Hemodynamic disorders are disorders pertaining to the altered dynamics of blood flow.
Hemodynamic disorders may be due to:
- Increased hydrostatic pressure
- Reduced plasma osmotic pressure
- Sodium and water retention
- Lymphatic obstruction
What are Examples of Hemodynamic Disorders?
Examples of hemodynamic disorders include:
- Edema
- Effusions
- Hyperemia
- Congestion
- Hemorrhagic disorders
- Thrombosis
- Disseminated intravascular coagulation
- Embolism
- Infarction
- Shock
What is Edema?
Edema is the abnormal accumulation of fluid in certain tissues within the body.
What is the Pathology of Edema?
The pathology of edema is:
-Etiology: The cause of edema is an imbalance of hydrostatic or oncotic forces.
-Pathogenesis: The sequence of events that lead to edema is the increased movement of fluid from the intravascular to the interstitial space or decreased movement of water from the interstitium into the capillaries or lymphatic vessels.
-Morphology: The morphology associated with edema shows increased fluid attenuation, hydrothorax, hydropericardium, and ascites.
How does Edema Present?
Patients with edema typically are either male or female present in the age range of older adults. The symptoms, features, and clinical findings associated with edema include swelling of the affected area.
How is Edema Diagnosed?
Edema is typically diagnosed by physical exam. Additional tests, such as chest X-ray, abdominal ultrasound, ultrasound of the legs, blood tests of liver function, urinalysis, and evaluation of the patient’s kidney and liver function may be considered.
How is Edema Treated?
Edema is typically treated with fluid management, diuretics, and dietary changes.
What is the Prognosis of Edema?
The prognosis of edema is good in most cases. Patients with congestive heart failure, or liver issues may have worse prognosis.
What are Effusions?
Effusions are abnormal collections of fluid in body cavities.
What is the Pathology of Effusions?
The pathology of effusions is:
-Etiology: The cause of effusions include increased hydrostatic pressure, increased vascular permeability, decreased oncotic pressure, increased intrapleural negative pressure, decreased lymphatic drainage, trauma, or infection.
-Pathogenesis: Mismatch of fluid forces.
-Morphology: The morphology associated with effusions shows fluid accumulation that may appear clear, straw-colored, or milky white.
-Histology: The histology associated with effusions shows either serous, serofibrinous, or fibrinous and turbid serous fluid with histiocytes, with or without inflammatory cell infiltrates.
How do Effusions Present?
Patients with effusions typically are either male or female present at the age range of between 15 years of age or older. The symptoms, features, and clinical findings associated with effusions include chest pain, dry, nonproductive cough, and shortness of breath. Two main types of pleural effusions include transudative and exudative which is based on Light’s criteria.
How are Effusions Diagnosed?
Effusions are diagnosed with tests that include chest x-ray, computed tomography (CT) scan of the chest, ultrasound of the chest, thoracentesis, and pleural fluid analysis.
How are Effusions Treated?
Effusions are typically treated with diuretics and medical management of the underlying condition. Heart failure medications used for effusion caused by congestive heart failure or other medical causes. Malignant effusions may need chemotherapy, radiation therapy, or chemotherapy.
What is the Prognosis of Effusions?
The prognosis of effusions is fair.
What is Hyperemia?
Hyperemia is an excess of blood in vessels supplying a particular organ or limb.
What is the Pathology of Hyperemia?
The pathology of hyperemia is:
-Etiology: The cause of hyperemia varies greatly, from exercise, inflammation, to organ failure.
-Pathogenesis: The sequence of events that lead to hyperemia is the excess blood that builds up inside the vascular system.
-Morphology: The morphology associated with hyperemia shows active dilation of vasculature.
How does Hyperemia Present?
Patients with hyperemia typically are older males or females. The symptoms, features, and clinical findings associated with hyperemia include bright red in color, warmth, and swelling.
How is Hyperemia Diagnosed?
Hyperemia is diagnosed with a physical exam and a test for reactive hyperemia that helps measure blood flow.
