Pancreas pathology is the study of significant disorders of the pancreas that affect its endocrine, exocrine functions and alter its anatomy. Pancreas pathology may be endocrine or exocrine related.
What is Exocrine Pancreas Pathology?
Exocrine pancreas pathology is an abnormal change in function and structure to the pancreas that results from pancreatic inflammations, neoplasm, and duct obstruction.
Exocrine pancreas pathology includes:
- Congenital anomalies of the pancreas
- Pancreatitis
- Non-neoplastic pancreatic cysts
- Neoplasms
What are Congenital Anomalies of the Pancreas?
Congenital anomalies of the pancreas are the abnormal functions and structure of the pancreas that develop during the complex process by which the dorsal and ventral pancreatic primordia fuse during pancreatic development.
Examples of congenital anomalies of the pancreas include:
- Agenesis of the pancreas
- Annular pancreas
- Ectopic pancreas
- Pancreas divisum
What is Agenesis of the Pancreas?
Agenesis of the pancreas is a very rare condition in which the is a total absence of the pancreas.
What is the Pathology of Agenesis of the Pancreas?
The pathology of agenesis of the pancreas is due to an absence of pancreas.
-Etiology: The cause of agenesis of the pancreas is the mutation in the IPF1 gene on chromosome 13q12.1.
-Genes involved: IPF1 gene
-Pathogenesis: The sequence of events that lead to agenesis of the pancreas is atypical embryogenesis due to developmental failure of the dorsal pancreas and the mutation in the IPF1 gene on chromosome 13q12.1. This resultis in the complete or partial absence of the pancreas.
-Morphology: The morphology associated with agenesis of the pancreas shows partial or complete absence of pancreas.
-Histology: None.
How does the Agenesis of the Pancreas Present?
Patients with agenesis of the pancreas are typically rare present at the age range of neonatal and infant. The symptoms, features, and clinical findings associated with agenesis of the pancreas include pancreatitis, epigastric pain, diabetes mellitus, and hyperglycemia in a minority group. It is generally asymptomatic in most cases.
How is Agenesis of the Pancreas Diagnosed?
Agenesis of the pancreas is diagnosed via ultrasonographic imaging (USG), endoscopic ultrasound (EUS), magnetic resonance (MR), and computed tomography (CT).
How is Agenesis of the Pancreas Treated?
Agenesis of the pancreas is treated through the management of Diabetes and exocrine deficiency.
What is the Prognosis of Agenesis of the Pancreas?
The prognosis of agenesis of the pancreas is fair depending on the quality of treatment.
What is Annular Pancreas?
Annular pancreas is an uncommon congenital anomaly characterized by encasement of the duodenum by a band of pancreatic tissue.
What is the Pathology Annular Pancreas?
The pathology of annular pancreas is:
-Etiology: The cause of annular pancreas is well understood, linked to the embryological anomaly. One portion of the ventral pancreatic primordium becomes static, while the other part of primordium is drawn around the duodenum.
-Genes involved: Transmembrane 4 superfamily member 3 (tm4sf3)
-Pathogenesis: The sequence of events that lead to annular pancreas is anticipated to be a migration anomaly ensuing from ventral bud failure to rotate and extend to sheath the second portion of the duodenum partially or completely.
-Morphology: The morphology associated with annular pancreas shows it can be divided into intramural and extramural types grounded on the existence of pancreatic tissue in the duodenal wall.
-Histology: The histology associated with annular pancreas shows numerous pancreatic polypeptide (PP) cells of ventral pancreatic anlage organized in sporadically shaped islets.
How does Annular Pancreas Present?
Patients with annular pancreas typically have a slight male preponderance present at age range of infancy to adulthood. The symptoms, features, and clinical findings associated with annular pancreas include non-bilious vomiting, feeding intolerance, and bloating, in infants. Duodenal obstruction, pancreatitis, and abdominal pain in adults.
How is Annular Pancreas Diagnosed?
Annular pancreas is diagnosed through radiological(CT scan, MRI, magnetic resonance cholangiopancreatography (MRCP)) and clinical manifestations.
How is Annular Pancreas Treated?
Annular pancreas is treated through individual management of the symptoms, surgical management (duodenal bypass procedures) commonly in children.
What is the Prognosis of Annular Pancreas?
The prognosis of annular pancreas is good in children with overall survival rates and is fair in adults.
What is Ectopic Pancreas?
Ectopic pancreas is a condition in which pancreatic tissues are found in places other than the normal anatomical position.
What is the Pathology of Ectopic Pancreas?
The pathology of ectopic pancreas is:
-Etiology: The cause of ectopic pancreas is abnormal embryologic development.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to ectopic pancreas is persistence of a duodenal evagination intricated in the typical growth of the pancreas. The remnant travels with the developing gastrointestinal tract resulting in its numerous locations.
-Morphology: The morphology associated with ectopic pancreas shows existence of a characteristic central ductal orifice.
-Histology: The histology associated with ectopic pancreas shows the presence of islets of Langerhans, pancreatic acini.
How does Ectopic Pancreas Present?
Patients with ectopic pancreas are usually males. The symptoms, features, and clinical findings associated with ectopic pancreas include sessile mass, may cause pain from localized inflammation, or, rarely, may incite mucosal bleeding, anemia, melena abdominal fullness, and nausea.
How is Ectopic Pancreas Diagnosed?
Ectopic pancreas is diagnosed through radiological study (Endoscopic ultrasonography (EUS ) and clinical presentations.
How is Ectopic Pancreas Treated?
Ectopic pancreas is treated through surgical interventions laparoscopic wedge resection.
What is the Prognosis of Ectopic Pancreas?
The prognosis of ectopic pancreas is good, with proper management.
What is Pancreas Divisum?
Pancreas divisum is a fusional anomaly of the ductal systems of the dorsal and ventral buds of the embryonic pancreas during the seventh week of intrauterine life.
What is the Pathology of Pancreas Divisum?
The pathology of pancreas divisum is:
-Etiology: The cause of pancreas divisum is congenital fusion failure of the dorsal and ventral buds ducts.
-Genes involved: CFTR gene
-Pathogenesis: The sequence of events that lead to pancreas divisum caused a failure of the ducts of the dorsal and ventral buds to fuse throughout embryologic growth, at around the 8th week of intrauterine life.
-Morphology: None.
-Histology: No difference between normal pancreatic tissue, acini and ductules.
How does Pancreas Divisum Present?
