frequency. PGCG classically presents as a solitary broad-based reddish-blue polypoid nodule
-Histology: The histology associated with peripheral giant cell granuloma shows fibrillar and reticular connective tissue stroma with abundant young connective tissue cells of fusiform shape, and multinucleated giant cells.
How does Peripheral Giant Cell Granuloma Present?
Patients with peripheral giant cell granuloma typically affect females present at the age range of 40-60 years. The symptoms, features, and clinical findings associated with peripheral giant cell granuloma include reddish-blue rubbery nodules that range in size from a few millimeters to 2cm. Surface ulceration is common
How is Peripheral Giant Cell Granuloma Diagnosed?
Peripheral Giant Cell Granuloma is diagnosed by blood tests, chest X-rays, CT or MRI, and biopsy.
How is Peripheral Giant Cell Granuloma Treated?
Peripheral Giant Cell Granuloma is treated by local surgical excision down to the bone.
What is the Prognosis of Peripheral Giant Cell Granuloma?
The prognosis of Peripheral Giant Cell Granuloma is fair.
What are Pyogenic Granulomas?
Pyogenic granuloma is also known as lobular capillary hemangioma – is a benign vascular tumor that occurs on the skin and mucous membranes, occasional it can be found subcutaneously or intravascularly.
What is the Pathology of Pyogenic Granuloma?
The pathology of pyogenic granuloma is:
-Etiology: The cause of pyogenic granuloma is trauma caused by cheek bites or by sharp cusps or fractured teeth.
-Pathogenesis: The sequence of events that lead to pyogenic granuloma is a response of tissues to minor trauma and/or chronic irritation, thus opening a pathway for invasion of nonspecific microorganisms, although microorganisms are seldom demonstrated within the lesion.
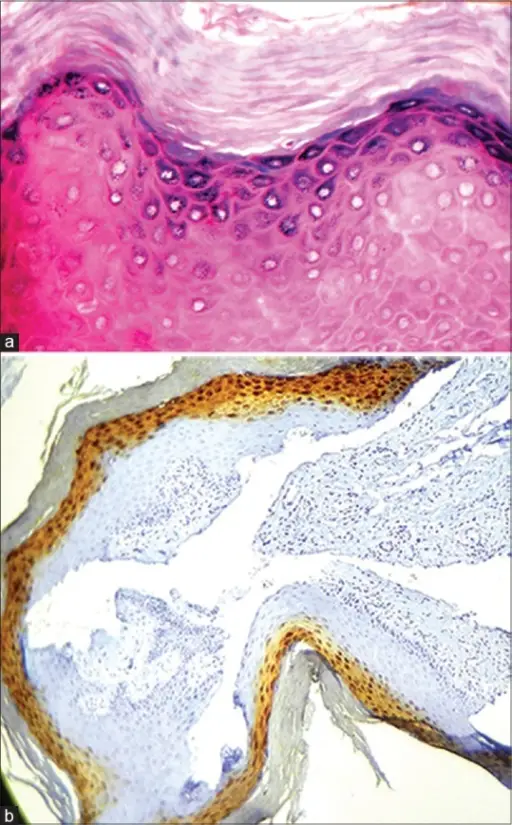
-Histology: The histology associated with pyogenic granuloma shows parakeratotic or non-keratinized stratified squamous epithelium.
How does Pyogenic Granuloma Present?
Patients with pyogenic granuloma typically affect females present at the age range of 20-60 years. The symptoms, features, and clinical findings associated with pyogenic granuloma include small shiny soft papules, with a smooth or slightly irregular surface, which is always elevated above the skin. It grows over a few days to reach its largest size, which is typically less than 2 cm. Larger lesions are uncommon but have been known to occur. It then stops enlarging and its diameter remains stationary for several weeks. The most conspicuous symptom is the ready occurrence of bleeding following even insignificant mechanical trauma.
How is Pyogenic Granuloma Diagnosed?
Pyogenic Granuloma is diagnosed based on its appearance. A biopsy is taken from the site to make a more accurate diagnosis.
How is Pyogenic Granuloma Treated?
Pyogenic Granuloma is treated by surgically removing if it’s recurred once after a nonsurgical approach. Alternatively, chemical, such as silver nitrate is applied to the pyogenic granuloma to help with the bleeding. These growths can also be removed using laser surgery.
What is the Prognosis of Pyogenic Granuloma?
The prognosis of pyogenic granuloma is fair but pyogenic granulomas can recur regardless of the therapeutic modality used.
What is Peripheral Ossifying Fibromas?
Peripheral ossifying fibroma is usually a fibroma of the gingiva which shows areas of calcification or ossification. It is a nonneoplastic enlargement of the gingiva.
-Etiology: The cause of peripheral ossifying fibromas is trauma.
-Pathogenesis: The sequence of events that lead to peripheral ossifying fibroma
POF arises as an exophytic, ulcerated mass attached to the gingiva that shares similar clinical features with other extraosseous lesions.
-Histology: The histology associated with peripheral ossifying fibroma shows either ulcerated or intact stratified squamous epithelium.
How does Ossifying Fibroma Present?
Patients with ossifying fibroma typically affect females. The symptoms, features, and clinical findings associated with ossifying fibroma include noticeable swelling and facial asymmetry.
How is Peripheral Ossifying Fibroma Diagnosed?
Peripheral Ossifying Fibroma diagnosis is based on excisional biopsy.
How is Peripheral Ossifying Fibroma Treated?
Peripheral Ossifying Fibroma is treated usually by surgical removal of the lesion down to the bone. If there are any adjacent teeth, they are cleaned thoroughly to remove any possible source of irritation.
What is the Prognosis of Peripheral Ossifying Fibroma?
The prognosis of peripheral ossifying fibroma is poor because the recurrence rate of the POF has been considered high for reactive lesions and it probably occurs due to incomplete initial removal, repeated injury, or persistence of the local irritants.
What are Infections of The Oral Cavity?
Infections of The Oral Cavity are the viral infections that manifest within the oral cavity.
Common infections of the oral cavity include:
- Candidiasis
- Fungal infections
- Herpes
What is Oral Candidiasis?
Oral candidiasis is a condition in which the fungus Candida albicans accumulates on the lining of your mouth. It’s also known as oral thrush, oropharyngeal candidiasis, or simply thrush.
What are Fungal Infections of the Oral Cavity?
Fungal infections of the oral cavity are the fungal infections that manifest within the oral cavity
Examples of fungal infections of the oral cavity include:
- Deep fungal infections
- Aspergillosis
- Blastomycosis
- Coccidioidomycosis
- Cryptococcosis
- Histoplasmosis
- Zygomycosis
| FUNGAL INFECTION | HISTOLOGY | PRESENTATION | TREATMENT | PROGNOSIS |
| ASPERGILLOSIS | Hyphae that are uniform, narrow (3 to 6 micrometers in width), tubular, and regularly septate. Branching is regular, progressive, and dichotomous. | Fever, cough, dyspnea, pleuritic chest pain, and sometimes hemoptysis in patients with prolonged neutropenia or immunosuppression. Aspergillus infection after organ transplantation most often occurs in bone marrow recipients. | Oral corticosteroids, Antifungal medications, Surgery | Prognosis is poor |
| BLASTOMYCOSIS | Broad verrucous lesion with epidermal papillomatosis which may resemble a keratoacanthoma. There may be surface erosion and suppuration. Numerous cystic spaces connect with the surface via draining sinuses. | Flu-like illness with fever, chills, myalgia, headache, chest pain, and a nonproductive cough | Antifungal medication. | Variable |
| COCCIDIOIDOMYCOSIS | Pseudoepitheliomatous hyperplasia of epidermis and adjacent or admixed acute suppurative inflammation. Variable infiltrate of neutrophils, eosinophils, histiocytes, multinucleated giant cells, plasma cells and rarely lymphocytes are present· | Reactive and organism-specific reactive manifestations do not contain visible microorganisms and may exhibit features of erythema nodosum, Sweet syndrome, and interstitial granulomatous dermatitis. Rarely, patients may exhibit features of erythema multiforme, acute generalized exanthema, secondary to hypersensitivity to systemic infection | Fluconazole or another type of antifungal medication. | Good |
| CRYPTOCOCCOSIS | Variably sized (3.5 – 8 μm in diameter)· Round to oval encapsulated yeasts with thin cell walls· | ·Opportunistic infection· | Liposomal amphotericin B | Good |
| HISTOPLASMOSIS | Yeast forms (2 – 5 um) with basophilic crescent-shaped nuclei | Diarrhea, bleeding, pain, nausea, vomiting, flu-like symptoms | Itraconazole Amphotericin for disseminated disease | Variable |
| ZYGOMYCOSIS | Coagulative necrosis due to fungi with broad, sparsely septate, thin-walled hyphae· | Necrosis | Amphotericin B or newer drugs· Surgical debridement | Poor prognosis |
What is Oral Herpes?
