Esophageal varices are enlarged veins in the esophagus.
What is the Pathology of Esophageal Varices?
The pathology of esophageal varices is:
-Etiology: The cause of esophageal varices is related to severe liver scarring cirrhosis, blood clot thrombosis, or parasitic infections.
-Genes involved: SST.
-Pathogenesis: The sequence of events that lead to esophageal varices are: increases portal pressures such as with cirrhosis, there is dilation of veins in the anastomosis, leading to esophageal varices. Splenic vein thrombosis is a rare condition that causes esophageal varices without a raised portal pressure.
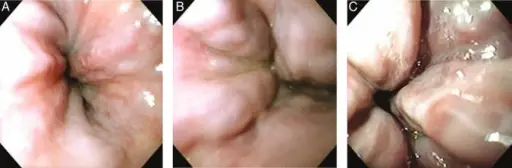
-Histology: The histology associated with esophageal varices shows expansion of the submucosa leads to elevation of the mucosa above the surrounding tissue, which is apparent during endoscopy and is a key diagnostic feature. Evidence of recent variceal hemorrhage includes necrosis and ulceration of the mucosa.
How does Esophageal Varices Present?
Patients with esophageal varices typically more in males and present at age range of 48-years-old. The symptoms, features, and clinical findings associated with esophageal varices include vomiting large amounts of blood, black, tarry or bloody stools, lightheadedness, and loss of consciousness in severe cases.
How are Esophageal Varices Diagnosed?
Esophageal varices are diagnosed by endoscopic exam, imaging tests, or capsule endoscopy.
How are Esophageal Varices Treated?
Esophageal varices is are treated by using elastic bands to tie off bleeding veins, medications to slow blood flow into the portal vein, diverting blood flow away from the portal vein, or placing pressure on varices to stop bleeding.
What is the Prognosis of Esophageal Varices?
The prognosis of esophageal varices is poor. Bleeding esophageal varices is life-threatening condition and can be fatal in up to 50% of patients. People who have had an episode of bleeding esophageal varices are at risk for bleeding again.