Upper airway pathology is any lesion or disorder that may occur in the upper airway, which consists of the nose, pharynx, and larynx.
What is Inflammation of the Nose?
Inflammation of the nose is a condition of the mucosal lining of the nose characterized by the basic signs; redness, hotness, swelling, pain, and sometimes function loss
Examples of inflammatory reactions of the nose include:
- Allergic rhinitis
- Chronic rhinitis
- Infectious rhinitis
- Sinusitis
What is Allergic Rhinitis?
Allergic rhinitis is the inflammation of the nasal passages mucosal precipitated by sensitivity responses to one of a hefty cluster of allergens characterized by obvious redness, mucosal edema, and mucus discharge, convoyed by a leukocytic infiltration.
What is the Pathology of Allergic Rhinitis?
The pathology of allergic rhinitis is:
-Etiology: The cause of allergic rhinitis is caused by an immunoglobulin E–mediated reaction due to several allergens to nasal mucosa.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to allergic rhinitis is due to sensitization to allergic causing factors.
-Histology: The histology associated with allergic rhinitis shows eosinophils, basophils, mast cells, and T cells.
How does Allergic Rhinitis Present?
Patients with allergic rhinitis typically are wide ranging. The condition can begin in patients as young as two years. The symptoms, features, and clinical findings associated with allergic rhinitis include Rhinorrhea, nasal congestion, postnasal drainage, Repetitive sneezing, snoring, frequent sore throat, constant clearing of the throat, cough, headaches, and pale nasal turbinate among others.
How is Allergic Rhinitis Diagnosed?
Allergic rhinitis is diagnosed mainly through history and allergic tests.
How is Allergic Rhinitis Treated?
Allergic rhinitis is treated through allergen elimination or avoidance. Topical nasal steroids may be helpful.
What is the Prognosis of Allergic Rhinitis?
The prognosis of allergic rhinitis is good a majority of patients live normal lives with the signs. Roughly, improve throughout the teenaged years, but most symptoms reappear later.
What is Chronic Rhinitis?
Chronic rhinitis is a sequel to recurrent attacks of acute rhinitis, whether microbial or allergic in source, with the ultimate advance of superimposed microbial infection.
What is the Pathology of Chronic Rhinitis?
The pathology of chronic rhinitis is:
-Etiology: The cause of chronic rhinitis is either whether microbial (adenoviruses) or allergic in the source which attacks recurrently.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to chronic rhinitis follows the repeated attacks of allergic rhinitis or non-allergic rhinitis.
-Histology: The histology associated with chronic rhinitis shows desquamation and ulceration of the mucosal epithelium and neutrophils, lymphocytes, and plasma cells subjacent to the epithelium. Glandular and goblet cell hyperplasia may also be present.
How does Chronic Rhinitis Present?
Patients with chronic rhinitis typically both males and females affected in equal proportions. Present at age range of 21-30 years which is its pick determine age range of people typically affected). The symptoms, features, and clinical findings associated with chronic rhinitis include those of acute rhinitis. Rhinorrhea, nasal congestion, postnasal drainage, repetitive sneezing, snoring, frequent sore throat, constant clearing of the throat, and cough may also be present.
How is Chronic Rhinitis Diagnosed?
Chronic rhinitis is diagnosed through medical history- recurrent rhinitis throughout. no definitive laboratory studies though may include those of rhinitis; skin-prick testing, Serum allergen-specific IgE testing, nasal smear, and cell blood count with differential are laboratory studies when history is relevant.
How is Chronic Rhinitis Treated?
Chronic rhinitis is treated the same way as acute rhinitis which includes; medical care- nasal/oral corticosteroids, saline nasal irrigation. Analgesics, oral-systemic decongestants. Surgical treatment is not recommended. Only when there are polyps or suggestively deviated nasal septum triggering nasal congestion.
What is the Prognosis of Chronic Rhinitis?
The prognosis of chronic rhinitis is good as with other rhinitis. Advantageous if underlying causative factors are addressed and treated early.
What is Infectious Rhinitis?
Infectious rhinitis is a common cold, caused by an upper respiratory tract infection. Caused mainly by one or more viruses. Major contributors are rhinoviruses, echoviruses, and adenoviruses.
What is the Pathology of Infectious Rhinitis?
The pathology of Infectious rhinitis is:
-Etiology: The cause of infectious rhinitis is mainly viral in origin: They include adenovirus, rhinovirus, coronavirus, respiratory syncytial virus, parainfluenza virus, or enterovirus.
-Genes involved: CFTR gene.
-Pathogenesis: The sequence of events that lead to infectious rhinitis infection of the upper airway tract by the virus.
-Histology: The histology associated with infectious rhinitis shows hydropic erosion and loss of cilia. Goblet cells and submucosal glands are agitated. The lamina propria, edematous and thinly infiltrated with inflammatory cells. Swelling to the mucous membrane causes mild respiratory distress, sneezing, and snuffling.
How does Infectious Rhinitis Present?
Patients with infectious rhinitis typically there is no variance in rates of infection among men and women. The symptoms, features, and clinical findings associated with infectious rhinitis include clear discharge to mucopurulent nasal discharge.
How is Infectious Rhinitis Diagnosed?
Infectious rhinitis is diagnosed mainly through medical history and physical examination. Laboratory tests include white blood cell count, as peripheral WBC may surge during the infection.
