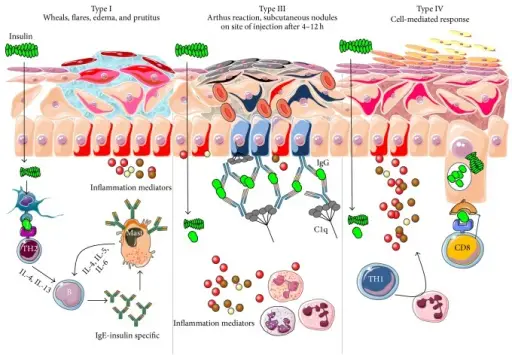
Hypersensitivity reactions are exaggerated or inappropriate immunologic responses occurring in response to an allergen or antigen. There are four types of hypersensitivity reactions that include immediate hypersensitivity reactions or delayed type hypersensitivity reactions. Immediate hypersensitivity reactions occur within 24 hours of exposure to the allergen or antigen. The first three hypersensitivity reactions are antibody-mediated. The the fourth hypersensitivity reaction is mediated primarily by T cells and macrophages.
What are Type I Hypersensitivity Reactions?
Type I hypersensitivity reactions are anaphylactic response that is characterized by an allergic reaction immediately following contact with the antigen. In response to environmental proteins immune system produces IgE antibodies. These antibodies (IgE) bind to mast cells and basophils, which releases histamine, a pharmacological mediator of inflammation that causes rapid vascular leakage and mucosal secretions, often followed by inflammation. These reactions occur within one hour after exposure to an antigen. Examples of immediate type I hypersensitivity reactions include anaphylactic shock, allergic conjunctivitis, allergic rhinitis, bronchial asthma, allergic dermatitis, and food allergy.
The pathophysiology of type I hypersensitivity reactions when mast cells sensitized by IgE are exposed to the allergen, they are activated to secrete inflammatory mediators. Histamine release causes increased vascular permeability and vasodilation, leading to the leak of fluid and plasma proteins into tissues, and stimulates the transient contraction of bronchial and intestinal smooth muscle. Cytokines released by mast cells recruitments leukocytes, which cause the late-phase reaction. The principal leukocytes involved in this reaction are eosinophils, neutrophils, and helper-T-cells.
What are Type II Hypersensitivity Reactions?
Type II hypersensitivity reactions are antibody-mediated cytotoxic hypersensitivity reactions and occurs when antibody binds to antigen on cells and this leads to phagocytosis, killer cell activity, or complement-mediated lysis.
Type II hypersensitivity reactions occur within 2 tp 24 hours.
Examples of antibody mediated type II hypersensitivity reactions include: autoimmune hemolytic anemia, idiopathic thrombocytopenic purpura, Graves’ disease, pernicious anemia, rheumatic fever, myasthenia gravis, Goodpasture syndrome, and pemphigus vulgaris.
The pathophysiology of type II hypersensitivity reactions involves antibodies that cause disease by three main mechanisms inducing inflammation at the site of deposition, opsonizing cells for phagocytosis and interfering with normal cellular functions.
What are Type III Hypersensitivity Reactions?
Type III hypersensitivity reactions are immune complex-mediated hypersensitivity reaction, develops when antibody-antigen complexes are formed in large quantities, or can not be cleared adequately by reticuloendothelial system, leading to serum sickness-type reactions. Tyype III hypersensitivity reactions involve immune complexes that attract complement and leukocytes, which produce localized vascular damage.
Type III hypersensitivity reactions typically occur within 3–6 h after exposure to antigen.
Examples of immune-complex mediated type III hypersensitivity reactions include: systemic lupus erythematosus (SLE), polyarteritis nodosa, and poststreptococcal glomerulonephritis.
The pathophysiology of type III hypersensitivity reactions occurs when immune complexes deposits within blood vessels, tissues, or joints.
What are Type IV Hypersensitivity Reactions?
Type IV hypersensitivity or delayed type hypersensitivity reactions are T cell-mediated reactions and develops when antigen trapped in a macrophage cannot be cleared. T lymphocytes are then stimulated to elaborate lymphokines, which mediate a range of inflammatory responses. The major causes of T cell–mediated hypersensitivity reactions are persistent exagerated immune responses or autoimmunity.
Type IV hypersensitivity reactions occur within 48 to 72 hours.
Examples of immediate type IV hypersensitivity reactions include: multiple sclerosis, rheumatoid arthritis, type 1 diabetes, Crohn disease, psoriasis, and contact sensitivity reactions.
The pathophysiology of type IV hypersensitivity reactions involves excessive polyclonal T cell activation by certain microbial toxins that are produced by some bacteria and viruses that can lead to production of large amounts of inflammatory cytokines. These inflammatory cytokines may cause a syndrome similar to septic shock.