The cellular response to injury depends on the specific type of injury, how severe the injury is, and how long the injury is for.
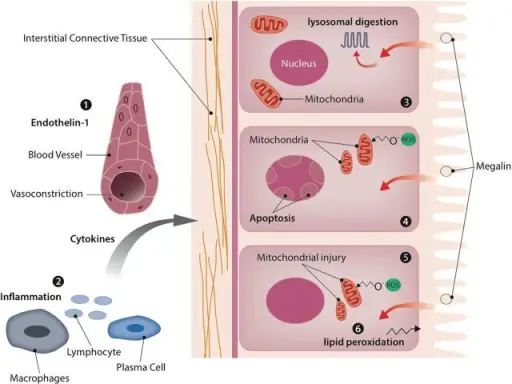
The mechanisms of cell injury may involve the following:
- Depletion of ATP
- Mitochondrial damage
- Influx of calcium and loss of calcium homeostasis
- Accumulation of oxygen-derived free radicals (oxidative stress)
- Defects in membrane permeability
- Damage to DNA and proteins
How Can Depletion of ATP Lead to Cell Injury?
Depletion of ATP may lead to cell injury or necrotic cell death via the following mechanism. It causes an end to a broad range of energy-dependent processes necessary for maintaining cellular life. Probably the most vital such process is maintaining plasma membrane, whose interruption deranges the permeability of the membrane.
How Can Mitochondrial Damage Lead to Cell Injury?
Mitochondrial damage may lead to cell injury or necrotic cell death via the following mechanism. It eliminates cellular respiration, therefore resulting in a decline in cellular ATP stores. This damage could also predispose the system to improper Cytochrome C release. It can induce apoptosis and cause cell death.
How Can Influx of Calcium Lead to Cell Injury?
Influx of calcium and loss of calcium homeostasis may lead to cell injury or necrotic cell death via the following mechanism. Loss of Ca(2+) homeostasis leads to cell injury. Based on the Ca(2+) intensity of toxicity and cell type, the following pathology can be either irreversible or reversible.
How Can Accumulation of Oxygen Derived Free Radicals Lead to Cell Injury?
Accumulation of oxygen-derived free radicals (oxidative stress) may lead to cell injury or necrotic cell death via the following mechanism. Oxidative stress induces autophagy under reperfusion/ischemia and starvation conditions. ROS created at high levels induce cell death and cellular damage. The former often incorporates the induction of apoptosis via caspase activation.
How Can Defects in Membrane Permeability Lead to Cell Injury?
Defects in membrane permeability may lead to cell injury or necrotic cell death via the following mechanism. Membrane damage can impact the plasma membrane, mitochondria, and additional cellular membranes. In ischemic cells, for example, the defects could be caused by events featuring ATP depletion and alterations in intracellular calcium via activation of phospholipases.
How Can Damage to DNA Lead to Cell Injury?
Damage to DNA and proteins may lead to cell injury or necrotic cell death via the following mechanism. Structural DNA changes drastically impact its functions. Transcription and replication play a key role in age-related illnesses and carcinoma. The repercussions of DNA damage vary based on its severity and cell type. Mild damage often prompts cell-cycle arrest. While irreparable injuries shift the cellular response, inducing cell death programs.
Examples of Cellular Injury:
Lack of oxygen may be associated with ischemic injury, hypoxic injury, and ischemic-reperfusion injury.
What is Ischemic Injury?
Ischemic injury is the result of absence or drop in circulation. Complications like severe abnormal heart rhythms are typical examples of such an injury. An ischemic state prompts anaerobic metabolism, thus curbing ATP production and affecting the ion-exchange channels. Failure of these channels causes impaired cytoplasm enzymatic activity and cell swelling.
What is Hypoxic Injury?
Hypoxic injury happens when a certain internal event won’t allow blood packed with oxygen to reach the brain, as is the case with a cardiac arrest. Simply put, the cell swells in hypoxic injury. This issue is the result of oxygen deprivation. The cell begins to swell due to the loss of volume control.
What is Ischemia Reperfusion Injury?
Ischemia-reperfusion injury is a paradoxical exacerbation of cell death, and cellular dysfunction after circulation has been restored to tissues that were previously ischemic. This injury happens in many organs, such as the gut, kidney, lung, heart, brain, and skeletal muscle. The blood flow obstruction triggers hypoxia, causing disruptions in the electron transport chain. This injury, for example, is an unavoidable consequence of a kidney transplant.
What is Chemical Injury?
Chemical (toxic) injury is caused by chemicals or various toxins (such as industrial and pharmaceutical products) that interfere with the body’s normal functioning. Take poisons, for example. They can change the speed of normal bodily functions, like decreased breathing or increased heart rate. The impact of the toxicity will vary based on the length of exposure. Acute toxicity is from short-term exposure. While chronic toxicity is the result of long-term exposure.
How Can Physical Agents Damage Cells?
Physical agents can lead to cell membrane disruption. Agents capable of causing such injuries include very hot and cold temperatures, mechanical trauma, drastic changes in atmospheric pressure, radiation, or getting electrocuted. Take radiation or heat, for example. They can induce cell damage by literally coagulating or cooking their contents. Now, pair that with a lack of nutrients, like blood sugar or oxygen, and the cells get deprived of key materials to survive. In other words, prolonged and excessive stimuli can negatively influence key cell functions.
How Can Drugs Cause Cell Injury?
Drugs can cause cell injury by deranging or directly affecting electrolyte cell homeostasis. Even O2 in high concentrations is highly toxic. Countless reactive intermediates of toxic chemicals are free-radical generators, free radicals, and electrophiles. They could deplete biological antioxidants and intracellular glutathione. They can result in cell death, DNA damage, calcium pump impairment, and membrane damage. Like a drug-induced liver injury, for instance.
How Can Nutrient Imbalances Cause Cellular Injury?
Nutrient imbalances can cause cell injury by inducing apoptosis in a range of cell types. Diets devoid of enough protein, carbs and fat, lead to serious cell injury and poor overall health. It predisposes patients to infections, which makes it harder for the system to overcome various ailments. A typical example is protein-calorie deficiencies in malnourished populations.
How Can Infections Cause Cellular Injury?
Infections can cause cell injury through the release of exotoxins. Bacteria secrete these toxins, which could rip holes inside the cells or disrupt their normal chemical processes. The two most well-known toxins are the tetanus toxin and botulinum toxin. The former leads to spastic paralysis of muscles, while the latter triggers flaccid paralysis.
How Can Immune Issues Cause Cell Injury?
Immune issues, like an autoimmune disease, feature complicated regulatory mechanisms capable of affecting the host response to cellular injury. Thus, the immune system mistakes some parts of the body as foreign. So, it ends up releasing autoantibodies to fend off the invaders, which in reality are healthy cells.
How Can Genetic Issues Cause Cell Injury?
Genetic issues may cause cell injury due to the lack of functional proteins. A genetic abnormality often results in defects as serious as congenital malformations found in patients with Down syndrome. But, they could also be as subtle as a reduced life span of red blood cells found in sickle cell anemia patients. These changes are the result of one amino acid substitution. Therefore, the cellular impact varies from person to person. Sometimes, genetic defects can result in cell injury due to the accumulation of DNA damage or misfolded proteins – both of which can cause cellular death if they can’t be repaired. Any genetic makeup variations could also affect how much a patient is predisposed to cell injury, like whether they are vulnerable to physical agents, infections, chemicals, drugs, and so on.