Autoimmune disorders are conditions in which the body’s immune system misidentifies and attacks its own healthy tissues as foreign. The majority of which causes inflammation, which can affect various parts of the body. Autoimmune disorders are due to autoimmunity, which is reactions against self antigens.
What is Immunologic Tolerance?
Immunologic tolerance is a complex set of mechanisms keeps that impairs the immune system’s ability to properly have an immune responses against self-antigens. It is a state of inactivity in which lymphocytes remain alive but unable to perform physiological functions.
What is Central Tolerance?
Central tolerance is when immature lymphocytes in the primary lymphoid organs encounter self-antigens, causing them to die or become unresponsive. Lymphocytes are deleted early in the development of lymphoid cells, allowing self-reactive B and T cells to be removed.
What is Peripheral Tolerance?
Peripheral tolerance is when self-reactive T cells in the periphery are deleted, suppressed, or rendered anergic.
What is the Role of Anergy in Immunologic Tolerance?
The role of anergy in immunologic tolerance is the lack of responsiveness to a self-antigen despite the presence of antigen-specific lymphocytes, causing anergic cells to persist but fail to respond to the antigenic stimulation.
What is the Role of Suppression in Immunologic Tolerance?
The role of suppression in immunologic tolerance is to reduce T cell reactivity and to maintain self-tolerance.
What is the Role of Apoptosis in Immunologic Tolerance?
The role of apoptosis in immunologic tolerance is the deletion of T cells expressing self-antigens and T-cells infected with viruses.
What Causes Autoimmunity?
Causes of autoimmunity include susceptibility genes, breakdown of self-tolerance, environmental triggers, and infections. Defective tolerance. Defective regulation. Abnormal display of self-antigens. Inflammation. Initial innate immune response.
Defective tolerance is the inability to distinguish between self and non-self antigens, which leads to autoimmune diseases.
Defective regulation is the inability to control or restrain immune responses, resulting in either underreacting or overreacting to foreign invaders.
Abnormal display of self-antigens is the failure of self-tolerance mechanisms in T or B cells, resulting in an imbalance between lymphocyte activation and control.
Inflammation is a normal physiological defense against pathogen infection and tissue damage that resolves quickly. However, as a result of dysregulation, it may persist and cause significant tissue and organ damage.
Initial innate immune response is the first line of defense against invading pathogens and relies on the body’s ability to recognize pathogens.
What are Susceptibility Genes?
Susceptibility genes or genetic predisposition is an increased likelihood of developing a particular disease based on a person’s genetic makeup.
Examples of susceptibility genes include:
- HLA genes (HLA-B27)
- Non-MHC genes
- PTPN22
- NOD2
- NLR
Genetic issues that may lead to autoimmunity:
HLA-B27, also known as human leukocyte antigen B27, is a protein found on the surface of white blood cells that aids the body’s immune system in distinguishing between its own cells and foreign substances. It is found in people who have autoimmune disorder such as arthritis.
PTPN22 polymorphisms or the protein tyrosine phosphatase non-receptor type 22, is a missense polymorphism that inhibits spontaneous T-cell activation and development, as well as inactivating T-cell receptor-associated kinases and their substrates.
NOD2 polymorphism is a substitution mutation (Arginine – Glycine), or a frameshift mutation, resulting to a diminished function of its ability to detect bacteria and trigger immune response.
IL-2 polymorphisms is a single nucleotide polymorphism that affects its regulatory function in the immune system.
CD25 mutation is due to an insertion and substitution in the gene leading to the formation of a stop codon which terminates its regulation and activity in the immune system
AIRE mutation causes autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED). This causation is due to the missense mutation of the gene that shortens it and makes it inactive compromising its role as an autoimmune regulator and a central contributor to central tolerance.
CTLA4 mutation occurs as a heterozygous nonsense mutation, gene splicing, or missense mutation that decreases the expression of CTLA4 protein which is responsible for the negative regulation of immunity.