Patients with pancreas divisum typically slightly high in females present at age range of between infancy and adulthood. The symptoms, features, and clinical findings associated with pancreas divisum include epigastric tenderness. palpable pseudocyst, abdominal pain, and pancreatitis.
How is Pancreas Divisum Diagnosed?
Pancreas divisum is diagnosed through radiological study- endoscopic retrograde cholangiopancreatography (ERCP), CT scan, magnetic resonance cholangiopancreatography (MRCP), and clinical presentations.
How is Pancreas Divisum Treated?
Pancreas divisum is treated through surgical intervention sphincteroplasty, and minor papilla sphincterotomy. Medical management of symptoms may be utilized.
What is the Prognosis of Pancreas Divisum?
The prognosis of pancreas divisum is good with appropriate management.
What is Pancreatitis?
Pancreatitis is a group of ailments categorized by inflammation of the pancreas
Examples of pancreatitis include:
- Acute Pancreatitis
- Chronic Pancreatitis
What is Acute Pancreatitis?
Acute pancreatitis is a group of reversible lesions characterized by inflammation of the pancreas with severity ranging from edema, fat necrosis to parenchymal necrosis with severe hemorrhage.
What is the Pathology of Acute Pancreatitis?
The pathology of acute pancreatitis is:
-Etiology: The cause of acute pancreatitis is biliary tract disease, drugs, trauma, alcoholism, infectious, and post-ERCP.
-Genes involved: Cationic Trypsinogen (PRSS1), CFTR gene
-Pathogenesis: The sequence of events that lead to acute pancreatitis; injures the acinar cell and impairs the secretion of zymogen granules, believed that both extracellular factors and intracellular factors play a role. Also results from ductal cell injury which leads to the absence or delayed enzymatic secretion. Acute pancreatitis is an inflammatory process by which there is autodigest gland by pancreatic enzymes. The gland may restore without any loss of function or any morphologic variations.
-Morphology: The morphology associated with acute pancreatitis shows interstitial edema.
-Histology: The histology associated with acute pancreatitis shows inflammatory infiltrate hemorrhage and necrosis.
How does Acute Pancreatitis Present?
Patients with acute pancreatitis are typically more common in males present at an age range of 35-75 years. The symptoms, features, and clinical findings associated with acute pancreatitis include abdominal pain, nausea, and vomitting.
How is Acute Pancreatitis Diagnosed?
Acute pancreatitis is diagnosed through laboratory studies- raised serum amylase and lipase levels, BUN, creatinine, serum electrolytes, cholesterol, glucose, and triglycerides. A 48 hour C-reactive protein (CRP) value. Radiological studies- abdominal ultrasonography, endoscopic ultrasonography, abdominal CT scan, magnetic resonance cholangiopancreatography (MRCP), and endoscopic retrograde cholangiopancreatography (ERCP).
How is Acute Pancreatitis Treated?
Acute pancreatitis is treated through medical care, antibiotic therapy, fluid resuscitation. Surgical intervention and nutritional support may be needed.
What is the Prognosis of Acute Pancreatitis?
The prognosis of acute pancreatitis is fair with an overall mortality of 15%.
What is Chronic Pancreatitis?
Chronic pancreatitis is a condition pancreas characterized by inflammation with irreversible destruction of exocrine parenchyma, and in the late stages, the destruction of endocrine parenchyma.
What is the Pathology of Chronic Pancreatitis?
The pathology of chronic pancreatitis is:
-Etiology: The cause of chronic pancreatitis is long-term alcohol abuse, long-standing obstruction, hereditary pancreatitis, and idiopathic chronic pancreatitis.
-Genes involved: PRSS1 gene.
-Pathogenesis: The sequence of events that lead to chronic pancreatitis is not well defined, and may involve ductal obstruction, toxins, oxidative stress, and necrosis. The inflammation of the pancreas, may present as repeated bouts of acute pancreatitis, the main distinction to acute pancreatitis is the irreversible impairment in the pancreatic function that is characteristic of chronic pancreatitis.
-Histology: The histology associated with chronic pancreatitis shows parenchymal fibrosis, reduced number, and size of acini. There may be relative sparing of the islets of Langerhans.
How does Chronic Pancreatitis Present?
Patients with chronic pancreatitis are typically common in males than females present at an age range of 35 to 45years. The symptoms, features, and clinical findings associated with chronic pancreatitis include moderately severe abdominal pain, back pain, jaundice.
How is Chronic Pancreatitis Diagnosed?
Chronic pancreatitis is diagnosed through the clinical presentation, ultrasonography, CT scan- evidence of calcifications.
How is Chronic Pancreatitis Treated?
Chronic pancreatitis is treated through medical care, analgesics, fluid management.
What is the Prognosis of Chronic Pancreatitis?
The prognosis of chronic pancreatitis is poor with a 20 to 25 year mortality rate of 50%.
What are Non-neoplastic Pancreatic Cysts?
Non-neoplastic pancreatic cysts are unilocular cysts that tend to be benign lesions of the pancres.
Examples of non-neoplastic pancreatic cysts include:
- Congenital pancreatic cysts
- Pancreatic pseudocysts
What are Congenital Pancreatic Cysts?
Congenital pancreatic cysts are anomalies believed to result from anomalous development of the pancreatic ducts characterized by thin-walled unilocular cysts.
What is the Pathology of Congenital Pancreatic Cysts?
The pathology of congenital pancreatic cysts is: The study of a lesion lined by a glistening, duct-type cuboidal epithelium/completely attenuated cell layer. Cyst enclosed in a thin, fibrous capsule filled with a clear-to-turbid mucoid/serous fluid.
-Etiology: The cause of congenital pancreatic cysts is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to congenital pancreatic cysts not clearly understood, and is likely multifactorial.
-Morphology: The morphology associated with congenital pancreatic cysts shows fibrous capsules and are filled with a clear-to-turbid mucoid or serous fluid.
-Histology: The histology associated with congenital pancreatic cysts shows cuboidal epithelium or by a completely attenuated cell layer.
How do Congenital Pancreatic Cysts Present?
Patients with congenital pancreatic cysts typically have a female to male ratio of 4:1 present at an age range of <10 years. The symptoms, features, and clinical findings associated with congenital pancreatic cysts include acholic stools in infants, recurring attacks of pancreatitis, jaundice, colicky abdominal pain, right upper quadrant mass, and cholangitis.
