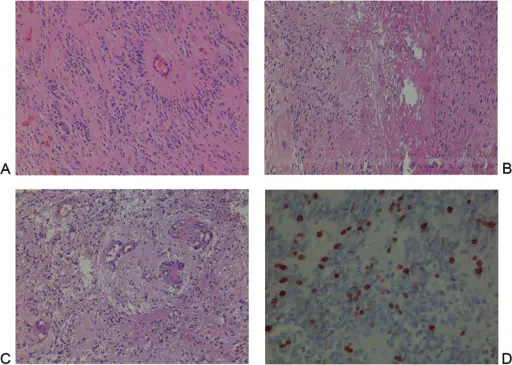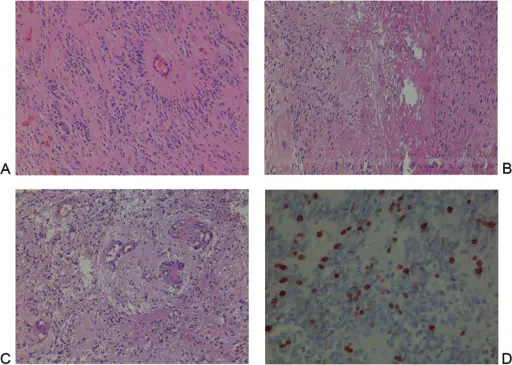
Inıtial microscopic evaluation of the case after first operation. (A) Moderately cellular tumor composed of monomorphic cells with round to oval nuclei containing “salt and pepper” pattern of chromatin. Radially arranged ependymal cell processes become thinner toward the vascular wall leaving an acellular zone around the blood vessel, called “perivascular pseudorosette,” a key histologic feature for ependymoma (hematoxylin and eosin [H&E] ×100). After the second operation (B) abundant endothelial proliferation, microvascular proliferation, hypercellularity with nuclear hyperchromasia, pleomorphism, numerous mitoses, and pseudopalisading necrosis warrants a diagnosis of anaplastic ependymoma when seen throughout the lesion (H&E ×200). Moreover (C), focus of coagulative necrosis, nuclear pseudopalisading was prominent around the necrotic areas, tumor cells oriented closer to viable areas emphasizing anaplastic changes (H&E ×200). Ki-67 immunolabeling index is an independent prognostic factor and accurate predictor of outcome in patients with intracranial ependymoma (D). The index was 10% in the first operation that increased to 35% for our case in this image (Ki-67 ×200).Malignant Transformation of Grade II Ependymoma in a 2-Year-Old Child: Case Report.
Sarıkafa Ş, Çelik SE, Yarikkaya E, Sayılgan A - Journal of neurological surgery reports (2015). Not Altered. CC.
Ependymomas are a very rare type of tumor that start in the brain or spinal cord. Ependymomas may occur in both children and adults.
What is the Pathology of Ependymomas?
Etiology: The cause of ependymomas is unknown.
Genes involved: Unknown. Increased risk with NF2.
Pathogenesis: Clonal expansion.
Histology: The histology associated with ependymomas shows well circumscribed tumors of 3 major types which include cellular (with clear cell and papillary), myxopapillary, and tanycytic.
How do Ependymomas Present?
Patients with ependymomas are typically males. Symptoms occur more commonly before 40 years of age. The symptoms, features, and clinical findings associated with Ependymomas include headaches, vomiting, dizziness, and seizures.
How is Ependymoma Diagnosed?
Ependymoma is diagnosed by neurological exam, imaging, and biopsy.
How is Ependymoma Treated?
Ependymomas are treated with surgical resection. Radiosurgery or chemotherapy may also be considered.
What is the Prognosis of Ependymomas?
The prognosis of ependymoma is fair.