How is Infectious Rhinitis Treated?
Infectious rhinitis is treated encompass supportive treatment for symptoms of respiratory illness since the condition is self-limited.
What is the Prognosis of Infectious Rhinitis?
The prognosis of infectious rhinitis is excellent. The manifestation, the common cold, is usually mild and self-limited. Recovery is usually within a week for adolescents/adults and within two weeks for young children.
What is Sinusitis?
Sinusitis is condition characterized by inflammation of the paranasal sinuses lining.
What is the Pathology of Sinusitis?
The pathology of sinusitis is:
-Etiology: The cause of sinusitis is acute or chronic rhinitis, an extension of a periapical infection through the bony floor of the sinus in case of maxilla sinusitis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to sinusitis is an inflammatory response.
-Histology: The histology associated with sinusitis shows there are numerous neutrophils, lymphocytes, plasma cells, and some eosinophils with abundant edema on the paranasal sinuses.
How does Sinusitis Present?
Patients with sinusitis typically, women have more occurrences of infective sinusitis than men. Present at age range of 3 to 15years most common in children than adults. The symptoms, features, and clinical findings associated with sinusitis include. Nasal obstruction., mucopurulent nasal drainage, craniofacial discomfort described/interorbital heaviness such as facial dull pain, frank periorbital, or facial edema. fever (new-onset), cough that worsens at night, diminished sense of smell.
How is Sinusitis Diagnosed?
Sinusitis is diagnosed through the medical history and physical exam.
How is Sinusitis Treated?
Sinusitis is treated through the following modalities: Medical care – antimicrobial medication first line amoxicillin. Symptomatic treatment includes Warm compresses, adequate hydration, nonnarcotic analgesia, smoking cessation, humidification, and balanced nutrition.
What is the Prognosis of Sinusitis?
The prognosis of sinusitis is fair. Roughly about 40% case of acute sinusitis resolves impulsively without antibiotics. The impulsive cure of viral origin sinusitis is about 98%. When treated with proper antibiotics, show speedy improvement. The relapse rate after efficacious treatment is <5%.
What are Nasal Polyps?
Nasal polyps are pedunculated grape-like masses of tissue. Recurrent bouts of rhinitis may lead to nasal polyps.
What is the Pathology of Nasal Polyps?
The pathology of nasal polyps is:
-Etiology: The cause of nasal polyps is chronic inflammation (rhinitis).
-Genes involved: mucin (MUC)5AC, MUC5B, and MUC2 genes.
-Pathogenesis: The sequence of events that lead to nasal polyps remains unclear.
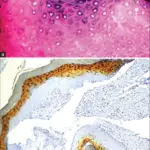
-Histology: The histology associated with nasal polyps shows edematous connective tissue comprising some mucous glands and the variable number of inflammatory cells plasma cells, lymphocytes, and eosinophils. Allergic polyps partake plenty of eosinophils and also hyperplasia of mucous glands.
How does Nasal Polyps Present?
Patients with nasal polyps typically, the male-to-female ratio is 2-4:1 in adults. Present at age range of older than 20years Common in the generation of 40 years and above. The symptoms, features, and clinical findings associated with nasal polyps include Chronic or recurrent acute sinusitis symptoms and signs. headaches, postnasal drainage, snoring airway obstruction, chronic mouth breathing, dull, and rhinorrhea.
How is Nasal Polyps Diagnosed?
Nasal polyps is diagnosed through, medical history and physical examination. Laboratory studies including; sweat chloride test, nasal smear, and serologic radioallergosorbent test. Imaging studies, maxillofacial CT scan, and MRI.
How is Nasal Polyps Treated?
Nasal polyps is treated through medical care; Oral/topical nasal steroid therapy, and leukotriene receptor antagonist, analgesic. Surgical intervention, endoscopic sinus surgery, and polypectomy.
What is the Prognosis of Nasal Polyps?
The prognosis of nasal polyps is fair recurrence following medical/surgical treatment usually common in case of multiple benign polyps.
What are Necrotizing Lesions of the Nose and Upper Airways?
Necrotizing lesions of the nose and upper airways are condition caused either by fungal infections (mucormycosis), Wegener granulomatosis, and or polymorphic.
Examples of necrotizing lesions of the nose and upper airways include:
- Acute fungal infections
- Extranodal T/NK-cell lymphoma:
- Granulomatosis with polyangiitis (Wegener granulomatosis)
What Acute Fungal Infections Cause Necrotizing Infections of the Nose and Upper Airway?
Acute fungal infections cause necrotizing infections of the nose and upper airway is Mucormyzosis.
What is Mucormycosis?
Mucormycosis is an opportunistic contagion caused by mold fungi, that including Rhizopus, Absidia, Mucorall, Cunninghamella, and belong to the class Zygomycetes.
What is the Pathology of is Mucormycosis?
The pathology of is mucormycosis is:
-Etiology: The cause of mucormycosis is Fungal bread mold fungi. Other predisposing factors; neutropenia, corticosteroid use, diabetes mellitus, and breakdown of the cutaneous barrier.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to mucormycosis. Fungal is transmitted through airborne asexual spores. Inhaled or through percutaneous, causes infection to the sinus and or lungs. There is phagocytic and oxidative elimination of spore largely by macrophage cells (neutrophils) throughout established infection.