Oral herpes is an infection caused by the herpes simplex virus.
What is the Pathology of Oral Herpes?
The pathology of oral herpes is:
-Etiology: The cause of oral herpes is caused by the herpes simplex virus type 1 (HSV-1).
-Pathogenesis: The sequence of events that lead to oral herpes the virus is spread by contact, the usual site for the implantation is skin or mucous membrane.
-Histology: The histology associated with oral herpes shows a low power pattern of a typical lesion is of an intraepidermal blister the key feature is acantholysis with solitary keratinocytes within the blister cavity.
How does Oral Herpes Present?
Patients with oral herpes typically affect males and females both present at the range of 25 and above. The symptoms, features, and clinical findings associated with oral herpes include open sores or rashes with a burning sensation.
How is Oral Herpes Diagnosed?
Oral herpes is diagnosed with a virus culture called PCR, blood test, or biopsy. PCR is the preferred test for diagnosing herpes infections.
How is Oral Herpes Treated?
Oral Herpes is treated by keeping the infected area clean and dry. Taking antiviral oral medications, such as acyclovir, famciclovir, and valacyclovir.
What is the Prognosis of Oral Herpes?
The prognosis of oral herpes is good. The sores and symptoms of oral herpes usually completely disappear in two to three weeks with no scarring. However, the sores may reappear under certain stressful situations.
What is Hairy Leukoplakia?
Hairy leukoplakia is a condition triggered by the Epstein-Barr virus (EBV). It causes white patches on your tongue.
What is the Pathology of Hairy Leukoplakia?
The pathology of hairy leukoplakia is:
-Etiology: The cause of hairy leukoplakia is the Epstein-Barr virus (EBV).
-Genes involved: EBNA-2 gene.
-Pathogenesis: The sequence of events that lead to hairy leukoplakia is clearly complex, potentially requiring a convergence of factors including EBV co-infection, productive EBV replication, EBV genetic evolution, expression of specific EBV “latent” genes, and immune escape.
-Histology: The histology associated with hairy leukoplakia shows hyperkeratotic oral mucosa due to the piling of keratotic squamous epithelium.
How does Hairy Leukoplakia Present?
Patients with hairy leukoplakia typically affect males present in the range of 25 and above. The symptoms, features, and clinical findings associated with hairy leukoplakia include white patch, which almost exclusively occurs on the lateral surfaces of the tongue, although rarely it may occur on the buccal mucosa, soft palate, pharynx, or esophagus. The lesion may grow to involve the dorsal surface of the tongue. The texture is vertically corrugated (“hairy”) or thickly furrowed and shaggy in appearance.
How is Hairy Leukoplakia Diagnosed?
Hairy Leukoplakia is diagnosed through biopsy.
How is Hairy Leukoplakia Treated?
Hairy Leukoplakia is treated by topical use of podophyllum resin or retinoids has also been reported to produce a temporary remission. Antiretroviral drugs such as zidovudine may be effective in producing a significant regression of OHL.
What is the Prognosis of Hairy Leukoplakia?
The prognosis of hairy leukoplakia is fair.
What is Leukoplakia?
Leukoplakia is a white patch or plaque that cannot be scraped off and cannot be characterized clinically or pathologically as any other disease.
What is the Pathology Leukoplakia?
The pathology of leukoplakia is:
-Etiology: The cause of leukoplakia is related to alcohol, tobacco use, and micro-organisms.
-Genes involved: amplification of 8q24. 3, deletion of 8p23. 2, and dysregulation of DERL3, EIF5A2, ECT2, HOXC9, HOXC13, MAL, MFAP5, and NELL2.
-Pathogenesis: The sequence of events that lead to leukoplakia is the tumor suppressor genes that are involved in the regulation of normal cell turnover and apoptosis (programmed cell death).
-Histology: The histology associated with leukoplakia shows hyperkeratotic type squamous epithelium.
How does Leukoplakia Present?
Patients with leukoplakia typically affect males present at the range of 40-70 years. The symptoms, features, and clinical findings associated with leukoplakia include discomfort or pain. The exact appearance of the lesion is variable. Leukoplakia may be white, whitish-yellow, or grey. The size can range from a small area to much larger lesions. The most common sites affected are the buccal mucosa, the labial mucosa, and the alveolar mucosa, although any mucosal surface in the mouth may be involved.
How is Leukoplakia Diagnosed?
Leukoplakia is diagnosed by physical exam and histologic examination.
How is Leukoplakia Treated?
Leukoplakia is treated by the removal of leukoplakia patches.
What is the Prognosis of Leukoplakia?
The prognosis of leukoplakia is poor.
What is Erythroplakia?
Erythroplakia is any lesion of the oral mucosa that presents as bright red velvety plaques which cannot be characterized clinically or pathologically as any other recognizable condition. Such lesions are usually irregular in outline, although clearly demarcated from the adjacent normal epithelium.
What is the Pathology of Erythroplakia?
The pathology of erythroplakia is:
-Etiology: The cause of erythroplakia is smoking.
-Genes involved: p53 gene.
-Pathogenesis: The sequence of events that lead to erythroplakia is epidermoid carcinoma (squamous cell carcinoma). Epidermoid carcinoma originates in abnormal mucosa as either leukoplakia, erythroplakia, or speckled leukoplakia. This disease most commonly begins in a leukoplakic lesion which can be smooth or rough, flat or elevated, ulcerated or intact.
-Histology: The histology associated with erythroplakia reveals epithelial dysplasia, carcinoma in situ, and even invasive OSCC,
How does Erythroplakia Present?
Patients with erythroplakia typically affect males and females both present at the range of 25 and above. The symptoms, features, and clinical findings associated with erythroplakia include red macule or plaque with well-demarcated borders. The texture is characterized as soft and velvety. An adjacent area of leukoplakia may be found along with the erythroplakia.
How is Erythroplakia Diagnosed?
Erythroplakia is diagnosed only by biopsy.
How is Erythroplakia Treated?
Erythroplakia is treated by complete excision.
What is the Prognosis of Erythroplakia?
The prognosis of erythroplakia is poor.
What is Squamous Cell Carcinoma of the Oral Cavity?
Squamous Cell Carcinoma of the Oral Cavity refers to cancer occurring between the vermilion border of the lips and the junction of the hard and soft palates or the posterior one-third of the tongue.
What is the Pathology of Squamous Cell Carcinoma?
The pathology of squamous cell carcinoma is:
-Etiology: The cause of squamous cell carcinoma is UV solar radiation.
-Genes involved: Mutations in the p53 gene.
-Pathogenesis: The sequence of events that lead to squamous cell carcinoma is that the p53 protein stops cells with mutated or damaged DNA from replicating. If the p53 gene becomes mutated through the ways discussed above, then the p53 protein is rendered non-functional, and cells with damaged DNA, such as those found in squamous cell carcinoma can replicate.
-Histology: The histology associated with squamous cell carcinoma shows squamous epithelial cells arising from the epidermis and extending into the dermis the malignant cells are often large with abundant eosinophilic cytoplasm and a large, often vesicular, nucleus.
How does Squamous Cell Carcinoma Present?
Patients with squamous cell carcinoma typically affect male and female both present at the range of 50 and above. The symptoms, features, and clinical findings associated with squamous cell carcinoma include wart like growths.
How is Squamous Cell Carcinoma Diagnosed?