How is Hyperemia Treated?
Hyperemia is treated with medications for hyperemia which may include beta-blockers, blood thinners, and digoxin.
What is the Prognosis of Hyperemia?
The prognosis of hyperemia is fair.
What is Congestion?
Congestion is a general term that refers to a feeling of stuffiness in the nasal or breathing passageways.
What is the Pathology of Congestion?
The pathology of congestion is:
-Etiology: The cause of congestion is typically increased blood volume to the vessels that line the passages inside the nose in response to allergies, or infections.
-Pathogenesis: The sequence of events that lead to congestion is the physical obstruction of nasal passages, or mucosal inflammation.
How does Congestion Present?
Patients with congestion typically are either males or females present in the age range of all age groups. The symptoms, features, and clinical findings associated with congestion include a feeling of fullness in the face, headache, and dull hearing.
How is Congestion Diagnosed?
Congestion is diagnosed based on the symptoms and a physical exam.
How is Congestion Treated?
Congestion is treated with decongestants such as pseudoephedrine or antihistamines.
What is the Prognosis of Congestion?
The prognosis of congestion is good.
What are Hemorrhagic Disorders?
Hemorrhagic disorders are a group of disorders that share the inability to form a proper blood clot.
Hemorrhagic disorders include:
- Primary hemostasis defects: platelet dysfunction, von Willebrand disease.
- Secondary hemostasis defects: coagulation factor defects.
- Small vessel defects: ecchymoses, hematoma, amyloidosis, scurvy.
What are Platelet Dysfunctions?
Platelet dysfunctions are a group of bleeding disorders in which the platelets do not function appropriately, leading to bleeding.
What is the Pathology of Platelet Dysfunctions?
The pathology of platelet dysfunctions is:
-Etiology: The cause of platelet dysfunctions is a problem in the platelets themselves or to an external factor that alters the function of normal platelets.
-Pathogenesis: The sequence of events that lead to platelet dysfunctions depends on the underlying issue which may include defects to the platelets, defects to platelet receptors, or medication related alterations of platelet activity.
-Morphology: The morphology associated with platelet dysfunctions depends on the underlying cause which may show giant platelets, structural anomalies of platelets, megakaryocyte abnormalities, or alterations of the granules within platelets.
How do Platelet Dysfunctions Present?
Patients with platelet dysfunctions typically are either males or females present in the age range of 6-80 years old. The symptoms, features, and clinical findings associated with platelet dysfunctions typically include increased bruising, nosebleeds, gum bleeding, and prolonged bleeding times.
How are Platelet Dysfunctions Diagnosed?
Platelet dysfunctions are diagnosed using special tests that include:
- Bleeding time
- Platelet function assay
- Platelet aggregation testing
- Platelet electron microscopy
- Genetic testing
How are Platelet Dysfunctions Treated?
Platelet dysfunctions are treated based on the underlying cause.
What is the Prognosis of Platelet Dysfunctions?
The prognosis of platelet dysfunctions is good if properly managed.
What is Von Willebrand Disease?
Von Willebrand disease is a blood disorder associated with excessive bleeding.
What is the Pathology of the Von Willebrand Disease?
The pathology of von Willebrand disease is:
-Etiology: The cause of von Willebrand disease is an inherited defect.
-Genes involved: vWF gene.
-Pathogenesis: The sequence of events that lead to von Willebrand disease is an abnormality, either quantitative or qualitative, of the von Willebrand factor that does not properly help stop bleeding.
-Morphology: The morphology associated with von Willebrand disease is associated with bruising and easy bleeding.
How does Von Willebrand Disease Present?
Patients with Von Willebrand disease typically are either males or females present in the age range of all age groups. The symptoms, features, and clinical findings associated with Von Willebrand disease typically include frequent bleeding, easy bruising, and pink urine.
How is Von Willebrand Disease Diagnosed?
Von Willebrand disease is diagnosed with blood and genetic tests.