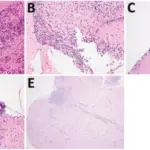
-Histology: The histology associated with mucormycosis shows pathognomonic broad, asymmetrical, ribbonlike, hyphae with uneven branching. Neutrophil infiltration, tissue infarction, and vessel invasion are observed. A granulomatous reaction was also seen.
How does Mucormycosis Present?
Patients with mucormycosis typically since is not a notifiable illness, the true prevalence is mysterious. The symptoms, features, and clinical findings associated with mucormycosis include: facial pain, nasal congestion, numbness, black discharge retro-orbital headache, dyspnea, fever, hemoptysis, abdominal pain, and cellulitis.
How is Mucormycosis Diagnosed?
Mucormycosisis diagnosed through laboratory tests: Complete blood cell (CBC) count for neutropenia. Arterial blood gas (ABG) study assesses for acidosis. Blood cultures to check for bacteremia. Molecular based testing using fresh tissue over paraffin tissue. Biopsy for histology. Radiologic Studies; CT scan of the sinuses, brain, chest, and abdomen. Sinuses and brain Magnetic resonance imaging (MRI).
How is Mucormycosis Treated?
Mucormycosis is treated as follows. Medical care; Treating the underlying abnormality, managing DKC, and correcting neutropenia. Prompt antifungal therapy first-line liposomal amphotericin B. Surgical interventions, necrotic tissue debridement. Drainage of the sinuses and excision of the orbital contents and affected brain tissue.
What is the Prognosis Mucormycosis?
The prognosis of Mucormycosisis poor. Mortality due to mucormycosis fluctuates flanked by 40%-80%, despite treatment advancements.
What is Extranodal T/NK-Cell Lymphoma?
Extranodal T/NK-Cell Lymphoma is a form of non-Hodgkin lymphoma (NHL) which are most of B-cell origin.
What is the Pathology of Extranodal T/NK-Cell Lymphoma?
The pathology of extranodal T/NK-Cell lymphoma is:
-Etiology: The cause of extranodal T/NK-Cell lymphoma is as follow: Acquired immunodeficiency ailments, Inherited immunodeficiencies, autoimmune ailment, association with infectious agents (EBV), and chemical or drug exposures (radiation).
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to extranodal T/NK-Cell lymphoma; Nasal NKTCLs are mostly linked with Epstein-Barr virus (EBV), regardless of the background of the affected population. The precise mechanism of malignant conversion via EBV is not yet clearly clarified.
-Histology: The histology associated with extranodal T/NK-Cell lymphoma shows the presence of a broad cytologic spectrum. Diffuse infiltration of both pleomorphic small and large lymphoma cells, assorted with several inflammatory cells on the necrotic contextual. Cells are with, small nucleoli, pale-to-clear cytoplasm, granular chromatin, and irregular nuclei.
How does Extranodal T/NK-Cell Lymphoma Present?
Patients with extranodal T/NK-Cell lymphoma typically male are more frequently affected with the ailment than females, with a ratio of 3:1. present at age range of the sixth decade. The symptoms, features, and clinical findings associated with extranodal T/NK-Cell lymphoma include: night sweats, weight loss, bone pain, fever, fatigue, facial agony, decreased visual acuity, purulent nasal discharge, orbital swelling, nasal obstruction, refractory sinusitis, nasal septal perforation among others.
How Extranodal T/NK-Cell Lymphoma Diagnosed?
Extranodal T/NK-cell lymphoma is diagnosed thorough medical history and physical exam. Laboratory studies include, liver function tests, complete blood count (CBC), uric acid and calcium levels, renal function tests and Epstein-Barr virus (EBV) titers test. Imaging studies include CT scan and MRI other include nasopharyngoscopy and biopsy.
How is Extranodal T/NK-Cell Lymphoma Treated?
Extranodal T/NK-cell lymphoma is treated Medical care chemotherapy based on tumor cell growth; Antineoplastic agents, Vincristine, Doxorubicin Cyclophosphamide, and Prednisone. Surgical intervention is limited to biopsy, debulking of disease, and the need to stabilization the airway.
What is the Prognosis of Extranodal T/NK-Cell Lymphoma?
The prognosis of extranodal T/NK-cell lymphoma is poor. Multidrug resistance phenotype contributes to low survival rates, low rates of rejoinder to management are secondary to CD56 cell marker.
What is Granulomatous with Polyangiitis (Wegener Granulomatosis)?
Granulomatous with polyangiitis (Wegener granulomatosis) is a multisystem autoimmune amenity of unfamiliar etiology which is rare.
What is the Pathology of is Granulomatous with Polyangiitis (Wegener Granulomatosis)?
The pathology of is granulomatous with polyangiitis (Wegener granulomatosis) is:
-Etiology: The cause of granulomatous with polyangiitis (Wegener granulomatosis) is a type of antineutrophil cytoplasmic antibody–allied vasculitis which largely targets small arteries.
-Genes involved: CTLA-4 (cytotoxic T-lymphocyte antigen 4)
-Pathogenesis: The sequence of events that lead to granulomatous with polyangiitis (Wegener granulomatosis) may characterize some type of hypersensitivity.
-Histology: The histology associated with granulomatous with polyangiitis (Wegener granulomatosis) shows granulomatous vasculitis or necrotizing of small and sometimes larger arteries.
