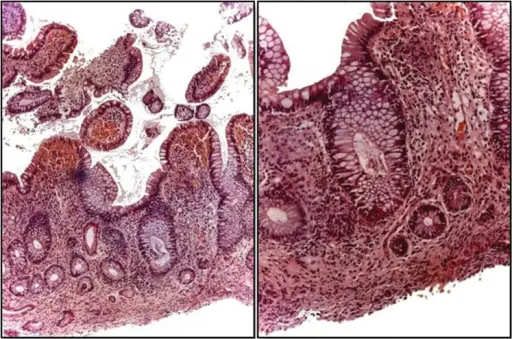
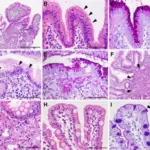
Mucosal atrophy is the loss of appropriate glands, which occurs when glands damaged by inflammation are replaced either by connective tissue scarring or by glandular structures inappropriate for location metaplasia.
What is the Pathology of Mucosal Atrophy?
The pathology of mucosal atrophy is:
-Etiology: The causes of mucosal atrophy are autoimmune due to pernicious anemia or chronic Helicobacter pylori infection.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to mucosal atrophy are low gastric acid output and hypergastrinemia, which may lead to enterochromaffin-like ECL cell hyperplasia and carcinoid tumors.
-Histology: The histology associated with mucosal atrophy shows severe mucosal damage, erosions and hemorrhage.
How does Mucosal Atrophy Present?
Patients with mucosal atrophy typically more severe in men and present at any age range. The symptoms, features, and clinical findings associated with mucosal atrophy include: stomach pain, nausea and vomiting, loss of appetite, unexpected weight loss, stomach ulcers.
How is Mucosal Atrophy Diagnosed?
Mucosal atrophy is diagnosed by endoscopy and biopsy.
How is Mucosal Atrophy Treated?
Mucosal atrophy is treated antibiotics and vitamin B12 injections.
What is the Prognosis of Mucosal Atrophy?
The prognosis of mucosal atrophy is not good. It will finally end up in a permanently acid-free stomach in the most extreme cases. Severe atrophic gastritis and acid-free stomach are the highest independent risk conditions for gastric cancer.