How is Von Willebrand Disease Treated?
Von Willebrand disease is typically treated with desmopressin acetate.
What is the Prognosis of the Von Willebrand Disease?
The prognosis of von Willebrand disease is fair.
What are Coagulation Factor Defects?
Coagulation factor defects are abnormalities in coagulation factors that may alter the clotting process.
What is the Pathology of Coagulation Factor Defects?
The pathology of coagulation factor defects is:
-Etiology: The cause of coagulation factor defects is typically an inherited defect in the factor’s gene.
-Pathogenesis: The sequence of events that lead to coagulation factor defects are related to the specific factor that is defective.
-Morphology: The morphology associated with coagulation factor defects shows heavy and prolonged bleeding after an injury, bruising, and epistasis.
How do Coagulation Factor Defects Present?
Patients with coagulation factor defects typically are either male or female present at the age range of infants. The symptoms, features, and clinical findings associated with coagulation factor defects include bruising, and easy bleeding.
How are Coagulation Factor Defects Diagnosed?
Coagulation factor defects are diagnosed with specialized tests, and possibly genetic tests.
How are Coagulation Factor Defects Treated?
Coagulation factor defects are typically treated by replacing the defective factor with functional factors.
What is the Prognosis of Coagulation Factor Defects?
The prognosis of coagulation factor defects is good.
What is Ecchymosis?
Ecchymoses are purple flat patches on the skin that are commonly known as bruises.
What is the Pathology of Ecchymoses?
The pathology of ecchymoses is:
-Etiology: The cause of ecchymoses is typically trauma.
-Pathogenesis: The sequence of events that lead to ecchymoses is a bursting of small blood vessels that allow blood to leak under the skin.
-Morphology: The morphology associated with ecchymoses shows non-blanching, purpuric flat lesions.
How do Ecchymoses Present?
Patients with ecchymoses typically are females present in the age range of older years. The symptoms, features, and clinical findings associated with ecchymoses include an area of skin discoloration larger than 1 centimeter.
How are Ecchymoses Diagnosed?
Ecchymoses are diagnosed with a physical exam.
How are Ecchymoses Treated?
Ecchymoses are treated with symptomatic management.
What is the Prognosis of Ecchymoses?
The prognosis of ecchymoses is good.
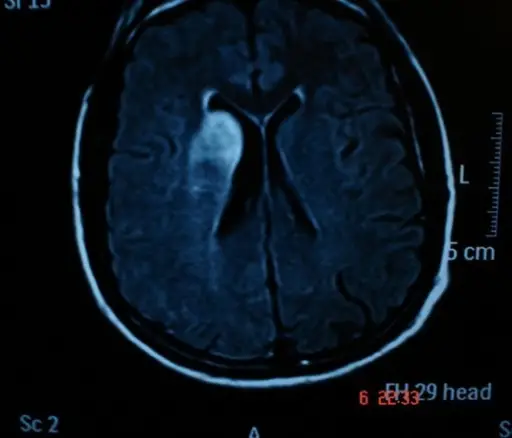
What is a Hematoma?
A hematoma is a collection of blood outside of blood vessels.
What is the Pathology of Hematoma?
The pathology of hematoma is:
-Etiology: The cause of hematoma is typically trauma.
-Pathogenesis: The sequence of events that lead to hematoma is an injury to the wall of a blood vessel.
-Morphology: The morphology associated with hematoma shows a collection of extravasated blood that may clot.
How does Hematoma Present?
Patients with hematoma typically are males present in the age range of older years. The symptoms, features, and clinical findings associated with hematoma include bruises, swelling, and redness.
- Subdural hematoma symptoms: Headache, neurologic symptoms, confusion, seizure, slurred speech.
- Epidural hematoma symptoms: Back pain, weakness, and loss of bowel or bladder control.
- Subungual hematoma symptoms: Nail pain.
- Splenic, hepatic, or peritoneal hematoma: Abdominal pain.
How is Hematoma Diagnosed?