How are Congenital Pancreatic Cysts Diagnosed?
Congenital pancreatic cysts is diagnosed through radiological studies- abdominal ultrasonography, ct scan, MRI, and endoscopic ultrasonography (EUS).
How is Congenital Pancreatic Cysts Treated?
Congenital pancreatic cysts is may be left alone or treated with FNA and surgical excision depending on the size and type of cyst.
What is the Prognosis of Congenital Pancreatic Cysts?
The prognosis of congenital pancreatic cysts is generally good.
What are Pancreatic Pseudocysts?
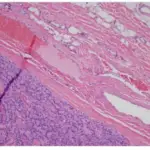
Pancreatic pseudocysts are cysts of the pancreas that are characterized by localized collections of hemorrhagic and necrotic material that lack an epithelial lining.
What is the Pathology of Pancreatic Pseudocysts?
The pathology of pancreatic pseudocysts is: Study of localized fluid collections of hemorrhagic and necrotic material, having a nonepithelialized wall be made up of fibrous and granulation tissue, and generally appears weeks after onset of pancreatitis.
-Etiology: The cause of pancreatic pseudocysts is include acute pancreatitis and pancreatic trauma.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pancreatic pseudocysts stem from interruptions to the pancreatic duct owing to pancreatitis and eructation of the enzymatic material.
-Morphology: The morphology associated with pancreatic pseudocysts shows varying sizes of 2 to 30 cm diameter sac.
-Histology: The histology associated with pancreatic pseudocysts shows zones of peripancreatic hemorrhagic fat necrosis and fibrous tissue. Pancreatic pseudocysts are characterized by localized collections of hemorrhagic and necrotic material that lack an epithelial lining.
How does Pancreatic Pseudocysts Present?
Patients with pancreatic pseudocysts typically have a male predominance present at an age range of any age group. The symptoms, features, and clinical findings associated with pancreatic pseudocysts include Fever, scleral icterus, pleural effusion a tender abdomen.
How is Pancreatic Pseudocysts Diagnosed?
Pancreatic pseudocysts is diagnosed through laboratory study- amylase and lipase levels elevated. Abdominal ultrasonography, abdominal computed tomography (CT) scan.
How is Pancreatic Pseudocysts Treated?
Pancreatic pseudocysts is treated through medical care-antibiotic therapy, somatostatin analogues, and octreotide. Surgical intervention which may involve catheter drainage, endoscopic drainage may be utilized.
What is the Prognosis of Pancreatic Pseudocysts?
The prognosis of pancreatic pseudocysts is good as most cases resolve without interference.
What are Pancreatic Neoplasms?
Pancreatic neoplasms are fluid-filled sacs (cysts) or solid within the pancreas which may benign or malignant.
Examples of pancreatic neoplasms include:
- Acinar cell carcinoma
- Pancreatic carcinoma aka ductal carcinoma of the pancreas
- Pancreatoblastoma
- Pancreatic intraepithelial neoplasia (PanIN)
- Cystic neoplasms
What is Acinar Cell Carcinoma?
Acinar cell carcinoma is an epithelial neoplasm defined by its morphologic similarity to acinar cells and the secretion of pancreatic exocrine enzymes.
What is the Pathology of Acinar Cell Carcinoma?
The pathology of acinar cell carcinoma is: The study of an infrequent tumor, accounting for only approximately 1 % of all pancreatic tumors, is solid and malignant though benign may exist (acinar cell cystadenocarcinoma).
-Etiology: The cause of acinar cell carcinoma is defective DNA repair, tobacco smoking.
-Genes involved: K-RAS gene.
-Pathogenesis: The sequence of events that lead to acinar cell carcinoma are a result of accretion of genetic modification, counting chromosomal variability, and recurrent allelic copy number disparity.
-Morphology: The morphology associated with acinar cell carcinoma shows pyramidal cells clustered around small lumina, large around 10 cm in diameter carcinomas.
-Histology: The histology associated with acinar cell carcinoma shows circumscribed multinodular. Soft nodules, yellow to brown, central necrosis, and cystic degeneration.
How does Acinar Cell Carcinoma Present?
Patients with acinar cell carcinoma typically have a male to female ratio of 3.6:1 present at an age range of 20 to 40 years. The symptoms, features, and clinical findings associated with acinar cell carcinoma include idiopathic weight loss, abdominal pain, generalized weakness, diarrhea, melena, nausea, and vomiting.
How is Acinar Cell Carcinoma Diagnosed?
Acinar cell carcinoma is diagnosed through laboratory study- elevated serum lipase levels. Radiological studies- CT scan and MRI disclose well-defined, hefty oval masses. Fine-needle aspiration biopsy- discloses cells portrayal degrees of acinar differentiation.
How is Acinar Cell CarcinomaTreated?
Acinar cell carcinoma is treated through, surgical resection, chemotherapy, and radiation therapy.
What is the Prognosis of Acinar Cell Carcinoma?
The Prognosis of acinar cell carcinoma is poor. It is highly aggressive with an overall 5 year survival rate of <10%.
What is Pancreatic Carcinoma aka ductal carcinoma of the pancreas?
Pancreatic carcinoma aka ductal carcinoma of the pancreas is a highly aggressive lethal malignancy due to the lack of early diagnosis and limited response to treatments.
What is the Pathology of Pancreatic Carcinoma?
The pathology of pancreatic carcinoma is:
-Etiology: The cause of pancreatic carcinoma is smoking, a diet rich in fats, chronic pancreatitis, obesity, alcohol consumption.
-Genes involved: K-RAS gene, SMAD4 gene, p53 tumor suppressor gene
-Pathogenesis: The sequence of events that lead to pancreatic carcinoma; arise from the exocrine and endocrine part of the pancreas, smoking, thought to twofold the risk of pancreatic tumor, diabetes mellitus, and pancreatitis are associated with an increased risk of pancreatic tumor. There is also familial clustering to pancreatic cancer. The study of a highly aggressive lethal malignancy affecting the structure and function of the pancreas. It is seldom diagnosed at its early stages as it is asymptomatic till it metastasize to other organs.
-Morphology: The morphology associated with pancreatic carcinoma shows hard, stellate, gray-white, poorly defined masses.
-Histology: The histology associated with pancreatic carcinoma shows dense stromal fibrosis with poorly formed glands and the presence of inflammatory cells.
How does Pancreatic Carcinoma Present?