Squamous Cell Carcinoma is diagnosed by biopsy.
How is Squamous Cell Carcinoma Treated?
Squamous Cell Carcinoma is treated by surgical excision.
What is the Prognosis of Squamous Cell Carcinoma?
The prognosis of Squamous Cell Carcinoma is fair for initial cases but advanced squamous cell cancers have a poor prognosis with a 5-year survival rate below 40%
What are Odontogenic Cysts?
Odontogenic Cysts are a group of jaw cysts that are formed from tissues involved in odontogenesis (tooth development).
Inflammatory Odontogenic Cysts include:
- Paradental cyst
- Periapical cyst
- Residual cyst
Developmental cysts include:
- A calcifying epithelial odontogenic cyst (Gorlin Cyst)
- Dentigerous cysts
- Eruption cyst
- Gingival cyst of adult
- Gingival cyst of newborn
- Glandular odontogenic cyst
- Lateral periodontal cyst
- Odontogenic keratocysts
What is a Paradental Cyst?
A paradental cyst is an odontogenic cyst of inflammatory origin, which occurs on either the buccal, distal, or (rarely) mesial aspects of partially erupted mandibular third molars.
What is the Pathology of Paradental Cyst?
The pathology of paradental cyst is:
-Etiology: The cause of paradental cysts is they originate from the reduced epithelium of enamel or from the inflammatory proliferation of epithelial rests of Malassez that come from the superficial mucosa of a tooth in eruption (pericoronitis).
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to paradental cyst is that it arises from one of the reduced enamel epithelium, epithelial rests of Malassezia, crevicular epithelium, and epithelial remnants of the dental lamina.
-Histology: The histology associated with paradental cyst shows a fibrous connective tissue capsule invaded by a lymphocytic inflammatory infiltrate, lined by a hyperplastic, non-keratinized, stratified squamous epithelium.
How does Paradental Cyst Present?
Patients with paradental cysts typically affect males and females both present at the range of 25 and above. The symptoms, features, and clinical findings associated with paradental cyst include discomfort, tenderness, moderate pain, and, in some cases, suppuration through the periodontal sulcus
How Paradental Cyst Diagnosed?
Paradental Cyst is diagnosed by a positive electric pulp test.
How is Paradental Cyst Treated?
Paradental Cyst is treated by enucleation of the cyst without the extraction of the tooth.
What is the Prognosis of Paradental Cyst?
The prognosis of paradental cyst is good.
What is a Periapical Cyst?
A periapical cyst is also known as radicular cysts, are the most frequent cystic lesion related to teeth and result from an infection of the tooth.
What is the Pathology of Periapical Cyst?
The pathology of periapical cyst is:
-Etiology: The cause of periapical cyst is root infection involving tooth decay.
-Genes involved: MMP2 and MMP3
-Pathogenesis: The sequence of events that lead to periapical cyst epithelial cells from the rest of Malassez at the apex of the roots of a tooth become stimulated due to the body’s inflammatory response.
How does Periapical Cyst Present?
Patients with periapical cyst typically affect males present at the range of 20 to 60 years. The symptoms, features, and clinical findings associated with periapical cyst include swelling and pain. Initially, the cyst swells to a round hard protrusion, but later on, the body resorbs some of the cyst walls, leaving a softer accumulation of fluid underneath the mucous membrane. Secondary symptoms of periapical cysts include inflammation and infection of the pulp causing dental caries. This infection is what causes necrosis of the pulp.
How is Periapical Cyst Diagnosed?
Periapical Cyst is diagnosed through oral examination and laboratory tests
How is Periapical Cyst Treated?
Periapical Cyst is treated by root canal treatment or marsupialization.
What is the Prognosis of Periapical Cyst?
The prognosis of periapical cyst is good. Complete healing was observed in 75.0% of cases.
What is a Residual cyst?
Residual cysts are essentially radicular cysts without the presence of the offending dentition.
What is the Pathology of Residual Cyst?
-Etiology: The cause of residual cyst results from the extraction of a tooth with a radicular cyst. Trauma, carious lesion, or bacterial colonization of developmental anomaly affecting tooth irreversibly injures dental pulp.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to residual cyst is initiated by the spread of bacteria from a non-vital tooth in the periapical region of the jaw.
-Histology: The histology associated with residual cyst shows stratified squamous epithelium which may demonstrate exocytosis, spongiosis, or hyperplasia
How does Residual cyst Present?
Patients with Residual Cyst typically accounts for 10% of all jaw cysts. The symptoms, features, and clinical findings associated with residual cyst include a range from asymptomatic and only incidentally detected on imaging, to the expansion of the affected jaw region, to pain and drainage.
How is Residual Cyst Diagnosed?
Residual Cyst is diagnosed by laboratory tests.
How is Residual Cyst Treated?
Residual Cyst is treated by excising surgically, even in the absence of symptoms.
What is the Prognosis of Residual Cyst?
The prognosis of Residual Cyst is good. Residual cysts do not recur after appropriate management.
What is a Calcifying epithelial odontogenic cyst (Gorlin Cyst)?
A calcifying epithelial odontogenic cyst (Gorlin Cyst) is a benign odontogenic cyst that occurs in the gnathic bones. This cyst is part of a spectrum of lesions characterized by odontogenic epithelium containing “ghost cells,” which may undergo calcification.
What is the Pathology of Calcifying epithelial odontogenic cyst (Gorlin Cyst)?
The pathology of Calcifying epithelial odontogenic cyst (Gorlin Cyst):
-Etiology: The cause of calcifying epithelial odontogenic cyst (Gorlin Cyst) is odontogenic epithelial remnants (remains) that were trapped within the bones of the maxilla and mandible or gingival tissues. It is associated with impacted and unerupted teeth.
-Genes involved: The human homolog of the Drosophila segment polarity gene PTCH1.
-Pathogenesis: The sequence of events that lead to calcifying epithelial odontogenic cyst (Gorlin Cyst) Epithelial lining has the ability to induce the formation of dental tissues in adjacent connective tissue walls.
-Histology: The histology associated with calcifying epithelial odontogenic cyst (Gorlin Cyst) shows the stratified squamous epithelium.
How does Calcifying Epithelial Odontogenic Cyst (Gorlin Cyst) Present?
Patients with calcifying epithelial odontogenic cyst (Gorlin Cyst) typically affects male and female both present at the range of 33 and above. The symptoms, features, and clinical findings are associated with calcifying epithelial odontogenic cysts (Gorlin Cyst); Most calcifying odontogenic cysts appear asymptomatic. They are normally presented as a painless, slow-growing mass on the mandible and/or the maxilla, mostly in the front of the mouth. Symptoms include swelling in the mouth, both inside the bone, in the tooth-bearing areas, and outside the bone, in the gingiva.
How is Calcifying Epithelial Odontogenic Cyst (Gorlin Cyst) Diagnosed?
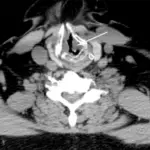
A calcifying epithelial odontogenic cyst (Gorlin Cyst) is diagnosed through a radiograph and CT scan.
How is Calcifying Epithelial Odontogenic Cyst (Gorlin Cyst) Treated?
A calcifying epithelial odontogenic cyst is treated as enucleation and curettage.
What is the Prognosis of Calcifying Epithelial Odontogenic cyst (Gorlin Cyst)?
The prognosis of the calcifying epithelial odontogenic cyst (Gorlin Cyst) is favorable. It has minimal chance of recurrence after simple surgical removal.
What is a Dentigerous Cyst?
Dentigerous cysts are a type of odontogenic cysts and generally occur in the ages of twenties or thirties. Dentigerous cyst always includes a tooth that cannot complete the eruption process and occurs around the crown by the fluid accumulation between the layers of the enamel organ.
What is the Pathology of Dentigerous Cyst?
The pathology of dentigerous cyst is:
-Etiology: The cause of dentigerous cyst is tooth enamel
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to dentigerous cyst includes the development from the accumulation of fluid (including glycosaminoglycans) between reduced enamel epithelium of dental follicle and crown of an unerupted tooth
-Histology: The histology associated with dentigerous cyst shows fibrous connective tissue and hyperplastic non-keratinized epithelium, sometimes elongated interconnecting rete ridges.