Hematoma is diagnosed with a physical inspection along with a comprehensive medical history. Imaging may also be required.
How is Hematoma Treated?
Hematoma treatment is based on the type of hematoma that is present.
What is the Prognosis of Hematoma?
The prognosis of hematoma is based on the type of hematoma that is present.
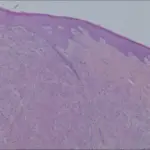
What is Amyloidosis?
Amyloidosis is a rare disease that occurs when amyloid protein deposits on certain organs which may alter the organs normal function.
What is the Pathology of Amyloidosis?
The pathology of amyloidosis is:
-Etiology: The cause of amyloidosis is the deposition of amyloid protein.
-Pathogenesis: The sequence of events that lead to amyloidosis is the abnormal accumulation of amyloid protein.
-Morphology: The morphology associated with amyloidosis shows amyloid fibrils.
-Histology: The histology of amyloidosis shows pink amorphous globules that have apple green birefringence under polarized light.
How does Amyloidosis Present?
Patients with amyloidosis typically are males present in the age range of between 60 and 70 years. The symptoms, features, and clinical findings associated with amyloidosis depend on the organ involved which typically are the kidneys, heart, or brain.
How is Amyloidosis Diagnosed?
Amyloidosis is diagnosed with biopsy.
How is Amyloidosis Treated?
Amyloidosis is treated with symptomatic management or medical management.
What is the Prognosis of Amyloidosis?
The prognosis of amyloidosis is dependent on the organ that is involved.
What is Scurvy?
Scurvy is a disease caused by vitamin C deficiency.
What is the Pathology of Scurvy?
The pathology of scurvy is:
-Etiology: The cause of scurvy is vitamin C deficiency.
-Pathogenesis: The sequence of events that lead to scurvy is a vitamin C intake below 10 mg per day.
How does Scurvy Present?
Patients with scurvy typically are males that do not eat fruits. The symptoms, features, and clinical findings associated with scurvy include easy mucosal bleeding, easy bruising, skin changes, weakness, and fatigue.
How is Scurvy Diagnosed?
Scurvy is diagnosed by history and physical exam by a healthcare professional. A blood test may be needed to measure vitamin C levels.
How is Scurvy Treated?
Scurvy is treated by increasing vitamin C consumption.
What is the Prognosis of Scurvy?
The prognosis of scurvy is good.
What is Thrombosis?
Thrombosis is a blood clot within a vessel.
There are two main types of thrombosis:
- Venous thrombosis: Blood clot blocks a vein.
- Arterial thrombosis: Blood clot blocks an artery.
What is Disseminated Intravascular Coagulation?
Disseminated intravascular coagulation is a blood clotting issue that can result in uncontrollable bleeding.
What is Embolism?
An embolism is a blocked artery caused by a foreign body. The foreign bodies include a blood clot, fat, marrow, or air bubbles.
What is Infarction?
An infarction is a well demarcated tissue lesion due to a blocked vessel.
What is Shock?
Shock is a critical condition brought on by the sudden drop in blood flow or blood pressure.
What is Hemostasis?
Hemostasis is the normal response to vascular injury that leads to clot formation and stabilization.
Hemostasis involves:
- Arteriolar vasoconstriction
- Primary hemostasis
- Secondary hemostasis
- Clot stabilization
Key components of hemostasis include the endothelium, platelets, and the coagulation cascade.
What is Arteriolar Vasoconstriction?
Arteriolar vasoconstriction is the narrowing of the blood vessels resulting from the contraction of the muscular wall of the vessels.
What is Primary hemostasis?
Primary hemostasis is a pro coagulation clot-forming process associated with the initiation and formation of the platelet plug.
What is Secondary hemostasis?
Secondary hemostasis is also a pro-coagulation clot-forming process and it’s associated with the propagation of the clotting process via the intrinsic and extrinsic coagulation cascades.
What is the Coagulation Cascade?