PD1 mutation negates the suppressive effect of the gene on T-cell acivation
FAS mutation leads to the accumulation of lymphocytes after an immune response is triggered due to the interference to the initiation of apoptosis
FASL mutation in the exon site causes defect in apoptosis function resulting to autoimmune lymphoproliferative syndrome
Can Autoimmune Reactions Be Triggered By Infections?
Yes, autoimmune reactions may be triggered by infections. Such as the following:
- Systemic Lupus Erythematosus – CMV, EBV, T. gondii
- Antiphospholipid Syndrome – EBV, C. tetani, CMV
- Type 1 diabetes – CMV, Saccharomyces cerevisiae
- Rheumatoid arthritis – E.coli, K. pneumoniae, P. mirabilis, EBV, endogenous retrovirus
- Multiple Sclerosis – EBV, Actinobacter sp., P. aeruginosa
- Sjogren’s syndrome – coxsackie virus, EBV
What are the Features of Autoimmune Diseases?
The features of autoimmune conditions are fatigue, joint pain and swelling, skin problems, abdominal pain or digestive issues, recurring fever, and swollen glands. Autoimmune diseases are usually chronic issues, and are prone to remission and relapse. The damage caused by autoimmune conditions is typically progressive.
Examples of autoimmune conditions include:
- Systemic Lupus Erythematosus
- Rheumatoid Arthritis
- Sjögren Syndrome
- Systemic Sclerosis
- Inflammatory Myopathies
- Mixed Connective Tissue Disease
- Polyarteritis Nodosa and Other Vasculitides
- Necrotizing Inflammation of Blood Vessel Walls
- IgG4-Related Disease
What is Systemic Lupus Erythematosus?
Systemic lupus erythematosus (SLE) is an autoimmune disease that affects multiple organs. Autoantibodies are produced due to failure to maintain self-tolerance. Antinuclear antibodies (ANAs).
What is the Pathology of Systemic Lupus Erythematosus?
The pathology of systemic lupus erythematosus is:
-Etiology: The cause of systemic lupus erythematosus is unknown, but can be attributed to multiple genetic predispositions and gene-environmental interaction.
-Pathogenesis: The sequence of events that lead to systemic lupus erythematosus is the self-dependent antigen activation of autoreactive B cells and CD4+ T cells in secondary lymphoid organs leading to the release of autoantibodies and inflammatory cytokines that lead to tissue injury.
-Morphologic changes: The morphologic changes involved with systemic lupus erythematosus can be seen on the:
- Skin (malar rash, urticaria, bullae and ulcerations)
- Kidneys (Minimal mesangial lupus nephritis, Mesangial proliferative lupus nephritis, Focal lupus nephritis, Diffuse lupus nephritis, Membranous lupus nephritis, and Advance sclerosing lupus nephritis)
- Heart (myocarditis, valvular abnormalities, and endocarditis)
- Spleen (splenomegaly, follicular hyperplasia, onion-skin lesions)
- Lungs (chronic interstitial fibrosis)
How does Systemic Lupus Erythematosus Present?
Patients with systemic lupus erythematosus typically women of childbearing age or at a range of 14-64 years, and predominates in Blacks, Asians, and Americans. The symptoms, features, and clinical findings associated with systemic lupus erythematosus include a triad of fever, joint pains, and a characteristic butterfly malar rash.
How is Systemic Lupus Erythematosus Diagnosed?
Systemic lupus erythematosus is diagnosed through clinical findings and laboratory evidence. Standard laboratory studies include CBC, serum creatinine, and urinalysis; autoantibody tests are also performed such as ANA and anti-dsDNA.