How does the Dentigerous cyst Present?
Patients with dentigerous cysts typically affect males and females present in the range of twenties and thirties. The symptoms, features, and clinical findings associated with dentigerous cyst include swelling, sensitivity, displacement.
How is a Dentigerous Cyst Diagnosed?
Dentigerous cyst is diagnosed by radiographic findings, in combination with clinical information, can support a histomorphology diagnosis
How is Dentigerous Cyst Treated?
Dentigerous cyst is treated by enucleation of the entire cyst, marsupialization, removal of the cysts sparing the permanent tooth.
What is the Prognosis of Dentigerous Cyst?
The prognosis of dentigerous cyst is the excellent prognosis, almost never recurs with complete enucleation, however, follow up radiographic studies recommended
What is an Eruption cyst?
Eruption cysts are benign cysts that appear on the mucosa of a tooth shortly before its eruption.
What is the Pathology of Eruption Cysts?
The pathology of eruption cyst is:
-Etiology: The cause of eruption cyst is unknown. However, some research suggests that early cavities, trauma, genetics or a lack of space for the tooth to move into can result in their formation.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to eruption cyst is the accumulation of fluid or hemorrhage between the crown of erupting tooth and the reduced enamel epithelium of the surrounding dental follicle
-Histology: The histology associated with eruption cyst shows dentigerous cyst (non-keratinized stratified squamous epithelium.
How does Eruption Cyst Present?
Patients with eruption cyst present in children under age 10. The symptoms, features, and clinical findings associated with eruption cyst include a dome shaped gingival mass.
How is Eruption Cyst Diagnosed?
Eruption Cyst is diagnosed by radiographic findings, in combination with clinical information, can support a histomorphologic diagnosis
How is Eruption Cyst Treated?
Eruption cyst is usually treated through marsupialization.
What is the Prognosis of Eruption Cyst?
The prognosis of eruption cyst is excellent.
What is a Gingival Cyst of an Adult?
Gingival cyst of an adult is a unique pathologic lesion of the oral cavity, typically localized in the mandibular canine and premolar region, appearing in adults in their fourth to fifth decades of life
What is the Pathology of Gingival Cyst of an adult?
The pathology of the gingival cyst of an adult is:
-Etiology: The cause of Gingival Cyst in adults is usually due to trauma.
-Genes involved: None.
-Pathogenesis: Arise from epithelial rests of dental lamina epithelium.
-Histology: The histology associated with a gingival cyst of adults shows unicystic structure lined with attenuated, non-keratinized low cuboidal or stratified squamous epithelium.
How does the Gingival Cyst of adults Present?
Patients with gingival cysts typically affect females present in the age range of 40-60 years.
The symptoms, features, and clinical findings associated with a gingival cyst of adults include The outward appearance of typically an oval-to-round, firm, elevated swelling located on the attached gingiva. Mostly are <5 mm in diameter, but lesions >5 cm.
How is Gingival Cyst of adult Diagnosed?
The gingival Cyst of an adult is diagnosed through a radiograph.
How is Gingival Cyst of adult Treated?
Gingival Cyst of an adult is treated by local surgical excision
What is the Prognosis of Gingival Cyst of adults?
The prognosis of gingival cysts in adults is good. They typically do not recur.
What is a Gingival Cyst of a Newborn?
The gingival cyst of newborns is an oral mucosal lesion of transient nature. Although it is a very common lesion within 3 to 6 weeks of birth, it is very rare to visualize the lesion thereafter. Presented here is a case report of a gingival cyst, which was visible just after 15 days of birth.
What is the Pathology of Gingival Cyst of Newborn?
The pathology of the gingival cyst of a newborn is:
-Etiology: The cause of the gingival cyst of newborns originates from the vestiges of dental lamina that has degenerated.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to gingival disease of newborns is from the vestiges of dental lamina that has degenerated. These remnants give rise to the gingival cysts and are lined by epithelium, which is capable of producing keratin.
-Histology: The histology associated with a gingival cyst of newborn shows small cysts lined with attenuated stratified squamous epithelium, fibrovascular stroma, without inflammatory cells.
How does Gingival Cyst of newborn Present?
Patients with gingival cysts typically affect newborns and infants. The symptoms, features, and clinical findings associated with a gingival cyst of the newborn include superficial papules.
How is Gingival Cyst of newborn Diagnosed?
Gingival Cyst of a newborn is diagnosed by differentiating from three other conditions, which are typically seen during the same time and possibly also have a location similarity. These include Natal teeth, Epstein’s pearls, and Bohn’s nodules.
How is Gingival Cyst of newborn Treated?
The gingival Cyst of a newborn usually requires no treatment, spontaneously rupture with cyst lining incorporated into the oral mucosa.
What is the Prognosis of Gingival Cyst of newborn?
The prognosis of gingival cyst of newborn good.
What is a Glandular odontogenic cyst?
A glandular odontogenic cyst is a rare and uncommon jaw bone cyst of odontogenic origin. It is a cyst having an unpredictable, potentially aggressive behavior, and has the propensity to grow in large size with a relatively high recurrence rate.
What is the Pathology of Glandular Odontogenic cyst?
The pathology of glandular odontogenic cyst is:
-Etiology: The cause of glandular odontogenic cyst is origin is rested of the dental lamina
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to glandular odontogenic cyst cellular mutation, cyst maturation at glandular, BCL-2 protein.
-Histology: The histology associated with glandular odontogenic cyst shows nonkeratinized or slightly basaloid epithelial cyst lining which may exhibit a number of microscopic parameters.
How does the Glandular Odontogenic Cyst Present?
Patients with Glandular Odontogenic cysts typically affect males and females present in the age range of 40-60 years. The symptoms, features, and clinical findings associated with Glandular Odontogenic cyst include Jaw expansion, swelling, impairment to the tooth, root, and cortical plate.
How is Glandular Odontogenic cyst Diagnosed?
Glandular Odontogenic cyst is diagnosed by biopsy, CT scans, and panoramic x-rays.
How is Glandular Odontogenic Cyst Treated?
Glandular Odontogenic cyst is treated by enucleation, curettage, marginal or partial resection, marsupialization
What is the Prognosis of Glandular Odontogenic cyst?
The prognosis of glandular odontogenic cyst is poor.
What is a Lateral periodontal Cyst?
A lateral periodontal cyst is a non-keratinized and non-inflammatory developmental cyst located adjacent or lateral to the root of a vital tooth
What is the Pathology of Lateral Periodontal Cyst?
-Etiology: The cause of lateral periodontal cyst is from epithelial rests in the periodontal ligament
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to lateral periodontal cyst remains controversial, with extensive debate in the literature over the different hypotheses.
-Histology: The histology associated with lateral periodontal cyst shows cystic lumens with thick linings.
How does a Lateral Periodontal cyst Present?
Patients with Lateral Periodontal cysts typically affect males and females present in the age range of 50-70 years. The symptoms, features, and clinical findings associated with lateral periodontal cyst include a small, soft-tissue swelling found just below or within the interdental papilla. However, as it is usually asymptomatic in nature, LPCs are usually detected through radiography.
How is Lateral Periodontal cyst Diagnosed?
Lateral Periodontal cyst is diagnosed in routine radiography.
How is the Lateral Periodontal Cyst Treated?
Lateral Periodontal cyst is treated by enucleation, curettage, or excision with preservation of adjacent teeth is adequate for conventional LPC
What is the Prognosis of Lateral Periodontal cyst?
The prognosis of lateral periodontal cyst is good with rare recurrence.
What is a Odontogenic Keratocysts?
Odontogenic keratocyst is the cyst arising from the cell rests of the dental lamina. It can occur anywhere in the jaw but is commonly seen in the posterior part of the mandible.
What is the Pathology of Odontogenic Keratocyst?
The pathology of odontogenic keratocyst is:
-Etiology: The cause of Odontogenic Keratocyst is generally thought to be derived from remnants of the dental lamina.
-Pathogenesis: The sequence of events that lead to odontogenic keratocyst is two-hit mechanism results in bi-allelic loss of PTCH (“patched”), tumor suppressor, on 9q22.3-q31 causing dysregulation of p53 and cyclin D1 oncoproteins.