The coagulation cascade is the series of steps that occur during the formation of a blood clot after injury by activating a cascade of proteins called clotting factors.
The factors involved in the coagulation cascade include:
- Factor XIII
- Factor XII
- Factor XI
- Factor X
- Factor IX
- Factor VIII
- Factor VII
- Factor VI
- Factor V
- Factor IV
- Factor III
- Factor II
- Factor I
| NAME | FUNCTION | |
| Factor XIII | Fibrin-stabilizing factor | Crosslinks Fibrin |
| Factor XII | Hageman factor | Activates Factor XI, VII and Prekallikrein |
| Factor XI | Plasma thromboplastin antecedent | Activates Factor IX |
| Factor X | Stuart-Prower factor | Activates Factor II, forms prothrombinase complex with Factor V |
| Factor IX | Plasma thromboplastin component, Christmas factor | Activates Factor X, forms tenase complex with Factor VIII |
| Factor VIII | Antihemophilic factor | Cofactor of IX with which it forms tenase complex |
| Factor VII | Stable factor or proconvertin | Activates Factor IX, X |
| Factor VI | Unassigned | Unassigned |
| Factor V | Labile factor or proaccelerin | Cofactor of X with which it forms prothrombinase complex |
| Factor IV | Ionized calcium (Ca++) | Required for coagulation factors to bind to phospholipid (formerly known as factor IV) |
| Factor III | Tissue thromboplastin (tissue factor) | Cofactor of VIIa (formerly known as Factor III) |
| Factor II | Prothrombin | Factor IIa activates I, X, VII, VIII, XI, XIII, protein C, platelets |
| Factor I | Fibrinogen | Blood clot formation (Fibrin) |
What are Vitamin K Dependent Factors?
Vitamin K dependent factors include:
Factors, 2, 7, 9, 10, protein C and protein S.
What is Warfarin?
Warfarin is an anticoagulant that works by decreasing the clotting ability of blood.
What is Warfarin Toxicity?
Warfarin toxicity is when warfarin levels are excessively high.
What is the Pathology of Warfarin Toxicity?
The pathology of warfarin toxicity is:
-Etiology: The cause of warfarin toxicity is too much warfarin.
-Pathogenesis: The sequence of events that lead to warfarin toxicity is excessive warfarin.
How does Warfarin Toxicity Present?
Patients with warfarin toxicity typically are either males or females present in the age range of all age groups. The symptoms, features, and clinical findings associated with warfarin toxicity may include bleeding.
How is Warfarin Toxicity Diagnosed?
Warfarin toxicity is diagnosed with a thorough physical examination, medical review, and blood tests such as INR, PT, and BT.
How is Warfarin Toxicity Treated?
Warfarin toxicity is treated with vitamin K, fresh frozen plasma, or protamine sulfate depending on the clinical implications and the urgency needed to reverse warfarin toxicity.
What is the Prognosis of Warfarin Toxicity?
The prognosis of warfarin toxicity is fair when properly treated.
What is Heparin Induced Thrombocytopenia?
Heparin induced thrombocytopenia is a hypercoagulable syndrome.
What is the Pathology of Heparin Induced Thrombocytopenia?
The pathology of heparin induced thrombocytopenia is:
-Etiology: The cause of heparin-induced thrombocytopenia is heparin-triggered immune response.
-Pathogenesis: The sequence of events that lead to heparin induced thrombocytopenia is heparin dependent IgG antibodies bind to heparin/platelet factor 4 complexes to activate platelets and produce a hypercoagulable state.
How does Heparin Induced Thrombocytopenia Present?
Patients with heparin induced thrombocytopenia typically are females present at the age range of more than 40 years. The symptoms, features, and clinical findings associated with heparin-induced thrombocytopenia include swelling, tenderness, and anxiety.
How is Heparin Induced Thrombocytopenia Diagnosed?
Heparin Induced thrombocytopenia is diagnosed with the lab tests.
How is Heparin Induced Thrombocytopenia Treated?