Patients with pancreatic carcinoma are typically common in males than females present at an age range of 60 to 80 years. The symptoms, features, and clinical findings associated with pancreatic carcinoma include noteworthy weight loss, fatigue mid-epigastric, anorexia, jaundice, and back pain.
How is Pancreatic Carcinoma Diagnosed?
Pancreatic carcinoma is diagnosed through laboratory studies, tumor makers, carbohydrate antigen 19-9. Imaging- pelvis, abdominal CT scan, transcutaneous ultrasonography, endoscopic ultrasonography, and endoscopic retrograde cholangiopancreatography.
How is Pancreatic Carcinoma Treated?
Pancreatic carcinoma is treated through surgical intervention, chemotherapy, and radiotherapy adjuvant.
What is the Prognosis of Pancreatic Carcinoma?
The prognosis of pancreatic carcinoma is poor, with a median survival rate of 4 to 6 months. less than 5% 5-year survival rate.
What is Pancreatoblastoma?
Pancreatoblastoma is a childhood tumor that is very rare of epithelial exocrine cells of the pancreas originate.
What is the Pathology of Pancreatoblastoma?
The pathology of pancreatoblastoma is: The study of fully malignant neoplasms, with a better rate than pancreatic ductal adenocarcinomas characterized squamous islands admixed with undifferentiated cells.
-Etiology: The cause of pancreatoblastoma is is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pancreatoblastoma is not well understood.
-Morphology: The morphology associated with pancreatoblastoma shows large tumors up to 18cm in diameter.
-Histology: The histology associated with pancreatoblastoma shows squamous islands admixed with undifferentiated cells.
How does Pancreatoblastoma Present?
Patients with pancreatoblastoma typically have no gender prevalence present at an age range of 1 to 15 years. The symptoms, features, and clinical findings associated with pancreatoblastoma include abdominal mass, abdominal pain, jaundice, failure to thrive, abdominal distension, and endocrine syndromes.
How is Pancreatoblastoma Diagnosed?
Pancreatoblastoma is diagnosed through laboratory studies, raised serum levels of AFP. Radiological studies-MRI, CT scan, ultrasound, reveal large well-defined, multilobulated masses.
How is Pancreatoblastoma Treated?
Pancreatoblastoma is treated through complete surgical resection, chemotherapy, and radiation therapy adjuvant.
What is the Prognosis of Pancreatoblastoma?
The prognosis of pancreatoblastoma is poor, with unresectable lesion and extensive metastasis.
What is Pancreatic Intraepithelial Neoplasia (PanIN)?
Pancreatic Intraepithelial Neoplasia (PanIN) is a well-defined precursor histologically to aggressive pancreas ductal adenocarcinoma.
What is the Pathology of Pancreatic Intraepithelial Neoplasia (PanIN)?
The pathology of pancreatic intraepithelial neoplasia (PanIN):
-Etiology: The cause of pancreatic intraepithelial neoplasia (PanIN) is idiopathically associated with gene mutations.
-Genes involved: KRAS2 gene, MAD4/DPC4, TP53, and p16/CDKN2A genes.
-Pathogenesis: The sequence of events that lead to pancreatic intraepithelial neoplasia (PanIN) is not well understood.
-Morphology: The morphology associated with pancreatic intraepithelial neoplasia (PanIN) shows they measure less than 0.5 cm,
-Histology: The histology associated with pancreatic intraepithelial neoplasia (PanIN) shows columnar epithelial cells, basally oriented uniform and round nuclei, with dysplasia.
How does Pancreatic Intraepithelial Neoplasia (PanIN) Present?
Patients with pancreatic intraepithelial neoplasia (PanIN) typically have no gender prevalence present at an age range of 50 to 80 years. The symptoms, features, and clinical findings associated with pancreatic intraepithelial neoplasia (PanIN) include noteworthy weight loss, fatigue mid-epigastric, anorexia, jaundice, and back pain.
How is Pancreatic Intraepithelial Neoplasia (PanIN) Diagnosed?
Pancreatic intraepithelial neoplasia (PanIN) is diagnosed through radiological studies and biopsy.
How is Pancreatic Intraepithelial Neoplasia (PanIN) Treated?
Pancreatic intraepithelial neoplasia (PanIN) is treated through surgical interventions, chemotherapy, and radiotherapy adjuvants.
What is the Prognosis of Pancreatic Intraepithelial Neoplasia (PanIN)?
The Prognosis of pancreatic intraepithelial neoplasia (PanIN) is poor as it is diagnosed when already it has metastasized.
What are Cystic Neoplasms of the Pancreas?
Cystic Neoplasms of the pancreas are the fluid-filled sacs within the pancreas.
Examples of Cystic Neoplasms of the pancreas include:
- Intraductal Papillary Mucinous Neoplasms (IPMNs)
- Mucinous Cystic Neoplasms
- Serous Cystic Neoplasms
- Solid-Pseudopapillary Neoplasm
What are Intraductal Papillary Mucinous Neoplasms (IPMNs)?
Intraductal papillary mucinous neoplasms (IPMNs) are cystic tumors of the pancreas that grow within the pancreatic ducts and are capable of producing mucin.
What is the Pathology of Intraductal Papillary Mucinous Neoplasms (IPMNs)?
The pathology of intraductal papillary mucinous neoplasms (IPMNs) is:
-Etiology: The cause of intraductal papillary mucinous neoplasms (IPMNs) is not clear, associated with chronic pancreatitis, diabetes, and pancreatic ductal adenocarcinoma.
-Genes involved: KRAS and GNAS gene.
-Pathogenesis: The sequence of events that lead to intraductal papillary mucinous neoplasms (IPMNs) results from the progression of benign neoplasms to invasive growths through DNA mutation. The mutated DNA loses protecting factors and experiences malignant degeneration causing unrestrained growth and convalescence.
-Morphology: The morphology associated with intraductal papillary mucinous neoplasms (IPMNs) shows duct dilatation, bulky, solid, or gelatinous nodular area.
-Histology: The histology associated with intraductal papillary mucinous neoplasms (IPMNs) shows mucin-rich columnar cells, complex papillae.
How does Intraductal Papillary Mucinous Neoplasms (IPMNs) Present?
Patients with intraductal papillary mucinous neoplasms (IPMNs) typically affect more males than females present at an age range of 5th to 7th decades. The symptoms, features, and clinical findings associated with intraductal papillary mucinous neoplasms (IPMNs) include back pain, abdominal pain, nausea/vomiting, anorexia, jaundice, and unexplained weight loss.