Criteria of systemic lupus erythematous include four or more of the following:
- Malar rash
- Discoid rash
- Photosensitivity
- Oral ulcers
- Arthritis
- Serositis
- Renal disorder
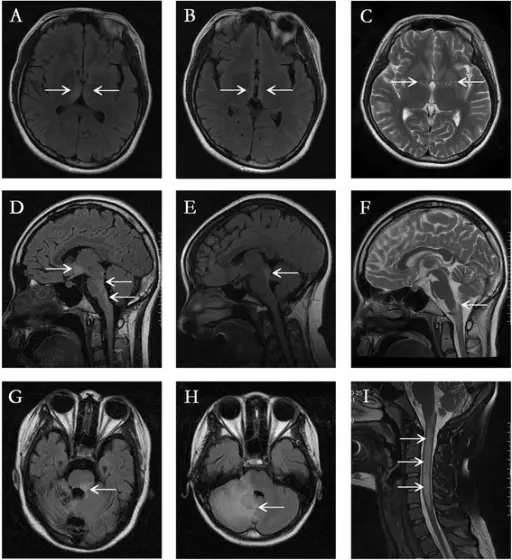
- Neurologic disorder
- Hematologic disorder
- Immunologic disorder
- Antinuclear antibody
Other laboratory tests that may be helpful in its diagnosis are presence of ESR/ CRP, complement levels, liver function tests, creatinine kinase assay, and spot protein/spot creatinine ratio. Radiologic studies are only used to monitor progression of the disease, and involvement of other organs.
How is Systemic Lupus Erythematosus Treated?
Systemic lupus erythematosus is treated mainly with hydroxychloroquine. Cutaneous manifestations are managed with NSAIDs and SLE without major organ involvement can benefit from glucocorticoids and antimalarial agents. Other immunosuppressive agents (azathioprine, mycophenolate mofetil, methotrexate) may be considered in refractory cases. DMARDS are also utilized to reduce disease activity such as belimumab, rituximab, and anifrolumab.
What is the Prognosis of Systemic Lupus Erythematosus?
The prognosis of systemic lupus erythematosus varies per individual. Systemic lupus erythematous ranges from benign to progressive to fatal manifestations of the disease. A milder disease progression and higher survival rate is associated with isolated skin and musculoskeletal disease manifestation; while patients with kidney and central nervous disease are associated with disease severity and poor survival rate.
What is Antiphospholipid Antibody Syndrome?
Antiphospholipid antibody syndrome is an acquired autoimmune disease that manifest as recurrent thrombosis or fetal loss in pregnant women. It is a condition that alters the regulation of blood coagulation.
What are the Different Types of Systemic Lupus Erythematous?
There are many types of Systemic lupus erythematous (SLE) which include:
- Diffuse lupus nephritis
- Membranous Lupus Nephritis
- Advanced Sclerosing Lupus Nephritis
- Chronic Discoid Lupus Erythematous
- Subacute Cutaneous Lupus Erythematous
- Drug-Induced Lupus Erythematosus
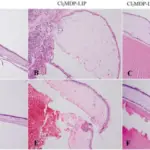
Diffuse lupus nephritis is class IV glomerulonephritis that involves more than 50% of all glomeruli with subendothelial deposits.
Membranous lupus nephritis is class V glomerulonephritis consists of global or segmental sub epithelial immune deposits that occur in combination with manifestations in class III or IV. It shows mesangial hyper cellularity and advanced sclerosis.
Advanced sclerosing lupus nephritis is class VI glomerulonephritis that involves more than 90% or the glomeruli that shows global sclerosis.
Chronic discoid lupus erythematous is the most common type of cutaneous lupus erythematosus that is characterized by scaly, disk-like plaques on the scalp, face, and ears.
Subacute cutaneous lupus erythematous is a type of cutaneous lupus erythematosus that is characterized by widespread photosensitive rash that is non-scarring.
Drug-induced lupus erythematosus is a type of lupus that is triggered by certain medications and presents features that overlap with systemic lupus erythematosus.
What is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a chronic inflammatory disease of the joints. Rheumatoid arthritis may also involve the skin, heart, blood vessels, and lungs.
What is the Pathology of Rheumatoid Arthritis?
The pathology of rheumatoid arthritis is:
-Etiology: The cause of rheumatoid arthritis is unknown, but it can be attributed to genetics, environment, immunologic and infectious factors. Its development may also be influenced by lifestyle and socioeconomic factors.
-Pathogenesis: The sequence of events that lead to rheumatoid arthritis can be triggered by an external factor that activates immune reaction that leads to articular and extra-articular manifestations.