Heparin Induced thrombocytopenia is treated by not using heparin.
What is the Prognosis of Heparin Induced Thrombocytopenia?
The prognosis of heparin-induced thrombocytopenia is fair.
What is Clot Stabilization?
Clot stabilization is the enhancing activation of procoagulants only at the site where a clot is desired by the coated platelets.
What are Bleeding Disorders?
Bleeding disorders are a group of conditions in which there is a problem with the body’s blood clotting process.
Examples of bleeding disorders include:
- Henoch-Schönlein purpura
- Bernard-Soulier syndrome
- Glanzmann thrombasthenia
- Von Willebrand disease
- Hemophilia A
- Hemophilia B aka Christmas disease
What is Henoch-Schönlein Purpura?
Henoch-Schönlein purpura is a disorder that causes the small blood vessels in the skin, joints, intestines, and kidneys to become inflamed and bleed.
What is the Pathology of Henoch-Schönlein Purpura?
The pathology of Henoch-Schönlein purpura is:
-Etiology: The cause of Henoch-Schönlein purpura is typically an infection.
-Pathogenesis: The sequence of events that lead to Henoch-Schönlein purpura is the body’s small blood vessels that become inflamed, which can cause bleeding in the skin, abdomen, and kidneys.
-Histology: The histology associated with Henoch-Schönlein purpura shows IgA-antibody immune complexes deposition in the small vessels.
How does Henoch-Schönlein Purpura Present?
Patients with Henoch-Schönlein purpura typically are males present in the age range of all age groups. The symptoms, features, and clinical findings associated with Henoch-Schönlein purpura include a purplish rash that is typically on the lower legs or buttocks.
How is Henoch-Schönlein Purpura Diagnosed?
Henoch-Schönlein purpura is diagnosed with lab tests, such as blood and urine tests. A biopsy may also be performed.
How is Henoch-Schönlein Purpura Treated?
Henoch-Schönlein purpura is treated with corticosteroids, such as prednisone.
What is the Prognosis of Henoch-Schönlein Purpura?
The prognosis of Henoch-Schönlein purpura is good.
What is Bernard-Soulier Syndrome?
Bernard-Soulier syndrome is a bleeding disorder associated with abnormal platelets.
What is the Pathology of Bernard-Soulier Syndrome?
The pathology of Bernard-Soulier syndrome is:
-Etiology: The cause of Bernard-Soulier syndrome is the genetic mutations in one of the Gp1b complex genes.
-Genes involved: GP1BA, GP1BB, or GP9.
-Pathogenesis: The sequence of events that lead to Bernard-Soulier syndrome is the proteins produced from GP1BA, and GP1BB.
-Morphology: The morphology associated with Bernard-Soulier syndrome shows thrombocytopenia, giant platelets, and qualitative platelet defects resulting in bleeding tendency.
How does Bernard-Soulier Syndrome Present?
Patients with Bernard-Soulier syndrome typically are either male or female present at the age range of infants. The symptoms, features, and clinical findings associated with Bernard-Soulier syndrome include easy bruising and nosebleeds.
How is Bernard-Soulier Syndrome Diagnosed?
Bernard-Soulier syndrome is diagnosed with blood and platelets tests.
How is Bernard-Soulier Syndrome Treated?
Bernard-Soulier syndrome is treated with platelet transfusion as needed.
What is the Prognosis of Bernard-Soulier Syndrome?
The prognosis of Bernard-Soulier syndrome is fair.
What is Glanzmann Thrombasthenia?
Glanzmann thrombasthenia is a bleeding disorder.
What is the Pathology of Glanzmann Thrombasthenia?
The pathology of Glanzmann thrombasthenia is:
-Etiology: The cause of Glanzmann thrombasthenia is the lack of a protein that is normally on the surface of platelets and is needed for platelets to clump together to form blood clots.
-Genes involved: ITGA2B and ITGB3.
-Pathogenesis: The sequence of events that lead to Glanzmann thrombasthenia is the platelet integrin GPIIb/IIIa abnormality that results in platelets not aggregating when they need to.