How is Intraductal Papillary Mucinous Neoplasms (IPMNs) Diagnosed?
Intraductal papillary mucinous neoplasms (IPMNs) are diagnosed through radiological studies-MRI, MRCP, and CT scans assess the cyst characteristics. Endoscopic ultrasound (EUS) with fine-needle aspiration (FNA) evaluates cysts with malignant features.
How is Intraductal Papillary Mucinous Neoplasms (IPMNs) Treated?
Intraductal papillary mucinous neoplasms (IPMNs) are treated through surgical oncology.
What is the Prognosis of Intraductal Papillary Mucinous Neoplasms (IPMNs)?
The prognosis of intraductal papillary mucinous neoplasms (IPMNs) is fair with a 5-year survival rate of about 45 to 50%.
What are Mucinous Cystic Neoplasms?
Mucinous cystic neoplasms are a type of cystic neoplasms that usually arise in the body or tail of the pancreas and present as painless, slow-growing masses.
What is the Pathology of Mucinous Cystic Neoplasms?
The pathology of mucinous cystic neoplasms is:
-Etiology: The cause of mucinous cystic neoplasms is unclear, though believed to be associated with female hormones.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to mucinous cystic neoplasms is not clear, believed to be related to female hormones. The incidence of estrogen receptors in these neoplasms alludes to a hormonal cause.
-Morphology: The morphology associated with mucinous cystic neoplasms are slow-growing masses that arise in the body and/or tail of the pancreas.
-Histology: The histology associated with mucinous cystic neoplasms shows it’s lined with fibrin and granulation tissue. Mucinous cystic neoplasms are filled with profuse, tenacious mucin, cysts lined with columnar mucinous epithelium, an associated dense stroma like ovarian stroma.
How does Mucinous Cystic Neoplasms Present?
Patients with mucinous cystic neoplasms typically are common in females present at an age range of 40 to 60 years. The symptoms, features, and clinical findings associated with mucinous cystic neoplasms include abdominal pain, weight loss, acute pancreatitis, and abdominal masses.
How are Mucinous Cystic Neoplasms Diagnosed?
Mucinous cystic neoplasms is diagnosed through the clinical presentation, laboratory studies-CBC count, a CA 19-9, and comprehensive metabolic panel (CMP). Radiological studies include CT scan, and MRI.
How are Mucinous Cystic Neoplasms Treated?
Mucinous cystic neoplasms is treated mainly through surgical resection splenectomy.
What is the Prognosis of Mucinous Cystic Neoplasms?
The prognosis of mucinous cystic neoplasms is fair with a 5-year survival rate of about 45 to 50%.
What are Serous Cystic Neoplasms?
Serous cystic neoplasms are benign cystic tumors having glycogen-rich, low-cuboidal cells surrounding trivial cysts comprising a clear, thin, straw-colored fluid, accounting for about 25% of pancreas cystic neoplasms.
What is the Pathology of Serous Cystic Neoplasms?
The pathology of serous cystic neoplasms is:
-Etiology: The cause of serous cystic neoplasms is not well understood.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to serous cystic neoplasms is not well understood.
-Morphology: The morphology associated with serous cystic neoplasms shows masses of varying sizes up to 20 cm, containing serous fluid.
-Histology: The histology associated with serous cystic neoplasms shows it is lined with flattened or cuboidal epithelium, dense fibronodular scar composed of acellular hyalinized tissue, and tiny cysts of cuboidal epithelial cells.
How does Serous Cystic Neoplasms Present?
Patients with serous cystic neoplasms typically common in females than males, present at an age range of 7th decade. The symptoms, features, and clinical findings associated with serous cystic neoplasms include nonspecific abdominal pain, abdominal masses.
How is Serous cystic neoplasms Diagnosed?
Serous cystic neoplasms are diagnosed through clinical presentation and radiological studies- CT scan, and MRI.
How is Serous Cystic Neoplasms Treated?
Serous cystic neoplasms is treated through surgical resection.
What is the Prognosis of Serous Cystic Neoplasms?
The prognosis of serous cystic neoplasms is fair.
What is Solid-Pseudopapillary Neoplasm?
Solid-pseudopapillary neoplasms are rare tumors of the pancreas with malignant potential characterized by large, well-circumscribed masses having solid and cystic zones.
What is the Pathology of Solid-Pseudopapillary Neoplasm?
The pathology of solid-pseudopapillary neoplasm is:
-Etiology: The cause of solid-pseudopapillary neoplasm is unclear.
-Genes involved: Beta-catenin gene on exon 3.
-Pathogenesis: The sequence of events that lead to solid-pseudopapillary neoplasm is unclear.
-Morphology: The morphology associated with solid-pseudopapillary neoplasm shows large, well-circumscribed masses partly solid and partly cyst filled with hemorrhagic debris.
-Histology: The histology associated with solid-pseudopapillary neoplasm shows cells grow in solid sheets.
How does Solid-Pseudopapillary Neoplasm Present?
Patients with solid-pseudopapillary neoplasm typically common in females present at an age range of the 3rd decade. The symptoms, features, and clinical findings associated with solid-pseudopapillary neoplasm include abdominal discomfort, abdominal mass, jaundice.
How is Solid-Pseudopapillary Neoplasm Diagnosed?
Solid-pseudopapillary neoplasm is diagnosed through clinical presentation and radiological studies- ultrasonography (US), CT scan, and magnetic resonance imaging (MRI).
How is Solid-Pseudopapillary Neoplasm Treated?
Solid-pseudopapillary neoplasm is treated through complete resection.
What is the Prognosis of Solid-Pseudopapillary Neoplasm?
The Prognosis of solid-pseudopapillary neoplasm is fair. They have malignant potential though timely resection and diagnosis offers long-term survival.
What is endocrine pancreas pathology?
Endocrine pancreas pathology is the disorder affecting the normal function of the islet cells.
Endocrine pancreas pathology includes Diabetes and pancreatic neuroendocrine tumors.
What is Diabetes?
Diabetes is a chronic ailment occurring either when the body does not effectively utilize the insulin produced or when the pancreas does not produce enough insulin.
Examples of Diabetes include:
- Diabetes Mellitus Type 1
- Diabetes Mellitus Type 2
- Monogenic Forms of Diabetes
- Pregnancy Related Diabetes
What is Diabetes Mellitus Type 1?