How does Granulomatous with Polyangiitis (Wegener Granulomatosis) Present?
Patients with granulomatous with polyangiitis (Wegener granulomatosis) typically males are affected more often than females present at age range of about 40 years. The symptoms, features, and clinical findings associated with granulomatous with polyangiitis (Wegener granulomatosis) include; mucosal ulcerations of the nasopharynx, persistent pneumonitis with bilateral nodular and cavitary infiltrates, chronic sinusitis, and evidence of renal disease.
How is Granulomatous with Polyangiitis (Wegener Granulomatosis) Diagnosed?
Granulomatous with polyangiitis (Wegener granulomatosis) is diagnosed through a Routine laboratory test: ESR. CBC, LFTs, Biopsy. P-ANCA testing. Imaging studies include sinus radiography and CT scan.
How is Granulomatous with Polyangiitis (Wegener Granulomatosis) Treated?
Granulomatous with polyangiitis (Wegener granulomatosis) is treated through medical care; mainstay medical treatment is an amalgamation of corticosteroids together with cytotoxic agents tailored to treat manifestations. Surgical care is considered in necrosis and damage to subglottic areas, bronchi trachea triggered by fibrosis.
What is the Prognosis of Granulomatous with Polyangiitis (Wegener Granulomatosis)?
The prognosis of granulomatous with polyangiitis (Wegener granulomatosis) is poor, linked with older age, board organ involvement, and board organ damage.
What are Inflammations of the Nasopharynx?
Inflammations of the nasopharynx are frequent co-occurrences of the common viral upper respiratory infections.
Inflammations of the nasopharynx include:
- Pharyngitis
- Tonsillitis
What is Pharyngitis?
Pharyngitis is an inflammation irritation of the pharynx.
What is the Pathology of Pharyngitis?
The pathology of pharyngitis is:
-Etiology: The cause of pharyngitis is usually infectious, with the viral origin and bacterial group A streptococci
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pharyngitis are as follows, bacteria or viruses may directly or indirectly attack the pharyngeal mucosa, triggering a local inflammatory response.
-Histology: The histology associated with pharyngitis shows the presence of inflammatory cells, eosinophils, mast cells, neutrophils. Inflammation of the Nasopharynx which is frequent co-occurrence to common viral upper respiratory infections.
How does Pharyngitis Present?
Patients with pharyngitis typically affect males and females, present at age range of 5 to 24 years with school-aged children 5- 18 years of age typically account for the highest portion. The symptoms, features, and clinical findings associated with pharyngitis include Headache, cough, vomiting, rheumatic fever, tonsillar exudate, anterior cervical lymphadenopathy, conjunctivitis, rhinorrhea, petechiae, petechiae among others.
How is Pharyngitis Diagnosed?
Pharyngitis is diagnosed with a medical history and physical examination. Laboratory studies include GABHS rapid antigen detection test, Throat culture, Peripheral smear, gonococcal culture. Imaging includes soft tissue neck CT scan.
How is Pharyngitis Treated?
Pharyngitis is treated through medical care; corticosteroids are recommended for airway obstruction, antibacterial to prevent complications such as RF.
What is the Prognosis of Pharyngitis?
The prognosis of pharyngitis is good as mortality due to pharyngitis is very rare.
What is Tonsillitis?
Tonsillitis is inflammation of the tonsils secondary to the viral or bacterial agent. Can either be acute or chronic.
What is the Pathology of Tonsillitis?
The pathology of tonsillitis is:
-Etiology: The cause of tonsillitis is Viral and/or bacterial contagions and immunologic aspects.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to tonsillitis include: Viral and or bacterial infections and immunologic aspects that contribute to tonsillitis and its problems. malnourishment and congested conditions do encourage tonsillitis.
-Histology: The histology associated with tonsillitis shows inflammations of the tonsils which are frequent co-occurrences to common viral or bacterial upper respiratory infections.
How does Tonsillitis Present?
Patients with tonsillitis typically more common in males than females present at age range of 5-15 years. The symptoms, features, and clinical findings associated with tonsillitis include: Sore throat, tender cervical lymph nodes, fever, dysphagia, foul breath, mouth breathing, and odynophagia.
How is Tonsillitis Diagnosed?
Tonsillitis is diagnosed through Medical history and physical examination. Laboratory studies: Throat culture, rapid antigen detection test. Imaging studies, lateral neck or CT scans, and ultrasonography.
How is Tonsillitis Treated?
Tonsillitis is treated through medical care largely supportive and suitable hydration, analgesic, antibiotic iv corticosteroid to control pharyngeal edema. Surgical intervention tonsillectomy.
What is the Prognosis of Tonsillitis?
The prognosis of tonsillitis is good mortality related to tonsilitis is rare due to advancement of care.
What is Inflammation of the Larynx?
Inflammation of the larynx is one of the most common laryngeal amenities that usually manifest in acute and chronic forms.
What is Laryngitis?
Laryngitis is inflammation of the larynx.
What is the Pathology of Laryngitis?
The pathology of laryngitis is:
-Etiology: The cause of laryngitis include exposure to noxious agents, vocal misuse, and/ or infectious agents causing upper respiratory tract infections
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to laryngitis is inflamation.
