Endocervical polyps are common benign proliferations composed of a fibrovascular core and endocervical glandular or metaplastic squamous epithelium.
What is the Pathology of Endocervical Polyps?
The pathology of endocervical polyps is:
-Etiology: The cause of endocervical polyps is unknown and is thought to be resulted from infections.
-Genes involved: DES.
-Pathogenesis: The sequence of events that lead to endocervical polyps are: abnormal response to increased levels of estrogen, chronic inflammation, and cogged blood vessels in cervix cause polyps.
-Morphology: The morphology associated with endocervical polyps shows flesh-colored, single finger-like growth.
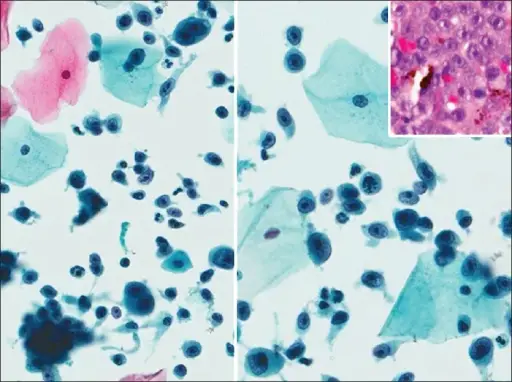
-Histology: The histology associated with endocervical polyps shows fibrovascular core, variable stromal cellularity, multinucleated stromal cells.
How does Endocervical Polyps Present?
Patients with endocervical polyps typically in females at any age but most common among patients with more than 40 years age. The symptoms, features, and clinical findings associated with endocervical polyps include: heavy menstrual periods, vaginal bleeding after intercourse, white yellow discharge.
How is Endocervical Polyps Diagnosed?
Endocervical polyps is diagnosed by: physical gynecologic examination or colposcopy, cervical pap smear test, biopsy.
How is Endocervical Polyps Treated?
Endocervical polyps is treated by excision of polyps, polypectomy, acetaminophen to treat pain.
What is the Prognosis of Endocervical Polyps?
The prognosis of endocervical polyps is good. Most cervical polyps are benign, cause no problems, and don’t come back once they’re removed.