Diabetes Mellitus Type 1 is a metabolic disorder that is characterized by a complete deficit of insulin triggered by pancreatic β-cell destruction.
What is the Pathology of Diabetes Mellitus Type 1?
The pathology of diabetes mellitus type 1 is:
-Etiology: The cause of diabetes mellitus type 1 is autoimmune β Cell Destruction, genetic susceptibility, environmental factors.
-Genes involved: None.
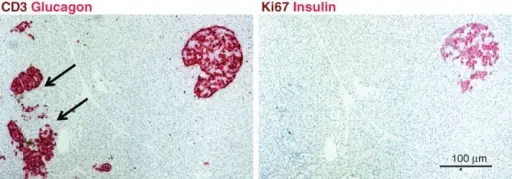
-Pathogenesis: The sequence of events that lead to diabetes mellitus type 1; the chronic autoimmune attack on β cells by T lymphocytes, autoantibodies against islet cells, and locally produced cytokines. Progressive obliteration of β cells results in clinical Diabetes. Also linked to genetic susceptibility mapped to at least 20 loci. However, the specific genes involved are not known.
-Morphology: Thin.
-Histology: None relevent.
How does Diabetes Mellitus Type 1 Present?
Patients with Diabetes mellitus type 1 typically present at an age range of 15 years. The symptoms, features, and clinical findings of Diabetes mellitus type 1 include polydipsia, polyuria, lethargy, dehydration, acidosis, and weight loss.
How is Diabetes Mellitus Type 1 Diagnosed?
Diabetes mellitus type 1 is diagnosed through clinical presentation and laboratory studies such as blood glucose elevated.
How is Diabetes Mellitus Type 1 Treated?
Diabetes mellitus type 1 is treated through insulin delivery by multiple daily injections or insulin pumps. Dietary consultation may also be needed.
What is the Prognosis of Diabetes Mellitus Type 1?
The prognosis of diabetes mellitus type 1 is fair has high morbidity and mortality and a reduced life expectancy by 10-20 years.
What is Diabetes Mellitus Type 2?
Diabetes mellitus type 2 is a metabolic disorder caused by both lack of the beta cells to allow the action of insulin to the cells and reduced secretion of insulin.
What is the Pathology of Diabetes Mellitus Type 2?
The pathology of diabetes mellitus type 2 is: a metabolic disorder characterized by the beta cells causing resistance to the action of insulin and destruction of beta cells.
-Etiology: The cause of diabetes mellitus type 2 is lifestyle factors, and obesity.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to diabetes mellitus type 2 based on the environmental and genetic factors causes the cells to be resistant to insulin leading to diabetes. In contrast, the dysfunction of the beta cells causes reduced insulin production.
-Morphology: The morphology associated with diabetes mellitus type 2 show the macrovascular disease of the arteries, microangiopathy of the small vessels, nephropathy, retinopathy, and neuropathy.
-Histology: None.
How does Diabetes Melitus Type 2 Present?
Patients with diabetes melitus type 2 are typical of both genders and present at an age range of 40 years and above but can be seen in children and adolescents. The symptoms, features, and clinical findings associated with diabetes mellitus type 2 include polyuria, polydipsia, retinopathy, blurred vision, atherosclerosis
How is Diabetes Melitus Type 2 Diagnosed?
Diabetes melitus type 2 is diagnosed by history taking and laboratory studies for any elevated levels of glucose and plasma glucose levels.
How is Diabets Meliutus Type 2 Treated?
Diabetes mellitus type 2 is treated by managing the symptoms controlling blood sugar levels, blood pressure, smoking cessation, and regular exercise to help in weight loss.
What is the Prognosis of Diabetes Melitus Type 2?
The prognosis of diabetes mellitus type 2 is fair when there is proper management of glucose levels.
What are Monogenic Forms of Diabetes?
Monogenic forms of diabetes are subtypes of diabetes that occur due to mutation of the genes involved making the loos function.
Monogenic forms of diabetes include:
- Maturity onset diabetes of the young (MODY)
- Diabetes due to insulin receptor defects
What is Maturity Onset Diabetes of the Young (MODY)?
Maturity onset diabetes of the young (MODY) is a type of diabetes that occurs mostly in young people and occurs due to a mutation in one of the six genes involved in insulin production, characterized by abnormally high levels of blood sugar.
What is the Pathology of Maturity Onset Diabetes of the Young?
The pathology of maturity-onset diabetes of the young is:
-Etiology: The cause of maturity-onset diabetes of the young is gene mutation mostly, genetic inheritance.
-Genes involved: HNF1A, GCK, HNF4A, HNF1B.
-Pathogenesis: The sequence of events that lead to maturity-onset diabetes of the young: the mutation in one of the genes responsible for the development and the function of the beta cells causes them to underdeveloped and fail in their position; hence insulin is not produced due to the altered function of the beta cells.
-Morphology: None.
-Histology: None relevent.
How does Maturity Onset Diabetes of the Young Present?
Patients with maturity-onset diabetes of the young typically affect obese children, teenagers, and adolescents present at an age range of 30 years. The symptoms, features, and clinical findings associated with maturity-onset diabetes of the young include increased blood sugar levels, polydipsia, polyuria.
How is Maturity Onset Diabetes of the Young Diagnosed?
The maturity-onset diabetes of the young is diagnosed urinalysis, lab workups, and genetic testing.
How is Maturity Onset Diabetes of the Young Treated?
The maturity-onset diabetes of the young is treated by diet modification, exercise, sulfonylureas, close management of blood sugar.
What is the Prognosis of Maturity-Onset Diabetes of the Young?
The Prognosis of maturity onset diabetes of the young is fair.
What is Diabetes due to Insulin Receptor Defects?
Diabetes due to Insulin receptor defects is an anomaly of the insulin receptors (INSR) most likely due to gene mutation leading to insulin resistance, consequently leading to diabetes.
What is the Pathology of Diabetes due to Insulin Receptor Defects?
The pathology of diabetes due to insulin receptor defects is:
-Etiology: The cause of diabetes due to insulin receptor defects is believed to be a mutation of INSR gene.
-Genes involved: INSR gene.
-Pathogenesis: The sequence of events that lead to diabetes due to insulin receptor defects not clearly understood.
-Morphology: None.
-Histology: None relevent.
How does Diabetes due to Insulin Receptor Defects Present?