-Histology: The histology associated with odontogenic keratocyst shows uniform epithelial lining 6 – 8 cells thick lacking rete ridges.
How does Odontogenic Keratocyst Present?
Patients with Odontogenic Keratocyst typically affect males and females present in the age range of 30-60 years. The symptoms, features, and clinical findings associated with odontogenic keratocyst include bony expansion or infection. However, bony expansion is uncommon as odontogenic keratocysts grow due to increased epithelial turnover rather than osmotic pressure. When symptoms are present they usually take the form of pain, swelling, and discharge due to secondary infection.
How is Odontogenic Keratocyst Diagnosed?
Odontogenic Keratocyst is diagnosed usually radiologically. However, a definitive diagnosis is through biopsy.
How is Odontogenic Keratocyst Treated?
Odontogenic keratocysts are treated by resection or enucleation.
What is the Prognosis of Odontogenic Keratocyst?
The prognosis of odontogenic keratocyst is poor. Recurrent OKC may develop in three different ways: By incomplete removal of the original cyst lining; by the retention of daughter cysts, from microcysts or epithelial islands in the wall of the original cyst, or by the development of new OKC from epithelial off-shoots of the basal layer.
What are Odontogenic Tumors?
Odontogenic Tumors are a group of neoplastic growths that originate from the tissues responsible for tooth formation and the periodontal apparatus of the jaw.
What are Odontomas?
Odontomas are benign tumors linked to tooth development. Specifically, it is a dental hamartoma, meaning that it is composed of normal dental tissue that has grown in an irregular way. It includes both odontogenic hard and soft tissues.
What is the Pathology of Odontomas?
The pathology of odontomas is:
-Etiology: The cause of odontomas is unknown.
-Genes involved:11q13. 3, FGF3, FGF4.
-Pathogenesis: The sequence of events that lead to odontomas is the alteration of differentiated mesenchymal and epithelial odontogenic cells; it has the capacity of forming enamel, dentin, and cement.
-Histology: The histology associated with odontomas shows scant or occasional ghost cell formation, can cause confusion with COC (CCOT / Gorlin cyst) calcifying cystic odontogenic tumor (CCOT).
How does Odontomas Present?
Patients with Odontomas typically affect males and females present in the early range. The symptoms, features, and clinical findings associated with odontomas include asymmetric tooth eruption, malposition, and devitalization.
How are Odontomas Diagnosed?
Odontomas are diagnosed dependent on clinical, radiologic, and pathologic correlation.
How is Odontomas Treated?
Odontomas are treated by excision.
What is the Prognosis of Odontomas?
The prognosis of odontomas is good. Recurrence is uncommon for isolated odontoma.
What is an Adenomatoid tumor?
The adenomatoid tumor is a well-recognized slow-growing benign tumor derived from a complex system of the dental lamina or its remnants.
What is the Pathology of an Adenomatoid tumor?
The pathology of adenomatoid tumor is:
-Etiology: The cause of the adenomatoid tumor is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to the adenomatoid tumor is unknown.
-Histology: The histology associated with adenomatoid tumors shows tubules, cords, or small nests composed of or lined with cuboidal cells.
How does Adenomatoid Tumor Present?
Patients with Adenomatoid tumors typically affect males and females present in the age range of 18-80 years. The symptoms, features, and clinical findings associated with adenomatoid tumors include painless, firm masses of <2 cm diameter.
How is Adenomatoid tumor Diagnosed?
An adenomatoid tumor is diagnosed primarily through biopsy.
How is Adenomatoid tumor Treated?
The adenomatoid tumor is treated by surgical excision.
What is the Prognosis of an Adenomatoid tumor?
The prognosis of an adenomatoid tumor is fair.
What is Ameloblastoma?
Ameloblastoma is a benign tumor that is nonfunctional, unicentric, intermittent in growth, anatomically benign and persistent.
What is the Pathology of Ameloblastoma?
The pathology of ameloblastoma is:
-Etiology: The cause of ameloblastoma is the remnants of the enamel organ or dental lamina.
-Genes involved: TGFB1, TGFB3, and GDF15.
-Pathogenesis: The sequence of events that lead to ameloblastoma are ameloblastoma arise from remnants of ameloblast or dental lamina, dentigerous cysts, or basal layer of the oral mucosa.
-Histology: The histology associated with ameloblastoma shows epithelial islands and cords of conventional ameloblastoma and the cystic epithelial lining of unicystic ameloblastoma.
How does Ameloblastoma Present?
Patients with Ameloblastoma typically affect males and females present in the age range of 40-50 years. The symptoms, features, and clinical findings associated with ameloblastoma include painless jaw swelling and ulceration.
How is Ameloblastoma Diagnosed?
Ameloblastoma is diagnosed based on clinical, radiologic, and pathologic correlation
How is Ameloblastoma Treated?
Ameloblastoma is treated through segmental resection and through nonsurgical therapy.
What is the Prognosis of Ameloblastoma?
The prognosis of ameloblastoma is fair.
What is a Calcifying epithelial odontogenic tumor (Pindborg tumor)?
A calcifying epithelial odontogenic tumor (Pindborg tumor) is a rare benign epithelial odontogenic neoplasm of slow growth that is locally aggressive and tends to invade bone and adjacent soft tissue.
What is the Pathology of Calcifying Epithelial Odontogenic Tumor?
The pathology of calcifying epithelia odontogenic tumor is:
-Etiology: The cause of the calcifying epithelial odontogenic tumor is unknown.
-Genes involved: Involvement of PTCH1 mutation.
-Pathogenesis: The sequence of events that lead to calcifying epithelial odontogenic tumor originate from the epithelial rests of the dental lamina or from the reduced enamel epithelium that overlies the crowns of the teeth.
-Histology: The histology associated with calcifying epithelial odontogenic tumor shows sheets of polyhedral, eosinophilic squamous epithelial cells with focal psammoma bodies.
How does Calcifying Epithelial Odontogenic Tumor Present?
Patients with Calcifying Epithelial Odontogenic Tumor typically affect males and females present in the age range of 40-50 years. The symptoms, features, and clinical findings associated with calcifying epithelial odontogenic tumors include enlarging, painless mass, nasal airway obstruction, epistaxis, and proptosis are sometimes experienced in the maxilla.
How is Calcifying Epithelial Odontogenic Tumor Diagnosed?
The calcifying epithelial odontogenic tumor is diagnosed by incisional and excisional biopsy.
How is Calcifying epithelial odontogenic tumor Treated?
The calcifying epithelial odontogenic tumor is treated by resection that includes a margin of normal soft tissue or bone is recommended.
What is the Prognosis of Calcifying Epithelial Odontogenic Tumor?
The prognosis of calcifying epithelial odontogenic tumors is fair.
What is a Squamous Odontogenic Tumor?
Squamous odontogenic tumor is a rare, benign, locally infiltrative neoplasm of the jaws that appears to originate from the rest of Malassezia.
What is the Pathology of a Squamous Odontogenic Tumor?
The pathology of squamous odontogenic tumor is:
-Etiology: The cause of the squamous odontogenic tumor is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to the squamous odontogenic tumor is still unclear in which remnants of the dental lamina (rests of Serres), epithelial rests of Malassez, or gingival epithelium are the main suspected origin.
-Histology: The histology associated with squamous odontogenic tumor shows stratified squamous epithelium within the fibrous stroma, often well-defined nests with clear cells.
How does Squamous Odontogenic Tumor Present?
Patients with Squamous odontogenic tumors typically affect males and females present in the age range of 40-50 years. The symptoms, features, and clinical findings associated with squamous odontogenic tumor include painless, slow-growing swelling is the most common presenting sign.
How is Squamous Odontogenic Tumor Diagnosed?
Squamous odontogenic tumor is diagnosed by excisional biopsy.
How is Squamous Odontogenic Tumor Treated?
Squamous odontogenic tumor is treated by excision with the extraction of involved teeth
What is the Prognosis of Squamous Odontogenic Tumor?
The prognosis of a squamous odontogenic tumor is good.