-Morphologic changes: The morphologic changes involved with rheumatoid arthritis are edematous, thickened, and hyperplastic synovium; formation of fronds and villi on the surface, aggregation of fibrin, osteoclastic activity leading to bone erosion, and pannus formation.
How does Rheumatoid Arthritis Present?
Patients with rheumatoid arthritis are typically women 3x more affected than men; with prevalence that increases with age and peaks presentation at age range of 35-50 years old. The symptoms, features, and clinical findings associated with rheumatoid arthritis include a hallmark of persistent symmetric polyarthritis on both hands and feet. Other features felt and seen in the joints are stiffness, tenderness, swelling, deformity, pain and limitation of motion, rheumatoid nodules, and extra-articular manifestations.
How is Rheumatoid Arthritis Diagnosed?
Rheumatoid arthritis is diagnosed through a combination of clinical, laboratory, and imaging tests. For laboratory studies, the following may be requested: ESR, CRP level, CBC, rheumatoid factor assay, and ANA assay. Radiography is the imaging pf choice for rheumatic arthritis that can assess extent and progression of the disease.
How is Rheumatoid Arthritis Treated?
Rheumatoid arthritis is treated with pharmacologic and non-pharmacologic treatments. For pharmacologic, NSAIDs, DMARDs, immunosuppressant and corticosteroids may be utilized. For non-pharmacologic, exercise, diet modification, stress management, physical therapy, and surgery, may be advised.
What is the Prognosis of Rheumatoid Arthritis?
The prognosis of Rheumatoid Arthritis is dependent on how early interventions are applied. Rheumatoid arthritis that was recognized early and treated with DMARDs showed the best prognosis in achieving remission. Prognosis is also poor in patients with positive RF results. While rheumatoid arthritis that is consistently active for one year lead to joint deformity and disability.
What is Sjögren Syndrome?
Sjögren syndrome is a chronic disease associated with dry mouth (xerostomia) and dry eyes (keratoconjunctivitis sicca) due to immune destruction of salivary and lacrimal glands.
What is Sjögren Syndrome?
Sjögren syndrome an autoimmune disease that cause dysfunction in the exocrine glands.
What is the Pathology of Sjögren Syndrome?
The pathology of sjögren syndrome is:
-Etiology: The cause of sjögren syndrome is not well understood but can be linked to environmental or endogenous antigens that trigger self-acting inflammatory response.
-Pathogenesis: The sequence of events that lead to sjögren syndrome starts with an infection or any process that can trigger an immune response in susceptible individuals. This trigger leads to epithelial cell activation and leads to a prolonged inflammatory response that resembles features of systemic autoimmunity.
-Morphologic changes: The morphologic changes involved with sjögren syndrome drying of corneal epithelium, inflammation, erosion, and ulceration of the epithelium; atrophy with inflammation, fissuring and ulceration of oral mucosa, drying and crusting of the nose that may lead to ulceration.
How does Sjögren Syndrome Present?
Patients with sjögren syndrome typically affects female more than males and can affect individuals at any age but manifests more often in the fourth to fifth decade of life, with median age of 53 years old. The symptoms, features, and clinical findings associated with sjögren syndrome include dry eyes and dry mouth, parotitis, skin dryness, raynaud phenomenon. It can also affect other part of the body such as Lungs, Gastrointestinal tract, kidneys, heart, and the CNS.
How is Sjögren Syndrome Diagnosed?
Sjögren syndrome is diagnosed through laboratory findings of elevated ESR, Presence of ANA, RF, and anti-alpha-fodrin antibody; leukopenia, anemia. Eosinophilia, and hypergammaglobulinemia. Schirmer test, staining, salivary testing, and protein profiling can also be utilized.
How is Sjögren Syndrome Treated?
Sjögren syndrome is treated based on the patient’s symptoms. Creams for dryness, NSAIDs for arthralgia’s; steroids, and immunosuppressive drugs can also be used for lymphocytic lung disease.