Patients with diabetes due to insulin receptor defects are typically more common in males than females present at an age range of 20 to 40 years. The symptoms, features, and clinical findings associated with diabetes due to insulin receptor defects include that insulin resistance: hypertension, symptoms of coronary artery disease, obesity, microvascular angina, severe hyperinsulinemia.
How is Diabetes due to Insulin Receptor Defects Diagnosed?
Diabetes due to insulin receptor defects is diagnosed through laboratory studies which include plasma glucose level, glycohemoglobin levels, lipid profile, electrolyte levels, plasminogen activator inhibitor (PAI)-1, and urinalysis.
Diabetes due to insulin receptor defects is treated through medical therapy- metformin, thiazolidinediones diet modification.
What is the Prognosis of Diabetes due to Insulin Receptor Defects?
The prognosis of diabetes due to insulin receptor defects is fair despite modern modalities treatment, mortality and morbidity rates are still significant.
What are Pregnancy Related Diabetes?
Pregnancy related diabetes are a form of elevated blood sugar levels that occur during pregnancy.
Pregnancy related diabetes include:
- Pregestational diabetes
- Gestational diabetes
What is Pregestational Diabetes?
Pregestational diabetes is a form of blood sugar elevation disease before one becomes pregnant.
What is the Pathology of Pregestational Diabetes?
The pathology of pregestational diabetes is: a disease caused by elevated blood sugar levels before one becomes pregnant, and it can be type 1 or type 2.
-Etiology: The cause of pregestational diabetes is type 1 or type 2 diabetes
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pregestational diabetes are hormone changes that trigger diabetes.
-Morphology: None.
-Histology: None.
How does Pregestational Diabetes Present?
Patients with pregestational diabetes typically are females present at an age range of reproductive period. The symptoms, features, and clinical findings associated with pregestational diabetes include polyuria, pilydypsia and also increased levels of blood sugar.
How is Pregestational Diabetes Diagnosed?
The pregestational diabetes is diagnosed by fasting blood sugar levels, and glucose tolerance testing.
How is Pregestational Diabetes Treated?
Pregestational diabetes is treated by lifestyle modification, blood sugar monitoring, healthy diet, and regular antenatal checkup.
What is the Prognosis of Pregestational Diabetes?
The prognosis of pregestational diabetes is fair since once the child is born it goes away.
What is Gestational Diabetes?
Gestational diabetes is a disease of increased blood sugar detected during pregnancy for the first time.
What is the Pathology of Gestational Diabetes?
The pathology of gestational diabetes is:
-Etiology: The cause of gestational Diabetes is hormonal changes during pregnancy, advanced age, history of large for gestational age babies
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to gestational diabetes changes of the hormones plasma levels. Gestational diabetes is characterized by increased blood sugar, and it only occurs for the first time during pregnancy.
-Morphology: None.
-Histology: None relevent.
How does Gestational Diabetes Present?
Patients with gestational diabetes are pregnant females with new onset diabetes.
How is Gestational Diabetes Diagnosed?
Gestational diabetes is diagnosed Glucose Challenge Test, follow-up glucose testing.
How is Gestational Diabetes Treated?
Gestational diabetes is treated changes in lifestyle, sugar monitoring, healthy diet, and exercise.
What is the Prognosis of Gestaional Diabetes?
The prognosis of gestational diabetes is good.
What are Pancreatic Neuroendocrine Tumors?
Pancreatic neuroendocrine tumors are diseases of abnormal cell growth that arise from the islet cells of the pancreas.
Examples of Pancreatic Neuroendocrine Tumors include:
- Gastrinoma
- Glucagonoma
- Insulinoma
- Pancreatic Carcinoid Tumor
- Pancreatic Polypeptide-Secreting Endocrine Tumors
- Somatostatinoma
- VIPoma
What is a Gastrinoma?
A gastrinoma is a type of tumor that leads to increased production of gastric acid secretion located at the head of the pancreas.
What is the Pathology of Gastrinoma?
The pathology of gastrinoma is:
-Etiology: The cause of gastrinoma is excess gastrin secretions.
-Genes involved: None.
-Pathogenesis: Excess gastrin secretion.
-Morphology: None.
-Histology: The histology associated with gastrinoma shows bland and rare cases of anaplasia, well-differentiated lesional cells.
How does Gastrinoma Present?
Patients with gastinoma typically more in males present at an age range of 30-50 years. The symptoms, features, and clinical findings of gastrinoma include abdominal pain, diarrhea, steatorrhea, weight loss, gastroesophageal reflux.
How is Gastrinoma Diagnosed?
Gastrinoma is diagnosed by secretin stimulation test, basal acid output >10mEq/h, fasting hypergastrinemia, fasting serum gastrin levels, somatostatin receptor scintigraphy, CT scan and MRI.
How is Gatrinoma Treated?
Gastrinoma is treated by symptom management. Chemotherapy, surgical care, and frequent long-term monitoring may be required.
What is the Prognosis of Gastrinoma?
The prognosis of gastrinoma is fair, with a survival rate of 5-years being 20-30%.
What is a Glucagonoma?
Glucagonoma is a disease of the pancreas that leads to increased production of the glucagon hormone in the blood.
What is the Pathology of Glucagonoma?
The pathology of glucagonoma is:
-Etiology: The cause of glucagonoma is unclear but can be due to familial inheritance.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to glucagonoma is uncertain.
-Morphology: The morphology associated with glucagonoma shows a single solid mass with well-marked boundaries.
-Histology: The histology associated with glucagonoma shows tumor cells organized in nests and strands.
How does Glucagonoma Present?
Patients with glucagonoma, are typically males and females, at an age range of 20-84 years. The symptoms, features, and clinical findings associated with glucagonoma include diarrhea but can be asymptomatic during the early stages, weight loss, stomatitis. Glucagonoma is associated with a characteristic rash called necrolytic migratory erythema.
How is Glucagonoma Diagnosed?
Glucagonoma is diagnosed by radioimmunoassay, fasting blood sugar and glucose tolerance test, complete blood count, angiography, and CT scan.
How is Glucagonoma Treated?
Glucagonoma is treated according to the stage of the disease, debulking, surgical resection, long-acting octreotide, and embolization.
What is the Prognosis of Glucagonoma?
The prognosis of glucagonoma is poor if metastasis has occurred.
What is an Insulinoma?
Insulinoma is a neuroendocrine tumor that causes endogenous hyperinsulinism.
What is the Pathology of Insulinoma?
