Interstitial cystitis is a condition that affects the urinary bladder, characterized by chronic inflammation. It is not secondary to an infection. It is a rare idiopathic condition of the edematous and possibly ulcerated bladder mucosa and a diagnosis of exclusion.
What is the Pathology of Interstitial Cystitis?
The pathology of interstitial cystitis is:
-Etiology: The etiology of interstitial cystitis is not well understood, and the current thoughts around its pathogenesis remain multifactorial.
-Genes involved: T13q22–q32.
-Morphology: The morphology associated with interstitial cystitis shows classic inflammatory type lesions: reddened mucosal areas with small vessels radiating towards a central scar, fibrin deposit or coagulum; site may rupture with oozing of blood and can have bullous edema.
Nonulcer type: normal-appearing urothelium or can have multiple glomerulations.
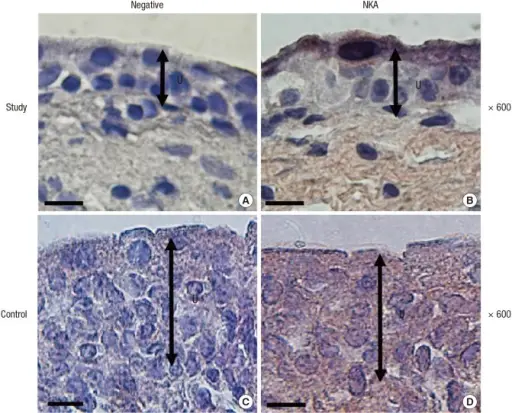
-Histology: The histology associated with interstitial cystitis shows mucosal ulceration with overlying fibrinous exudates and necrotic debris.
How does Interstitial Cystitis Present?
Patients with interstitial cystitis typically affect females between 50-60 years of age. The symptoms, features, and clinical findings associated with interstitial cystitis include suprapubic pain, urinary frequency, painful sexual intercourse, and waking up from sleep to urinate.
How is Interstitial Cystitis Diagnosed?
The diagnosis of interstitial cystitis is usually made through potassium sensitivity tests and cystoscopy.
How is Interstitial Cystitis Treated?
Interstitial cystitis is treated with antibiotics and surgical intervention.
What is the Prognosis of Interstitial Cystitis?
The prognosis of interstitial cystitis is good with appropriate treatment.