What is an Ameloblastic Carcinoma?
Ameloblastic carcinoma is a rare malignant (cancerous) tumor that normally begins in the bones of the jaw.
What is the Pathology of Ameloblastic Carcinoma?
The pathology of ameloblastic carcinoma is:
-Etiology: The cause of ameloblastic carcinoma is de novo.
-Genes involved: p53 gene.
-Pathogenesis: The sequence of events that lead to ameloblastic carcinoma is little to unknown however, malignant transformation of ameloblastomas may occur spontaneously or following chemotherapy or adjuvant radiotherapy.
-Histology: The histology associated with ameloblastic carcinoma shows peripheral palisading, reverse polarization, stellate reticulum.
How does Ameloblastic Carcinoma Present?
Patients with ameloblastic carcinoma typically affect males and females present in the age range of 40-50 years. The symptoms, features, and clinical findings associated with ameloblastic carcinoma include jaw pain and swelling.
How is Ameloblastic Carcinoma Diagnosed?
Ameloblastic Carcinoma is diagnosed by clinical, radiologic, and pathologic correlation
How is Ameloblastic Carcinoma Treated?
Ameloblastic Carcinoma is treated by composite surgical resection, with adjuvant radiation and chemotherapy as appropriate
What is the Prognosis of Ameloblastic Carcinoma?
The prognosis of ameloblastic carcinoma is poor.
What is a Clear-cell odontogenic carcinoma?
Clear-cell odontogenic carcinoma is a rare odontogenic tumor of the jaws.
What is the Pathology of Clear- cell Odontogenic Carcinoma?
The pathology of clear-cell odontogenic carcinoma is:
-Etiology: The cause of clear cell odontogenic carcinoma is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to clear-cell odontogenic carcinoma is unknown.
Histology: The histology associated with clear cell odontogenic carcinoma shows clear cells which are positive for cytokeratin and negative for vimentin and also negative for mucicarmine, which differentiates it from some of the other clear cell tumors such as mucoepidermoid carcinoma and renal carcinoma and calcifying epithelial odontogenic tumor (CEOT)
How does Clear Cell Odontogenic Carcinoma Present?
Patients with Clear cell odontogenic carcinoma typically affect females present in the age range of 40-60 years. The symptoms, features, and clinical findings associated with clear cell odontogenic carcinoma include swelling, tooth mobility, and pain
How is Clear Cell Odontogenic Carcinoma Diagnosed?
Clear cell odontogenic carcinoma is diagnosed dependent on clinical, radiologic, and pathologic correlation.
How is Clear Cell Odontogenic Carcinoma Treated?
Clear cell odontogenic carcinoma is a treated combination of chemotherapy (Paclitaxel and carboplatin or irinotecan plus cisplatin) and surgical resection.
What is the Prognosis of Clear Cell Odontogenic carcinoma?
The prognosis of clear cell odontogenic carcinoma is poor. The recurrence rate of 30% of resected and 87% of curetted/enucleated lesions
What is a Ghost Cell Odontogenic Carcinoma?
Ghost cell odontogenic carcinoma is an uncommon odontogenic carcinoma. All reported cases demonstrated malignant histological features such as cellular pleomorphism, mitosis, and necrosis with anucleated eosinophilic aggregates [ghost cells] in association with odontogenic epithelium.
What is the Pathology of Ghost Cell Odontogenic Carcinoma?
The pathology of ghost cell odontogenic carcinoma is:
-Etiology: The cause of ghost cell odontogenic carcinoma is thought to arise from calcifying odontogenic cysts (COCs) with features of either calcifying cystic odontogenic tumor or dentinogenic ghost cell tumor.
-Genes involved: CTNNB1gene.
-Pathogenesis: The sequence of events that lead to ghost cell odontogenic carcinoma is unclear.
-Histology: The histology associated with ghost cell odontogenic carcinoma shows peripheral palisading, reverse polarization, stellate reticulum.
How does Ghost Cell Odontogenic Carcinoma Present?
Patients with Ghost cell odontogenic carcinoma typically affect males and females present in the age range of 40-50 years. The symptoms, features, and clinical findings associated with ghost cell odontogenic carcinoma include swelling, tooth mobility, and pain
How is Ghost Cell Odontogenic Carcinoma Diagnosed?
Ghost cell odontogenic carcinoma is diagnosed dependent on clinical, radiologic, and pathologic correlation
How is Ghost Cell Odontogenic Carcinoma Treated?
Ghost cell odontogenic carcinoma is treated by composite surgical excision
What is the Prognosis of Ghost Cell Odontogenic Carcinoma?
The prognosis of ghost cell odontogenic carcinoma poor with an overall 5-year survival rate is 73% and recurrence is common
What is Malignant Ameloblastoma?
Malignant ameloblastoma is a rare odontogenic tumor.
What is the Pathology of Malignant Ameloblastoma?
The pathology of malignant ameloblastoma is:
-Etiology: The cause of malignant ameloblastoma is metastasis
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to ameloblastic carcinoma is the embryologic events that initiate and control the formation of human odontogenic structures through a finely regulated series of inductive interactions between epithelium and ectomesenchyme.
-Histology: The histology associated with ameloblastic carcinoma shows peripheral palisading columnar.
How does Ameloblastic Carcinoma Present?
Patients with Ameloblastic Carcinoma typically affect males and females present in the age range of 40-50 years. The symptoms, features, and clinical findings associated with ameloblastic carcinoma include pain and a lump or swelling in the jaw. If left untreated, the tumor can grow very large, distorting the shape of the lower face and jaw and shifting teeth out of position.
How is Ameloblastic Carcinoma Diagnosed?
Ameloblastic carcinoma is diagnosed based on clinical, radiologic, and pathologic correlation.
How is Ameloblastic Carcinoma Treated?
Ameloblastic carcinoma is treated b surgical excision.
What is the Prognosis of Ameloblastic Carcinoma?
The prognosis of ameloblastic carcinoma is poor. Metastatic cases to lung tend to show indolent clinical behavior with long survival times.
What is a Primary Intraosseous Squamous Cell Carcinoma?
Primary intraosseous squamous cell carcinoma is a rare epithelial odontogenic malignancy affecting the jaws and having no initial connection with oral mucosa and presumably developing from remnants of the odontogenic epithelium or from an odontogenic cyst or tumor.
What is the Pathology of Primary Intraosseous squamous cell carcinoma?
The pathology of primary intraosseous squamous cell carcinoma is:
-Etiology: The cause of primary intraosseous squamous cell carcinoma is smoking, alcohol, and tobacco chewing.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to primary intraosseous squamous cell carcinoma originates from odontogenic cysts with a nonkeratinized epithelial lining, especially from radicular/residual and dentigerous cysts.
-Histology: The histology associated with primary intraosseous squamous cell carcinoma shows carcinoma of keratinocytes that infiltrates the dermis
How does Primary Intraosseous Squamous Cell Carcinoma Present?
Patients with primary intraosseous squamous cell carcinoma typically affect males and females present at the range of 30-60 years. The symptoms, features, and clinical findings associated with primary intraosseous squamous cell carcinoma include pain and swelling
How is Primary intraosseous squamous cell carcinoma Diagnosed?
Primary intraosseous squamous cell carcinoma is diagnosed based on clinical, radiologic, and pathologic correlation.
How is Primary intraosseous squamous cell carcinoma Treated?
Primary intraosseous squamous cell carcinoma is treated by surgical excision.
What is the Prognosis of Primary intraosseous squamous cell carcinoma?
The prognosis of primary intraosseous squamous cell carcinoma is poor.
Tumors of odontogenic ectomesenchyme:
- Cementoblastoma
- Odontogenic fibroma
- Odontogenic myxoma
What is a Cementoblastoma?
Cementoblastoma is a relatively rare benign neoplasm of the cementum of the teeth. It is derived from ectomesenchyme of odontogenic origin.
What is the Pathology of Cementoblastoma?
The pathology of cementoblastoma is:
-Etiology: The cause of cementoblastoma is unknown and is linked with many sources, including trauma, nutritional deficiency, metabolic disturbances, and constitutional factors.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to cementoblastoma develop as cells that generate cementum, or cementoblasts uncontrollably proliferate at the apex of a tooth root. Cementoblasts that form the cementum typically cease activity and become cementocytes.