-Histology: The histology associated with laryngitis shows The study of inflammation to the larynx and the vocal fold mucosa.
How does Laryngitis Present?
Patients with laryngitis typically affect both genders though the prevalence is not documented, present at age range of 18-40 years. The symptoms, features, and clinical findings associated with laryngitis include; dysphonia, cough, rhinitis, fever, postnasal discharge, malaise, congestion, fatigue, and sore throat.
How is Laryngitis Diagnosed?
Laryngitis is diagnosed thorough medical history and physical examination. Imaging, indirect laryngoscopy.
How is Laryngitis Treated?
Laryngitis is treated through conversive measures. No medical treatment is needed, advice on complete voice rest, humidified air inhaling, cessation of smoking, and dietary modification such as caffeine avoidance.
What is the Prognosis of Laryngitis?
The prognosis of laryngitis is good as it is self-limited and with conservative measures mortality is rare.
What are Tumors of the Nasopharynx?
Tumors of the nasopharynx are benign or malignant condition affecting the nasopharynx.
Note that these tumors may also occur in the nose or sinuses.
Examples of tumors of the nasopharynx include:
- Nasopharyngeal angiofibroma
- Sinonasal (Schneiderian) papilloma
- Nasopharyngeal carcinoma
- NUT midline carcinoma
- Olfactory neuroblastoma aka esthesioneuroblastoma
What is a Nasopharyngeal Angiofibroma?
Nasopharyngeal angiofibroma is a peculiar tumor that occurs entirely in adolescent males (10-20 years of age) suggesting the role of testosterone hormone in its production.
What is the Pathology of Nasopharyngeal Angiofibroma?
The pathology of nasopharyngeal angiofibroma is:
-Etiology: The cause of nasopharyngeal angiofibroma is hormonal theory testosterone proposed and also suggested nonchromaffin paraganglionic cells.
-Genes involved: adenomatous polyposis coli (APC) gene.
-Pathogenesis: The sequence of events that lead to nasopharyngeal angiofibroma is: Starts next to the sphenopalatine foramen. Frontal growth occurs beneath the nasopharyngeal mucous membrane, relocating it anteriorly, inferiorly to the postnasal space. Nasal cavity filled on one side deviating septum to the other side.
-Histology: The histology associated with nasopharyngeal angiofibroma shows numerous small endothelium-lined vascular spaces and the stromal cells which are myofibroblasts.
How does Nasopharyngeal Angiofibroma Present?
Patients with nasopharyngeal angiofibroma typically affect young males present at age range of 10-28years. The symptoms, features, and clinical findings associated with nasopharyngeal angiofibroma include proptosis, orbital mass, nasal obstruction, facial swelling, epistaxis, and nasal mass.
How is Nasopharyngeal Angiofibroma Diagnosed?
Nasopharyngeal angiofibroma is diagnosed through Plain radiography views of the sinuses, Magnetic resonance imaging (MRI), and CT scan.
How is Nasopharyngeal Angiofibroma Treated?
Nasopharyngeal angiofibroma is treated through medical therapy hormonal therapy or surgery.
What is the Prognosis of Nasopharyngeal Angiofibroma?
The prognosis of nasopharyngeal angiofibroma is good under proper management.
What is a Sinonasal (Schneiderian) Papilloma?
Sinonasal (Schneiderian) papilloma is a benign infiltrative epithelial neoplasm arising from ectodermal derived pseudostratified ciliated epithelium which covers the nasal cavity and sinonasal tract.
What is the Pathology of Sinonasal (Schneiderian) Papilloma?
The pathology of sinonasal (Schneiderian) papilloma is:
-Etiology: The cause of sinonasal (Schneiderian) papilloma is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to sinonasal (Schneiderian) papilloma…
-Histology: The histology associated with sinonasal (Schneiderian) papilloma shows fungiform type composed of thick squamous epithelium, less frequently, respiratory epithelium organized in papillary fronds with an exophytic type of growth. the study of finger-like epithelial proliferations benign neoplasms that originate in the sinonasal tract.
How does Sinonasal (Schneiderian) Papilloma Present?
Patients with sinonasal (Schneiderian) papilloma typically Men are affected 4 times more often than women, present at age range of 6-90 years old. The symptoms, features, and clinical findings associated with sinonasal (Schneiderian) papilloma include Unilateral polypoidal mass filling and nasal obstruction, nasal discharge, epistaxis, epiphora, and facial agony.
How is Sinonasal (Schneiderian) Papilloma Diagnosed?
Sinonasal (Schneiderian) papilloma is diagnosed through imaging study preoperative radiographic assessment, CT scanning, and MRI, laboratory work, biopsy.
How is Sinonasal (Schneiderian) Papilloma Treated?
Sinonasal (Schneiderian) papilloma is treated through medical therapy for sinusitis complications.
What is the Prognosis of Sinonasal (Schneiderian) Papilloma?
The prognosis of sinonasal (Schneiderian) papilloma is fair with proper management.
What is a Nasopharyngeal Carcinoma?
Nasopharyngeal carcinoma is a tumor is categorized by a typical geographic distribution, in anatomic association to lymphoid tissue.
What is the Pathology of Nasopharyngeal Carcinoma?
The pathology of nasopharyngeal carcinoma is:
-Etiology: The cause of nasopharyngeal carcinoma is the environmental factors and infection with Epstein‐Barr virus.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to nasopharyngeal carcinoma proliferation of malignant cells.