What is the Prognosis of Sjögren Syndrome?
The prognosis of sjögren syndrome is generally good, and mostly depends on the associated disorder.
What is Systemic Sclerosis?
Systemic sclerosis, also called scleroderma, is an autoimmune condition in which certain tissues become fibrotic, especially small blood vessels and skin.
What is Systemic Sclerosis?
Systemic sclerosis is a systemic connective tissue disease that that affects the skin, joints, and internal organs.
What is the Pathology of Systemic Sclerosis?
The pathology of systemic sclerosis is:
-Etiology: The cause of systemic sclerosis is attributed to environmental exposures to silica,. Organic solvents, alipathic hydrocarbons, epoxy resin, and pesticides as well as use of appetite suppressants, substances in cosmetic procedures, and vibration injury.
-Pathogenesis: The sequence of events that lead to systemic sclerosis is the exposure to environmental factors that leads to vascular and immunologic dysfunction resulting to fibrosis and obliterative vasculopathy.
-Morphologic changes: The morphologic changes involved with systemic sclerosis are severe fibroproliferative vascular lesion of small arteries and arterioles, excessive deposition of collagen in skin and internal organs.
How does Systemic Sclerosis Present?
Patients with systemic sclerosis are typically women more than men with a 10:1 ratio. The symptoms, features, and clinical findings associated with systemic sclerosis include cutaneous pruritus, raynaud phenomenon, dysphagia and GIT symptoms, shortness of breath on exertion, joint pain, and weakness.
How is Systemic Sclerosis Diagnosed?
Systemic sclerosis is diagnosed through findings from laboratory studies such as an increases ESR, creatinine phosphokinase levels, and urea and creatinine levels. Hypergammaglobulinemia, microangiopathic hemolytic anemia and C-reactive protein may also be helpful. Imaging and lung function tests are used to assess severity and degree of involvement of other areas of the body.
How is Systemic Sclerosis Treated?
Systemic sclerosis is treated based on presentation of the disease. For Raynaud phenomenon and ulcer manifestation, calcium channel blockers, prostanoids, tadalafil, and bosentan are recommennded. For pruritus, Camphor and menthol, topical emollients, Psoralen UV-A (PUVA) treatment, and UVA-1 phototherapy may be helpful. In calcinosis, surgery is advised.
What is the Prognosis of Systemic Sclerosis?
The prognosis of systemic sclerosis is dependent on the type of sclerosis present in the patient. Diffuse systemic sclerosis, compared with limited systemic sclerosis, can lead to death if not treated promptly. The presence of pulmonary hypertension is also a significant factor in survival.
What are Inflammatory Myopathies?
Inflammatory myopathies are immune mediated inflammation and injury of skeletal muscles. There are three types:
- Polymyositis
- Dermatomyositis
- Inclusion-body myositis.
What is Polymyositis?
Polymyositis is a type of inflammatory myopathy that leads to muscle inflammation and weakness.
What is the Pathology of Polymyositis?
The pathology of polymyositis is:
-Etiology: The cause of polymyositis is a defective cellular immunity due to viral infection, malignancies, or connective-tissue disorders.
-Pathogenesis: The sequence of events that lead to polymyositis is a genetic defect that is triggered by environmental factors that leads to activation of the inflammatory cascade and overexpression of MHC 1 in the muscle fibers.
-Morphologic changes: The morphologic changes involved with polymyositis are varying sizes of muscle fibers, scattered necrotic and regenerating muscle fibers, and endomysial inflammation.
How does Polymyositis Present?
Patients with polymyositis typically are typically women. The symptoms, features, and clinical findings associated with polymyositis include insidious symmetrical and proximal muscle weakness, dysphagia, arthralgias, Patients may have difficulty in using the muscles, difficulty in holding the head up, pericarditis, rash in face, trunk or hands, and pain.
How is Polymyositis Diagnosed?
Polymyositis is diagnosed through laboratory tests such as thrombocytosis in CBC, elevated ESR, elevated muscle enzyme levels, myoglobinuria, autoantibodies, and positive rheumatoid factor.