-Histology: The histology associated with cementoblastoma shows large cementicles (globules) fused to form a mass within the proliferative fibrovascular stroma.
How does Cementoblastoma Present?
Patients with Cementoblastoma typically affect males and females present in the age range of 20-30 years. The symptoms, features, and clinical findings associated with cementoblastoma include dull pain and dentin hypersensitivity can occur as growth increases. Visibility of the cementoblastoma may increase with growth and cause distortion/swelling to the face and surrounding areas along with tooth displacement.
How is Cementoblastoma Diagnosed?
Cementoblastoma is diagnosed using a radiograph in which it shows dense homogenous mass continuous with tooth root.
How is Cementoblastoma Treated?
Cementoblastoma is treated by surgically removing the mass and possibly a portion of the affected area and/or teeth.
What is the Prognosis of Cementoblastoma?
The prognosis of cementoblastoma is good.
What is an Odontogenic Fibroma?
Odontogenic fibroma is an extremely rare benign tumor that accounts for 0.1% of all odontogenic tumors. It appears as an asymptomatic expansion of the cortical plate of the mandible or maxilla.
What is the Pathology of Odontogenic Fibroma?
The pathology of odontogenic fibroma is:
-Etiology: The cause of odontogenic fibroma is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to odontogenic fibroma is a proliferation of mature odontogenic mesenchyme.
-Histology: The histology associated with odontogenic fibroma shows cellular fibro collagenous tissue with scattered, small, inactive odontogenic epithelium in strands, cords, or nests
How does Odontogenic Fibroma Present?
Patients with Odontogenic Fibroma typically affect females present in the age range of 20-40 years. The symptoms, features, and clinical findings associated with odontogenic fibroma include swelling and pain.
How is Odontogenic Fibroma Diagnosed?
Odontogenic fibroma is diagnosed depending on clinical, radiologic, and pathologic correlation
How is Odontogenic Fibroma Treated?
Odontogenic fibroma is treated by excision, enucleation, and curettage
What is the prognosis of odontogenic fibroma?
The prognosis of odontogenic fibroma depends on the type of odontogenic fibroma.
What is an Odontogenic myxoma?
Odontogenic myxoma is a rare intraosseous neoplasm, which is benign but locally aggressive. It rarely appears in any bone other than the jaws. It is considered to be derived from the mesenchymal portion of the tooth germ.
What is the Pathology of Odontogenic Myxoma?
The pathology of odontogenic myxoma is:
-Etiology: The cause of odontogenic myxoma is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to odontogenic myxoma is the embryonic dental anlage of mesenchymal tissue.
-Histology: The histology associated with odontogenic myxoma shows spindled to stellate cells with eosinophilic cytoplasm set in a myxoid matrix.
How does Odontogenic Myxoma Present?
Patients with odontogenic myxoma are typically females. The symptoms, features, and clinical findings associated with odontogenic myxoma include a painless, slowly enlarging expansion of the jaw with possible tooth loosening or displacement.
How is Odontogenic Myxoma Diagnosed?
Odontogenic myxoma is diagnosed depending on clinical, radiologic, and pathologic correlation
How is Odontogenic Myxoma Treated?
Odontogenic myxoma is treated by surgery.
What is the Prognosis of Odontogenic Myxoma?
The prognosis of odontogenic myxoma is fair with a ~25% recurrence rate.
Benign tumors of odontogenic epithelium and ectomesenchyme:
- Adenomatoid odontogenic tumor
- Ameloblastic fibroma
- Ameloblastic fibro-odontoma
- A calcifying cystic odontogenic tumor (calcifying odontogenic cyst)
- Complex odontoma
- Compound odontoma
- Dentinogenic ghost cell tumor
- Odontoameloblastoma
What is an Adenomatoid odontogenic tumor?
The adenomatoid odontogenic tumor is a rare tumor of epithelial origin.
What is the Pathology of Adenomatoid Odontogenic Tumor?
The pathology of adenomatoid odontogenic tumor is:
-Etiology: The cause of the adenomatoid odontogenic tumor is derived from a complex system of the dental lamina or its remnants.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to an adenomatoid odontogenic tumor arising from the enamel organ, the epithelial lining of dentigerous cyst epithelial rests of Malassez of the deciduous or permanent tooth or remnants of the dental lamina
-Histology: The histology associated with adenomatoid odontogenic tumor shows well-circumscribed, the central proliferation of ductlike epithelium surrounding small foci of calcification.
How does Adenomatoid Odontogenic tumor Present?
Patients with Adenomatoid Odontogenic tumors typically affect females present in the age range of 30-60 years. The symptoms, features, and clinical findings associated with adenomatoid odontogenic tumor include engulfing of the crown and root by the tumor.
How is Adenomatoid Odontogenic tumor Diagnosed?
The adenomatoid odontogenic tumor is diagnosed through radiographs.
How is Adenomatoid odontogenic tumor Treated?
The adenomatoid odontogenic tumor is treated by enucleation.
What is the Prognosis of an Adenomatoid odontogenic tumor?
The prognosis of an adenomatoid odontogenic tumor was good.
What is Ameloblastic fibroma?
Ameloblastic fibroma is a rare odontogenic tumor comprising neoplastic epithelial and mesenchymal tissues.
What is the Pathology of Ameloblastic fibroma?
The pathology of ameloblastic fibroma is:
-Etiology: The cause of ameloblastic fibroma is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to ameloblastic fibroma is unclear
-Histology: The histology associated with ameloblastic fibroma shows small islands and cords of markedly attenuated ameloblastic epithelium two cells thick within dense collagenous stroma that is often immature.
How does Ameloblastic Fibroma Present?
Patients with Ameloblastic Fibroma typically affect females present in the age range of 40-60 years. The symptoms, features, and clinical findings associated with ameloblastic fibroma include; Small tumors are asymptomatic, while larger ones produce significant swelling of the jaws
How is Ameloblastic Fibroma Diagnosed?
Ameloblastic fibroma is diagnosed by radiography and histology.
How is Ameloblastic Fibroma Treated?
Ameloblastic fibroma is treated by enucleation and curettage. However, extensive and aggressive lesions may require radical treatment such as excision.
What is the Prognosis of Ameloblastic Fibroma?
The prognosis of Ameloblastic fibroma is good.
What is an Ameloblastic Fibro-odontoma?
Ameloblastic fibro-odontoma is a neoplasm consisting of odontogenic ectomesenchyme resembling the dental papilla, epithelial strands, and nest resembling dental lamina and enamel organ conjunction with the presence of dentine and enamel.
What is the Pathology of Ameloblastic Fibro-odontoma?
The pathology of ameloblastic fibro-odontoma is:
-Etiology: The cause of ameloblastic fibro-odontoma is developmental.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to ameloblastic fibro-odontoma; lesions with odontogenic epithelium with odontogenic ectomesenchyme, with or without hard tissue formation.
-Histology: The histology associated with ameloblastic fibro-odontoma shows numerous cords and follicles of odontogenic epithelium exhibiting peripheral ameloblast-like cells within primitive ectomesenchyme tissue.
How does Ameloblastic Fibro-odontoma Present?
Patients with Ameloblastic Fibro-odontoma typically affect males and females present in the age range of 40-60 years. The symptoms, features, and clinical findings associated with ameloblastic fibro-odontoma include swelling and failure of tooth eruption
How is Ameloblastic Fibro-odontoma Diagnosed?
Ameloblastic fibro-odontoma is diagnosed clinical, radiologic, and pathologic correlation.
How is Ameloblastic Fibro-odontoma Treated?
Ameloblastic fibro-odontoma is treated by a conservative surgical approach such as excision.
What is the Prognosis of Ameloblastic Fibro-odontoma?
The prognosis of ameloblastic fibro-odontoma is good.
What is a Calcifying Cystic Odontogenic Tumor (calcifying odontogenic cyst)?
A calcifying cystic odontogenic tumor (calcifying odontogenic cyst) is a benign cystic neoplasm of odontogenic origin that demonstrates ghost cells in the epithelial component.