-Histology: The histology associated with nasopharyngeal carcinoma shows non-keratinizing squamous cell carcinoma and undifferentiated carcinoma.
How does Nasopharyngeal Carcinoma Present?
Patients with nasopharyngeal carcinoma typically the male-to-female ratio is approximately 2:1 present at age range of 50-60 years. The symptoms, features, and clinical findings associated with nasopharyngeal carcinoma include bleeding, nasal obstruction, and nasal discharge. Ear infection, and tinnitus. Neck swelling and headaches.
How is Nasopharyngeal Carcinoma Diagnosed?
Nasopharyngeal carcinoma is diagnosed through Laboratory studies: Complete blood cell count, Epstein-Barr virus titers. chemistry profile. Imaging; positron emission tomography imaging, magnetic resonance imaging, CT scanning, bone scans.
How is Nasopharyngeal Carcinoma Treated?
Nasopharyngeal carcinoma is treated through medical care, radiation, and chemotherapy. Surgical intervention is limited to a biopsy tissue analysis.
What is the Prognosis of Nasopharyngeal Carcinoma?
The prognosis of nasopharyngeal carcinoma is fair as those treated with radiotherapy have a 40-50% survival rate.
What is NUT Midline Carcinoma?
NUT Midline Carcinoma is an erratic and aggressive carcinoma categorized by chromosomal reorganization occurring most frequently in the mediastinum.
What is the Pathology of NUT Midline Carcinoma?
The pathology of NUT midline carcinoma is:
-Etiology: The cause of NUT midline carcinoma is believed to be gene rearrangement.
-Genes involved: MYC, MED24, and p63 genes.
-Pathogenesis: The sequence of events that lead to NUT midline carcinoma is not well understood as it is diagnosed at a late stage.
-Histology: The histology associated with NUT midline carcinoma shows an ill differentiated carcinoma which has a habit to be pleomorphic.
How does NUT Midline Carcinoma Present?
Patients with NUT midline carcinoma typically have no substantial gender difference, present at age range of 5-15years. The symptoms, features, and clinical findings associated with NUT midline carcinoma include Cough, pain, fatigue, shortness of breath, and weight loss.
How is NUT Midline Carcinoma Diagnosed?
NUT midline carcinoma is diagnosed by Laboratory studies: Testing a monoclonal antibody to NUT (C52B1) with immunohistochemical (IHC) nuclear staining. Imaging studies: Digital radiography, CT scans, and positron emission tomography.
How is NUT Midline Carcinoma Treated?
NUT midline carcinoma is treated traditionally through radiotherapy and complete tumor resection through effective plans is still in research.
What is the Prognosis of NUT Midline Carcinoma?
The prognosis of NUT midline carcinoma is poor since it is diagnosed at a late stage, and no effective treatment is yet known.
What is an Olfactory Neuroblastoma aka Esthesioneuroblastoma?
Olfactory Neuroblastoma aka Esthesioneuroblastoma is rare, highly malignant tumor composing small round cells similar to neuroblasts thriving into lobular nests which are surrounded by vascularized connective tissue.
What is the Pathology of Olfactory Neuroblastoma aka Esthesioneuroblastoma?
The pathology of olfactory neuroblastoma aka esthesioneuroblastoma is:
-Etiology: The cause of olfactory neuroblastoma aka esthesioneuroblastoma is, has no clear exposure or etiologic agent
-Genes involved: Drosophila achaete-scute gene (hASH1).
-Pathogenesis: The sequence of events that lead to olfactory neuroblastoma aka esthesioneuroblastoma. Tumor cells are mitotically dynamic and they are forerunner cells that progress into neuronal and sustentacular cells.
-Histology: The histology associated with olfactory neuroblastoma aka esthesioneuroblastoma shows neoplastic cells displaying more diffuse growth patterns, cytological atypia of the neoplastic cells. The neuroblasts that rise mostly superiorly, laterally of the nose from the neuroendocrine cells disseminated at the olfactory mucosa.
How does Olfactory Neuroblastoma aka Esthesioneuroblastoma Present?
Patients with olfactory neuroblastoma aka esthesioneuroblastoma typically mark males and females similarly present at age range of 3-90years. The symptoms, features, and clinical findings associated with olfactory neuroblastoma aka esthesioneuroblastoma include Nasal discharge, obstruction, unilateral polyp, epistaxis, anosmia, paralysis of extraocular movement, and blindness headache, cervical – mass, nausea.
How is Olfactory Neuroblastoma aka Esthesioneuroblastoma Diagnosed?
Olfactory neuroblastoma aka esthesioneuroblastoma is diagnosed by biopsy.
How is Olfactory Neuroblastoma aka Esthesioneuroblastoma Treated?
Olfactory neuroblastoma aka esthesioneuroblastoma is treated through chemotherapy, radiation. Surgical, endoscopic craniofacial resection.
What is the Prognosis of Olfactory Neuroblastoma aka Esthesioneuroblastoma?
The prognosis of olfactory neuroblastoma aka esthesioneuroblastoma good though a subset displays recurrence, advanced and/or metastatic ailment, requiring additional management.
What are Vocal Cord Nodules?
