Inflammatory bowel disease is a term for two conditions Crohn’s disease and ulcerative colitis that are characterized by chronic inflammation of the gastrointestinal GI tract. Prolonged inflammation results in damage to the GI tract.
What is the Pathology of Inflammatory Bowel Disease?
The pathology of inflammatory bowel disease is:
-Etiology: The cause of inflammatory bowel disease is defective immune system.
-Genes involved: None.
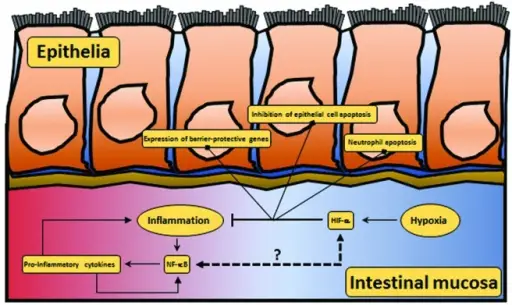
-Pathogenesis: The sequence of events that lead to inflammatory bowel disease are: the presence of pathogenic factors such as abnormal gut microbiota, immune response dysregulation, environmental changes, and gene variants. an aberrant immune response in which antibodies are formed against colonic epithelial protein.
-Histology: The histology associated with inflammatory bowel disease shows mucosal architecture, lamina propria and submucosal cellularity, neutrophil granulocyte infiltration, and epithelial abnormality.
How does Inflammatory Bowel Disease Present?
Patients with inflammatory bowel disease typically females, present at age older than 20 years. The symptoms, features, and clinical findings associated with inflammatory bowel disease include persistent diarrhea, abdominal pain, rectal bleeding/bloody stools, weight loss, and fatigue.
How Is Inflammatory Bowel Disease Diagnosed?
Inflammatory bowel disease is diagnosed by endoscopy, colonoscopy, contrast radiography, magnetic resonance imaging MRI, or computed tomography CT
How is Inflammatory Bowel Disease Treated?
Inflammatory bowel disease is treated by aminosalicylates, antibiotics, corticosteroids, and immunomodulators.
What is the Prognosis of Inflammatory Bowel Disease?
The prognosis of inflammatory bowel disease is good. Most patients with inflammatory bowel disease are able to lead a normal life and are not disabled by their disease.