How is Polymyositis Treated?
Polymyositis is treated empirically using corticosteroids and immunosuppressants. Other agents such as IV IG is used for short term treatment. Diet modification that is high in protein can laso help with the condition.
What is the Prognosis of Polymyositis?
The prognosis of polymyositis is good with most patients responding to treatment and only 30% experience residual weakness.
What is Dermatomyositis?
Dermatomyositis is a type of inflammatory myopathy with distinct cutaneous manifestations.
What is the Pathology of Dermatomyositis?
The pathology of dermatomyositis is:
-Etiology: The cause of dermatomyositis is associated with genetic, immunologic, infectious, and environmental causes.
-Pathogenesis: The sequence of events that lead to dermatomyositis starts with an exogenous factor triggering the inflammatory cascade, with antibodies directed against endothelial cells resulting to the membrane attack complex’d deposition on capillaries resulting to endothelial damage, capillary necrosis, ischemia, and myofibril necrosis.
-Morphologic changes: The morphologic changes involved with dermatomyositis skin findings are heliotrope rash, dilated capillary loops, Gottron papules, V sign, Shawl sign, and Mechanic’s hands.
– Histologic changes: The histologic findings associated with dermatomyositis is the perifascicular atrophy with/without perimysial and perivascualr inflammatory infiltrates, as well as tuboreticular inclusion in the intramuscular arterioles and capillaries.
How does Dermatomyositis Present?
Patients with dermatomyositis are typically women. The symptoms, features, and clinical findings associated with dermatomyositis include an initial manifestation of skin disease, that is preceded or followed by muscle disease that present as weakness and tenderness. Extramuscular manifestation include fever, arthralgia, malaise, weight loss, Raynaud phenomenon, dysphagia, gastroesophageal reflux, atrial-ventricular defects, tachyarrythmias, dilated cardiomyopathies, gastro-intestinal ulcers and infections, joint contractures, and pulmonary issues.
How is Dermatomyositis Diagnosed?
Dermatomyositis is diagnosed through laboratory testing (muscle enzyme levels) and diagnostic exams (magnetic resonance imaging, chest radiography, ultrasonography, electromyography, or computed tomography).
How is Dermatomyositis Treated?
Dermatomyositis is treated using general and specific treatments. Bed rest is advised for patients with severe muscle inflammation and rehabilitation for those with joint contractures. For muscle disease, first line treatments include corticosteroids and steroid sparing immunosuppressive drugs.
What is the Prognosis of Dermatomyositis?
The prognosis of dermatomyositis is good with most of the patients experience spontaneous remission and only 5% leading to disease progression and death.
What is Inclusion Body Myositis?
Inclusion body myositis is an inflammatory and degenerative disease that leads to painless muscle weakness.
What is the Pathology of Inclusion Body Myositis?
The pathology of Inclusion body myositis is:
-Etiology: The cause of inclusion body myositis is unknown. Viruses may be a factor the triggers the autoimmune activity of the disease.
-Pathogenesis: The sequence of events that lead to inclusion body myositis begins with an exogenous insult that triggers an autoimmune response.
-Morphologic changes: The morphologic changes involved with inclusion body myositis is endomysial inflammation, atrophic fibers, eosinophilic cytoplasmic inclusions, and multiple myofibers with rimmed vacuoles line with granules.
How does Inclusion Body Myositis Present?
Patients with inclusion body myositis typically affects males with no racial predilection and present at age range of 56-60 years old. The symptoms, features, and clinical findings associated with inclusion body myositis include insidious and slowly progressive proximal leg and distal arm weakness with a hallmark of weakness and atrophy that commonly affects knee extensors and ankle dorsiflexors as well as wrist and finger flexors.
How is Inclusion Body Myositis Diagnosed?
Inclusion body myositis is diagnosed with laboratory tests on serum CK, ANA, as well as nerve conduction studies, needle examinations, and skeletal muscle MRI.
How is Inclusion Body Myositis Treated?