Vocal cord nodules are confined, benign, shallow growths on the median surface to the vocal folds believed to originate from phonotrauma. Vocal cord nodules are also called reactive polyps, vocal cord polyps, and singers’ nodules.
What is the Pathology of Vocal Cord Nodules?
The pathology of vocal cord nodules is:
-Etiology: The cause of vocal cord nodules is believed to be vocal trauma.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to vocal cord nodules: imperfect dorsal vocal fold adduction, muscular exhaustion, and subsequent hypotonia augment curving. Augmented subglottal pressure by a reduction in active stress forces between the adjacent vocalis masses causes a localized impact.
-Histology: The histology associated with vocal cord nodules shows a condensed basement membrane zone and also a dense fibronectin arrangement to the superficial lamina propria.
How does Vocal Cord Nodules Present?
Patients with vocal cord nodules typically advanced in females than males present at age range of below 19years, they are likely to misuse and abuse voice. The symptoms, features, and clinical findings associated with vocal cord nodules include general and tenacious hoarseness, alteration in voice eminence, and augmented effort in constructing the voice, bilateral or unilateral lesions and polyps.
How is Vocal Cord Nodules Diagnosed?
Vocal cord nodules are diagnosed through high-resolution ultrasonography.
How is Vocal Cord Nodules Treated?
Vocal cord nodules treated through medical care steroid injection, submucosal triamcinolone acetonide injections. |Surgical intervention, phonosurgical methods to remove benign lesions. Others include vocal hydration, hygiene, and evading vocal abuse and misuse.
What is the Prognosis of Vocal Cord Nodules?
The prognosis of vocal cord nodules is good with appropriate treatment.
What is Squamous Papilloma of the Larynx?
Squamous papilloma of the larynx is a benign lesion triggered by a viral contagion of epithelial cells causing overgrowth in different parts of the respiratory tract.
What is the Pathology of Squamous Papilloma of the Larynx?
The pathology of squamous papilloma of the larynx is:
-Etiology: The cause of squamous papilloma of the larynx is the human papillomavirus (HPV).
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to squamous papilloma of the larynx though the exact mode of HPV transmission is indistinct, studies designate that childhood-onset recurrent respiratory papillomatosis happens during exposure of upper aerodigestive tract of the child to the cervix and vagina of a mother with HPV infection throughout delivery.
-Histology: The histology associated with squamous papilloma of the larynx shows finger-like papillae, each papilla contains fibrovascular core covered by stratified squamous epithelium.
How does Squamous Papilloma of the Larynx Present?
Patients with squamous papilloma of the larynx typically the male-to-female ratio is 4:1. present at age range of 20-40 years. The symptoms, features, and clinical findings associated with squamous papilloma of the larynx include feeding difficulties, vocal abuse, allergic rhinitis, tachypnea, use of accessory muscles, stridor, stridor, and reflux irritation.
How is Squamous Papilloma of the Larynx Diagnosed?
Squamous papilloma of the larynx is diagnosed through: Laboratory work, biopsies for histologic evaluation Imaging Studies, bronchoscopy, and nasopharyngoscopy.
How is Squamous Papilloma of the Larynx Treated?
Squamous papilloma of the larynx is treated through medical therapies, interferon. Photodynamic therapies, Intralesional therapies. Surgical intervention, excision using carbon dioxide lasers.
What is the Prognosis of Squamous Papilloma of the Larynx?
The prognosis of squamous papilloma of the larynx is good since the condition is a benign lesion.
What are Tumors of the Larynx?
Tumors of the larynx are lesions that are both benign and malignant tumors.
Examples of tumors of the larynx include:
- Inverting papilloma
- Adenocarcinoma
- Squamous cell carcinoma
- Melanoma
What is an Inverting Papilloma of the Larynx?
Inverting papilloma of the larynx is a benign tumor generally affecting squamous and ciliated epithelial to the larynx.
What is the Pathology of Inverting Papilloma of the Larynx?
The pathology of inverting papilloma of the larynx is:
-Etiology: The cause of inverting papilloma of the larynx is: Chronic inflammation, HPV, tumor suppressor gene p53 alterations.
-Genes involved: Tumor suppressor gene p53.
-Pathogenesis: The sequence of events that lead to inverting papilloma of the larynx, transpires at the histologic and molecular level. Molecular phases tangled in tumorigenesis not fully elucidated. Histologic advancement arises from typical laryngeal mucosa to dysplastic mucosa, carcinoma in situ culminating to invasive carcinoma.
-Histology: The histology associated with inverting papilloma of the larynx shows digitiform propagation to the squamous epithelium in the basal stroma.
How does Inverting Papilloma of the Larynx Present?
Patients with inverting papilloma of the larynx typically affect more males than females present at age range of 50-69 years. The symptoms, features, and clinical findings associated with inverting papilloma of the larynx include: Nasal obstruction, epistaxis and dysphagia, dysphonia tachypneic, stridulous, and suprasternal retraction.
How is Inverting Papilloma of the Larynx Diagnosed?
Inverting papilloma of the larynx is diagnosed through imaging, bronchoscopy.
How is Inverting Papilloma of the larynx Treated?
Inverting papilloma of the larynx is treated through surgical intervention, accompanied with postoperative radiotherapy if linked to malignancy.
What is the Prognosis of Inverting Papilloma of the Larynx?