How does Glanzmann Thrombasthenia Present?
Patients with Glanzmann thrombasthenia typically are males or females present at the age range of infants. The symptoms, features, and clinical findings associated with Glanzmann thrombasthenia include easy bleeding, and nose bleeds.
How is Glanzmann Thrombasthenia Diagnosed?
Glanzmann thrombasthenia is diagnosed with platelet function analysis (PFA), prothrombin time (PT), and partial thromboplastin time (PTT).
How is Glanzmann Thrombasthenia Treated?
Glanzmann Thrombasthenia is treated with platelet transfusions as needed.
What is the Prognosis of Glanzmann Thrombasthenia?
The prognosis of Glanzmann thrombasthenia is fair.
What is Von Willebrand Disease?
Von Willebrand disease is a blood disorder in which the blood does not clot properly.
What is the Pathology of the Von Willebrand Disease?
The pathology of von Willebrand disease is:
-Etiology: The cause of von Willebrand disease is an inherited abnormal gene that controls the von Willebrand factor.
-Genes involved: vWF gene.
-Pathogenesis: The sequence of events that lead to von Willebrand disease is a hereditary defect in vWF.
How does Von Willebrand Disease Present?
Patients with von Willebrand disease typically are either male or female present at the age range of infants. The symptoms, features, and clinical findings associated with von Willebrand disease include excessive bleeding.
How is Von Willebrand Disease Diagnosed?
Von Willebrand disease is diagnosed with a medical history, physical exam, platelet testing, and genetic testing.
How is Von Willebrand Disease Treated?
Von Willebrand disease is treated with desmopressin.
What is the Prognosis of the Von Willebrand Disease?
The prognosis of von Willebrand disease is fair.
What is Hemophilia A?
Hemophilia A is an X-linked, recessive bleeding disorder.
What is the Pathology of Hemophilia A?
The pathology of hemophilia A is:
-Etiology: The cause of hemophilia A is an inherited or acquired genetic mutation that results in deficiency or dysfunction of factor VIII.
-Genes involved: X linked FVIII.
-Pathogenesis: The sequence of events that lead to hemophilia A is abnormal or absence of factor VIII clotting factor.
How does Hemophilia A Present?
Patients with hemophilia A typically are males that present with excessive bleeding at a young age. Other symptoms, features, and clinical findings associated with hemophilia A include easy bruising, hemarthrosis, and epistasis.
How is Hemophilia A Diagnosed?
Hemophilia A is diagnosed with medical history, and clotting factor tests.
How is Hemophilia A Treated?
Hemophilia A is treated with factor replacement as needed.
What is the Prognosis of Hemophilia A?
The prognosis of hemophilia A is fair.
What is Hemophilia B?
Hemophilia B aka Christmas disease is a genetic disorder caused by defective or absent factor IX.
What is the Pathology of Hemophilia B?
The pathology of hemophilia B aka Christmas disease is:
-Etiology: The cause of hemophilia B aka Christmas disease is an inherited or acquired mutation in the factor IX gene, or acquired factor IX inhibitor.
-Genes involved: Factor IX gene.
-Pathogenesis: The sequence of events that lead to hemophilia B aka Christmas disease is factor IX deficiency or dysfunctional factor IX that results in prolonged bleeding.
How does Hemophilia B aka Christmas disease Present?
Patients with hemophilia B typically are males that present with excessive bleeding at a young age. Other symptoms, features, and clinical findings associated with hemophilia A include easy bruising, hemarthrosis, and epistasis.
How is Hemophilia B aka Christmas disease Diagnosed?
Hemophilia B is diagnosed with medical history, and clotting factor tests.
How is Hemophilia B aka Christmas disease Treated?
Hemophilia B aka Christmas disease is treated with a concentrated factor IX product when needed.
What is the Prognosis of Hemophilia B aka Christmas disease?
The prognosis of hemophilia B aka Christmas disease is good.