Sclerosing retroperitoneal fibrosis is a relatively rare condition that is characterized by chronic inflammatory and fibrotic process in the retroperitoneum that can lead to compression of structures within the retroperitoneum.
What is the Pathology of Sclerosing Retroperitoneal Fibrosis?
The pathology of sclerosing retroperitoneal fibrosis is:
-Etiology: The cause of sclerosing retroperitoneal fibrosis is idiopathic in 70% of the cases.
-Genes involved: No genes associated.
-Pathogenesis: The sequence of events that lead to sclerosing retroperitoneal fibrosis is due to the manifestation of a systemic autoimmune disease, which may arise as a primary aortitis that elicits a periaortic fibro-inflammatory response.
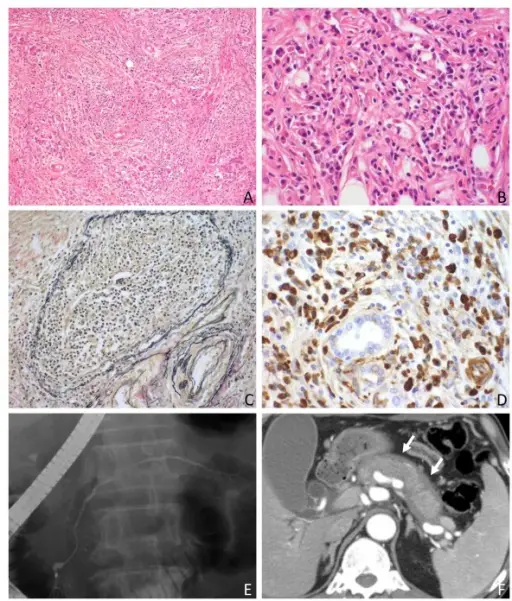
-Morphology: The morphology associated with sclerosing retroperitoneal fibrosis shows poorly circumscribed fibrotic mass.
-Histology: The histology associated with sclerosing retroperitoneal fibrosis shows the appearance of RPF of a nonspecific inflammatory process.
How does Sclerosing Retroperitoneal Fibrosis Present?
Patients with sclerosing retroperitoneal fibrosis typically affect males 2 times more than females in 40 to 60 years of age. The symptoms, features, and clinical findings associated with sclerosing retroperitoneal fibrosis include lower back and/or flank pain. This pain is often described as dull, non-colicky, unchanged with position, and with radiation into the groin or lower abdomen. Other possible associated symptoms include nausea, generalized malaise, anorexia, weight loss, oliguria, anuria. Patient’s may also describe upper-leg claudication related to arterial compromise of the lower extremities, or symptoms of mesenteric ischemia due to compression of mesenteric arteries.
How is Sclerosing Retroperitoneal Fibrosis Diagnosed?
The diagnosis of retroperitoneal fibrosis cannot be made based on the results of laboratory studies. CT is the best diagnostic modality.
How is Sclerosing Retroperitoneal Fibrosis Treated?
Patients with signs of ureteral compression with hydronephrosis and uremia require emergent decompression by either percutaneous nephrostomy tube or indwelling ureteral stents.
What is the Prognosis of Sclerosing Retroperitoneal Fibrosis?
The prognosis of sclerosing retroperitoneal fibrosis is good. Often within a few days of initiating treatment the patient’s symptoms begin to improve.