The prognosis of inverting papilloma of the larynx is good after successful treatment.
What is an Adenocarcinoma of the Larynx?
Adenocarcinoma of the larynx is rarely seen and presumably arising from mucous glands.
What is the Pathology of Adenocarcinoma of the Larynx?
The pathology of adenocarcinoma of the larynx is:
-Etiology: The cause of adenocarcinoma of the larynx is, HPV, nicotine uses, and alcohol consumption.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to adenocarcinoma of the larynx, transpires at the histologic and molecular level. Molecular phases tangled in tumorigenesis not fully elucidated. Histologic advancement arises from typical laryngeal mucosa to dysplastic mucosa, carcinoma in situ culminating to invasive carcinoma.
-Histology: The histology associated with adenocarcinoma of the larynx shows squamous cell carcinomas of the larynx follow the growth pattern of all squamous cell carcinomas.
How does Adenocarcinoma of the larynx Present?
Patients with adenocarcinoma of the larynx typically have a male-to-female ratio of 4:1. present at age range of 50 to 70 years. The symptoms, features, and clinical findings associated with adenocarcinoma of the larynx include: Dysphonia/aphonia, cachexia dysphagia, pain, dyspnea, halitosis, aspiration, expectoration of tissue, blood-tinged sputum, neck mass, fatigue, otalgia, weight loss, and weakness
How is Adenocarcinoma of the larynx Diagnosed?
Adenocarcinoma of the larynx is diagnosed through: Laboratory studies; Arterial blood gas analysis, platelet count, thyroid function test. Imaging studies; CT scan, plain chest radiography. PET-CT scan (Positron emission tomography-computerized tomography) may also be useful.
How is Adenocarcinoma of the larynx Treated?
Adenocarcinoma of the larynx is treated often by radical surgery, adjuvant radiotherapy, and chemotherapy. There is no harmony regarding its treatment and augmented recurrence.
What is the Prognosis of Adenocarcinoma of the larynx?
The prognosis of adenocarcinoma of the larynx is poor as there is no harmony regarding its treatment.
What is a Squamous Cell Carcinoma of the Larynx?
Squamous cell carcinoma of the larynx is a malignant tumor that accounts for 95% of laryngeal malignancies.
What is the Pathology of Squamous Cell Carcinoma?
The pathology of squamous cell carcinoma is:
-Etiology: The cause of squamous cell carcinoma is, HPV, alcohol use, cigarette smoking, and infection with Epstein–Barr.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to squamous cell carcinoma; transpires at the histologic and molecular levels. Molecular phases tangled in tumorigenesis not fully elucidated. Histologic advancement arises from typical laryngeal mucosa to dysplastic mucosa, carcinoma in situ culminating to invasive carcinoma.
-Histology: The histology associated with squamous cell carcinoma shows, hyperchromatic cells, squamous cell carcinoma of high grade.
How does Squamous Cell Carcinoma Present?
Patients with squamous cell carcinoma typically affect more males than females present at age range of 55 to75 years. The symptoms, features, and clinical findings associated with squamous cell carcinoma include, Hoarseness, blood-tinged sputum cachexia dysphagia, pain, dyspnea, halitosis, aspiration, expectoration of tissue, neck mass, fatigue, otalgia, weight loss, and weakness.
How is Squamous Cell Carcinoma Diagnosed?
Squamous cell carcinoma is diagnosed through Laboratory studies, biopsy, arterial blood gas analysis, platelet count, thyroid function test. Imaging studies; CT scan, and plain chest radiography.
How is Squamous Cell Carcinoma Treated?
Squamous cell carcinoma is treated through radical surgery, adjuvant radiotherapy, and chemotherapy.
What is the Prognosis of Squamous Cell Carcinoma?
The prognosis of squamous cell carcinoma is poor because it is not recognized and treated when small and early.
What is a Melanoma of the Larynx?
Melanoma of the larynx is is an extremely very erratic, aggressive neoplasm of melanocytic origin with very little known about it.
What is the Pathology of Melanoma of the Larynx?
The pathology of melanoma of the larynx is:
-Etiology: The cause of melanoma of the larynx is poorly unstated though tobacco use and formaldehyde exposure are suggested.
-Genes involved: BRAF mutation.
-Pathogenesis: The sequence of events that lead to melanoma of the larynx not yet known.
-Histology: The histology associated with melanoma of the larynx shows the tumor consisting of polygonal-epithelioid cells, spindle-shaped and elongated cells. Most cells establish dark-brown cytoplasmic also nuclear melanin. Noticeable abnormal mitoses and pleomorphism were noted.
How does Melanoma of the Larynx Present?
Patients with melanoma of the larynx typically have equal gender distribution, preset at age range of 20- 80 years. The symptoms, features, and clinical findings associated with melanoma of the larynx include sore throat, Hoarseness, and sporadic breathing difficulties. Dark color masses on the epiglottis.
How is Melanoma of the Larynx Diagnosed?
Melanoma of the larynx is diagnosed through immunohistochemical and histopathologic examination.
How is Melanoma of the larynx Treated?
Melanoma of the larynx is treated through laryngeal lesions, a total surgical excision, and postoperative radiation therapy.
What is the Prognosis of Melanoma of the Larynx?
The prognosis of melanoma of the larynx is poor since the lesion remains inactive for a long.