Inclusion body myositis is treated with corticosteroids and exercise therapy that can only result to transient and mild improvement in the course of the disease. No known effective treatment yet.
What is the Prognosis of Inclusion Body Myositis?
The prognosis of inclusion body myositis is good with life expectancy of patients not significantly altered, however most patients are bound to wheelchair 10-15 years after diagnosis.
What is Mixed Connective Tissue Disease?
Mixed connective tissue disease is a rare autoimmune disease that manifest features of systemic lupus erythematous, scleroderma, and polymyositis.
What is Polyarteritis Nodosa?
Polyarteritis nodosa is a systemic vasculitis associated with necrotizing inflammatory lesions that affects medium and small muscular arteries at bifurcations.
What is the Pathology of Polyarteritis Nodosa?
The pathology of polyarteritis nodosa is:
-Etiology: The cause of polyarteritis nodosa is unknown but is strongly linked with hepatitis B virus.
-Pathogenesis: The sequence of events that lead to polyarteritis nodosa start with immune complex mediated inflammation that may be due to hepatitis B virus infection leading to destruction of internal and external elastic lamina that results to fibrinoid necrosis.
-Morphologic changes: The morphologic changes involved with polyarteritis nodosa is segmental transmural necrotising inflammation
How does Polyarteritis Nodosa Present?
Patients with polyarteritis nodosa are typically men with no racial predilection and present at age range 45-65 years old. The symptoms, features, and clinical findings associated with polyarteritis nodosa include constitutional symptoms such as fever, malaise, fatigue, anorexia and weight loss, myalgia and arthralgia. Transient monocular blindness is the most common CNS presentation, while encephalopathy and seizures may occur due to multiple organ failure. Skin rashs, purpura, gangrene, nodules, and Raynaud phenomenon may also be present.
How is Polyarteritis Nodosa Diagnosed?
Polyarteritis nodosa is diagnosed with physical exam and laboratory tests. Althou non-specific, lab tests can help determine systemic nature of disease such as elevated ESR, leukocytosis, hepatitis B antigen, elevated creatinine level, proteinuria, elevated liver enzymes and hyper gammaglobulinemia.
How is Polyarteritis Nodosa Treated?
Polyarteritis Nodosa is treated with corticosteroids and cyclophosphamide.
What is the Prognosis of Polyarteritis Nodosa?
The prognosis of polyarteritis nodosa with cutaneous manifestation has better prognosis than those with abdominal manifestation.
What is IgG4-Related Disease?
IgG4-related disease is a new rare syndrome that is associated with many disease processes.
What is the Pathology of IgG4-Related Disease?
The pathology of IgG4-related disease is:
-Etiology: The cause of IgG4-related disease is unknown, but may be attributed to an autoimmune and allergic disorder.
-Pathogenesis: The sequence of events that lead to IgG4-related disease starts with autoantigens that trigger the condition, with IgG4 antibodies proven to be not pathogenic themselves and are released due to immunologic response to infection.
-Morphologic changes: The morphologic changes involved with IgG4-related disease are inflammatory pseudotumors, lymphoplasmacytic infiltration, and storiform fibrosis.
How does IgG4-Related Disease Present?
IgG4-related disease typically affects male in the head and neck region and present at age range of 50-55 years old. The symptoms, features, and clinical findings associated with IgG4-related disease include swelling of involved organ, pancreatitis, lymphadenopathy, hypothyroidism, bile duct lesion, salivary and lacrimal gland involvement, allergies and plaques, papules and nodules that are pruritic and most commonly located in the face or forearm.
How is IgG4-Related Disease Diagnosed?
IgG4-related disease is diagnosed through the combination of clincial, radiology, serologic, and endoscopic examination. Definite diagnosis requires biopsy.
How is IgG4-Related Disease Treated?
IgG4-related disease is treated with systemic steroids, azathioprine, mycophenolate mofetil, and rituximab.
What is the Prognosis of IgG4-Related Disease?
The prognosis of IgG4-related disease is dependent on its manifestation, that can either result to spontaneous resolution or progress to persistent and relapsing symptoms.