The pathology of insulinoma is:
-Etiology: The cause of insulinoma is endogenous hyperinsulinism.
-Genes involved: MEN 1 gene.
-Pathogenesis: The sequence of events that lead to insulinoma is not documented.
-Morphology: The morphology associated with insulinoma shows solitary well-encapsulated tumors and are alone and 0.5-10cm.
-Histology: None relevent.
How does Insulinoma Present?
Patients with insulinoma are typically more in females present at an age range of 30-60 years. The symptoms, features, and clinical findings associated with insulinoma include reduced sugar levels, diplopia, blurred vision, palpitations, weakness,
How is Insulinoma Diagnosed?
Insulinoma is diagnosed testing of serum insulin levels, glucose levels <40mg/dl, sulfonylurea negative, endoscopy, transabdominal high-resolution ultrasonography.
How is Insulinoma Treated?
Insulinoma is treated through medical care which include anti-hypoglycemics, and surgery.
What is the Prognosis of Insulinoma?
The prognosis of insulinoma is fair, but worsens if metastasis has occurred.
What is Pancreatic Carcinoid Tumor?
Pancreatic carcinoid tumor is a rare tumor of the pancreas that usually presents with carcinoid syndrome, which is characterized by diarrhea, valvular disease, cutaneous flushing.
What is the Pathology of Pancreatic Carcinoid Tumor?
The pathology of pancreatic carcinoid tumor is:
-Etiology: The cause of pancreatic carcinoid tumor is not known
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pancreatic carcinoid tumor are not known.
-Morphology: The morphology associated with pancreatic carcinoid tumor shows a polypoid mass.
-Histology: The histology associated with pancreatic carcinoid tumor shows distinctive patterns: trabecular or ribbons; solid, nodular, and insular cords; ill differentiated or atypical forms; tubules and glands or rosettelike forms; and assorted patterns.
How does Pancreatic Carcinoid Tumor Present?
Patients with pancreatic carcinoid tumor typically have no gender prevalence present at an age range of 20 years and above. The symptoms, features, and clinical findings associated with pancreatic carcinoid tumor include abdominal pain, cutaneous flushing, and pellagra skin lesions.
How is Pancreatic Carcinoid Tumor Diagnosed?
Pancreatic carcinoid tumor is diagnosed through laboratory testing which includes biomarkers and biogenic amine levels. Imaging studies plain radiography, CT scan, ultrasound, MRI, and angiography.
How is Pancreatic Carcinoid Tumor Treated?
Pancreatic carcinoid tumor is treated through chemotherapy and surgical interventions.
What is the Prognosis of Pancreatic Carcinoid Tumor?
The prognosis of pancreatic carcinoid tumors is fair.
What are Pancreatic Polypeptide-Secreting Endocrine Tumors?
Pancreatic polypeptide-secreting endocrine tumors are lesions of the pancreas that cause the secretion of the poly-peptide hormone and is also known as Ppomas.
What is the Pathology of Pancreatic Polypepetide-Secreting Endocrine Hormone?
The pathology of pancreatic polypepetide-secretine endocrine hormone is:
-Etiology: The cause of pancreatic polypepetide-secretine endocrine hormone is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pancreatic polypepetide-secreting hormone is unknown.
-Morphology: None.
-Histology: None relevent.
How does Pancreatic Polypolypepetide-Secreting Hormone Present?
Patients with pancreatic polypepetide-secreting hormone typically are females in their fortys. The symptoms, features, and clinical findings associated with pancreatic polypepetide-secreting hormone include asymptomatic at first later we see jaundice and severe abdominal pain.
How is Pancreativ Polypeptide-Secricting Hormone Diagnosed?
Pancreatic polypetide-secreting hormone is diagnosed by theserum levels of pancreatic polypeptide, physical examination, CT scan, and MRI.
How is Pancreatic Polypeptide-Secting Hormone?
Pancreatic polypeptide-secreting hormone is treated by surgical resection.
What is the Prognosis of Pncrestic Polypepetide-Secreting Hormone?
The prognosis of pancreatic polypeptide-secreting hormone is poor.
What is a Somatostatinoma?
Somatostatinoma is a rare tumor of the endocrine system that is characterized by increased production of the somatostatin hormone.
What is the Pathology of Somatostatinoma?
The pathology of somatostatinoma is the study of the disease that occurs in the pancreas or the GIT state that causes increased production of the somatostatin hormone:
-Etiology: The cause of somatostatin is multiple endocrine neoplasias.
-Genes involved: MEN 1
-Pathogenesis: The sequence of events that lead to somatostatinoma is believed to result from the inhibitory action of somatostatin.
-Morphology: None.
-Histology: None relevant.
How does Somatostatinoma Present?
Patients with somatostatinoma typically are both male and female present at age range of 20-80 years. The symptoms, features, and clinical findings associated with somatostatinoma include weigt loss, steatorrhoea, and diarrhea.
How is Somatostatinoma Diagnosed?
Somatoststinoma is diagnosed by physical examination, CT scan, MRI, somatoststin receptor scintigraphy, and angiography.
How is Somatostatinoma Treated?
Somatostatinoma is treated by insulin therapy. Surgery may be needed as well.
What is the Prognosis of Somatostatinoma?
The prognosis of somatostatinoma is good because it has a 10-year survival rate.
What is a VIPoma?
VIPoma is a neuroendocrine tumor that is characterized by in characterized by increased production of the vasoactive intestinal peptide hormone.
What is the Pathology of VIPoma?
The pathology of vipoma is:
-Etiology: The cause of VIPoma is increased production of vasoactive peptide hormone.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to vipoma is a result of VIP deficiency
-Morphology: None.
-Histology: The histology associated with VIPoma shows cells with round nuclei with low mitotic rate, and there are sheets of nests.
How does VIPoma Present?
Patients with vipoma are typically children or elderly. The symptoms, features, and clinical findings associated with vipoma include tachycardia, muscle weakness, hepatomegaly, diarrhea and, facial flushing.
How is VIPoma Diagnosed?
VIPoma is diagnosed history taking and physical examination, radioimmunoassay, CT scan, MRI, somatostatin receptors scintigraphy.
How is VIPoma Treated?
Vipoma is treated octreotide, glucocorticoids, fluids, and electrolyte replacement therapy, systemic chemotherapy, radiotherapy, surgical exploration with tumor resection.
What is the Prognosis of VIPoma?
The prognosis of vipoma is fair since it has a survival rate of more than 5 years.