What is the Pathology of Calcifying Cystic Odontogenic Tumor (calcifying odontogenic cyst)?
The pathology of Calcifying cystic odontogenic tumor calcifying odontogenic cyst is:
-Etiology: The cause of Calcifying cystic odontogenic tumor calcifying odontogenic cyst is unknown
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to Calcifying cystic odontogenic tumor calcifying odontogenic cyst; they arise from odontogenic epithelial remnants that were trapped within the bones of the maxilla and mandible or gingival tissues.
-Histology: The histology associated with Calcifying cystic odontogenic tumor calcifying odontogenic cyst shows cyst lining is of odontogenic epithelium with a well-defined layer of palisading basal cells, loosely arranged suprabasal epithelial cells resembling stellate reticulum, similar to ameloblastoma
How does Calcifying Cystic Odontogenic Tumor Calcifying Odontogenic Cyst Present?
Patients with calcifying cystic odontogenic tumor calcifying odontogenic cyst typically affects many people of varying age ranges. The symptoms, features, and clinical findings associated with calcifying cystic odontogenic tumor calcifying odontogenic cyst include a painless, slow-growing mass on the mandible and/or the maxilla.
How is Calcifying cystic odontogenic tumor calcifying odontogenic cyst Diagnosed?
Calcifying cystic odontogenic tumor calcifying odontogenic cyst is diagnosed based on incisional biopsy or enucleation specimen.
How is Calcifying cystic odontogenic tumor (calcifying odontogenic cyst) Treated?
A calcifying cystic odontogenic tumor (calcifying odontogenic cyst) is treated by enucleation and curettage.
What is the Prognosis of Calcifying cystic odontogenic tumor (calcifying odontogenic cyst)?
The prognosis of Calcifying cystic odontogenic tumor (calcifying odontogenic cyst) is excellent.
What is a Complex odontoma?
Complex odontoma is a common odontogenic tumor, and it is usually a hard painless mass, which rarely exceeds the diameter of the tooth. Most of these lesions are discovered accidentally on radiographic examination.
What is the Pathology of Complex Odontoma?
The pathology of a complex odontoma is:
-Etiology: The cause of complex odontoma is local trauma, inflammatory and/or infectious processes, and hereditary anomalies.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to complex odontoma growth of completely differentiated epithelial and mesenchymal cells that give rise to ameloblasts and odontoblasts.
-Histology: The histology associated with complex odontoma shows the more disorganized or haphazard arrangement of pulpal tissues, enamel, or dentin.
How does Complex Odontoma Present?
Patients with Complex Odontoma typically affect males and females present in the age range of 05-50 years. The symptoms, features, and clinical findings associated with complex odontoma include they are usually asymptomatic.
How is Complex Odontoma Diagnosed?
Complex Odontoma is diagnosed clinical, radiologic, and pathologic correlation
How is Complex Odontoma Treated?
Complex odontoma is treated by excision
What is the Prognosis of Complex Odontoma?
The prognosis of a complex odontoma is good.
What is a Compound odontoma?
Compound odontoma is regularly calcified tissue that bears similarity to teeth or appears as a collection of small teeth.
What is the Pathology of Compound Odontoma?
The pathology of a compound odontoma is:
-Etiology: The cause of compound odontoma is unknown
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to compound odontoma growth of completely differentiated epithelial and mesenchymal cells that give rise to ameloblasts and odontoblasts.
-Histology: The histology associated with compound odontoma shows similar to the layering of the normal tooth in the relation of dentin, enamel matrix, and pulp.
How does Compound Odontoma Present?
Patients with Complex Odontoma typically affect males and females present in the age range of 10-30 years. The symptoms, features, and clinical findings associated with compound odontoma include they are usually asymptomatic.
How is Compound Odontoma Diagnosed?
Compound odontoma is diagnosed by clinical, radiologic, and pathologic correlation
How is Compound Odontoma Treated?
Compound odontoma is treated by excision, enucleation, and curettage
What is the Prognosis of Compound Odontoma?
The prognosis of a compound odontoma is good.
What is a Dentinogenic ghost cell tumor?
Dentinogenic ghost cell tumor is a locally invasive neoplasm that is characterized by ameloblastoma-like epithelial islands, ghost cells, and dentoid.
What is the Pathology of Dentinogenic ghost cell tumor?
The pathology of dentinogenic ghost cell tumor is:
-Etiology: The cause of dentinogenic ghost cell tumor is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to dentinogenic ghost cell tumor is the signaling pathway that has a role in the development similar to calcifying odontogenic cyst since beta-catenin gene mutations and beta-catenin overexpression is also identified in DGCT.
-Histology: The histology associated with dentinogenic ghost cell tumor shows solid mass consisting of sheets of anastomosing cords and strands of the odontogenic epithelium; microcystic development is possible.
How does Dentinogenic Ghost Cell Tumors Present?
Patients with dentinogenic ghost cell tumors typically affect males and females present in the age range of 11-79 years. The symptoms, features, and clinical findings associated with dentinogenic ghost cell tumors include they are asymptomatic.
How are Dentinogenic Ghost Cell Tumors Diagnosed?
Dentinogenic ghost cell tumor is diagnosed by radiologic and histopathologic correlation
How are Dentinogenic Ghost Cell Tumors Treated?
Dentinogenic ghost cell tumor is treated simple enucleation, curettage
What is the Prognosis of Dentinogenic Ghost Cell Tumors?
The prognosis of dentinogenic ghost cell tumors is poor.
What is an Odontoameloblastoma?
Odontoameloblastoma is an extremely rare odontogenic tumor that contains an ameloblastomatous component together with odontoma-like elements.
What is the Pathology of Odontoameloblastoma?
The pathology of odontoameloblastoma is:
-Etiology: The cause of odontoameloblastoma is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to odontoameloblastoma is that mineralized dental tissues are formed as a hamartomatous proliferation in response to inductive stimuli produced by the proliferating epithelium over the mesenchymal tissue.
-Histology: The histology associated with odontoameloblastoma show proliferating odontogenic epithelium with peripheral palisading, reverse polarization and stellate reticulum.
How does Odontoameloblastoma Present?
Patients with Odontoameloblastoma typically affect males present in the age range of 02-50 years. The symptoms, features, and clinical findings associated with odontoameloblastoma include swelling, dull pain, delayed eruption of teeth, bone expansion
How is Odontoameloblastoma Diagnosed?
Odontoameloblastoma is diagnosed dependent on clinical, radiologic, and pathologic correlation
How is Odontoameloblastoma Treated?
Odontoameloblastoma is treated by enucleation or excision.
What is the Prognosis of Odontoamelobalstoma?
The prognosis of odontoameloblastoma is poor.
What is an Ameloblastic Fibrosarcoma?
Ameloblastic fibrosarcoma is an uncommon odontogenic tumor composed of a benign epithelial component and a malignant ectomesenchymal component
What is the Pathology of Ameloblastic Fibrosarcoma?
The pathology of ameloblastic fibrosarcoma is:
-Etiology: The cause of ameloblastic fibrosarcoma is de novo tumors tend to occur in younger patients
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to ameloblastic fibrosarcoma; they are derived from epithelial, ectomesenchymal, and mesenchymal elements of the tooth-forming apparatus.
-Histology: The histology associated with ameloblastic fibrosarcoma shows biphasic with benign epithelium and malignant stroma.
How does Ameloblastic Fibrosarcoma Present?
Patients with Ameloblastic Fibrosarcoma typically affect males present in the age range of 30-50 years. The symptoms, features, and clinical findings associated with ameloblastic fibrosarcoma include painful but occasionally painless facial mass with accompanying paresthesia or dysesthesia
How is Ameloblastic Fibrosarcoma Diagnosed?
Ameloblastic fibrosarcoma is diagnosed dependent on clinical, radiologic, and pathologic correlation
How is Ameloblastic Fibrosarcoma Treated?
Ameloblastic fibrosarcoma is treated by surgical resection and radiotherapy.
What is the Prognosis of Ameloblastic Fibrosarcoma?
The prognosis of ameloblastic fibrosarcoma is good.