Hepatoblastoma is rare tumor that originates in cells in the liver. It is the most common liver tumor in early childhood.
What is the Pathology of Hepatoblastoma?
The pathology of hepatoblastoma is:
–Etiology: The cause of hepatoblastoma is genetic.
–Genes involved: Germline APC gene mutation.
–Pathogenesis: The sequence of events that lead to hepatoblastoma are loss of function mutations in APC which leads to intracellular accumulation of the protooncogene beta-catenin, which leads to germline mutation of Wnt signal transduction and pathway.
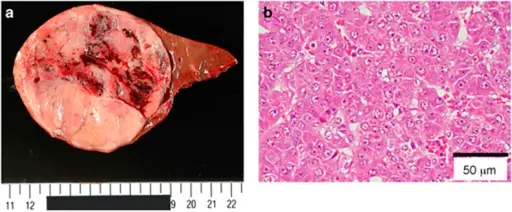
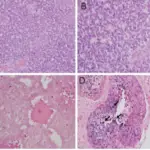
–Morphologic changes: The morphologic changes involved with hepatoblastoma are solitary, large, well circumscribed mass with heterogeneous cut surface.
How does Hepatoblastoma Present?
Patients with hepatoblastoma are typically males 1 to 5 years old. The symptoms, features, and clinical findings associated with hepatoblastoma include jaundice, swollen abdomen, weight loss, large mass in abdomen, and anemia.
How is Hepatoblastoma Diagnosed?
Hepatoblastoma is diagnosed by clinical signs, imaging findings, and elevation of serum α-fetoprotein (AFP) levels. Ultrasound, biopsy, x-rays, CT scan, MRI may be used. Biopsy is needed for definitive diagnosis.
How is Hepatoblastoma Treated?
Hepatoblastoma is treated by chemotherapy, radiotherapy, and surgery.
What is the Prognosis of Hepatoblastoma?
The prognosis of hepatoblastoma is good. Survival rates have reached 80-90 percent. This rate depends upon staging at diagnosis. Patients with fully resected tumors have a greater than 85 percent chance of survival. The rate is about 60 percent for those with metastatic disease that responds to chemotherapy.