Infectious diseases are disorders caused by living organisms. Infectious organisms include viral infections, bacterial infections, fungal infections, and parasitic infections.
How Do Microorganisms Cause Disease?
Microorganisms cause disease by infiltration and infection.
What are Sexually Transmitted Infections?
Sexually transmitted Infections are the infections which passed from one person to another person through sexual contact.
Sexually transmitted Infections may occur to the following pathogens:
Chlamydiae trachomatis
Ureaplasma urealyticum
Trichomonas vaginallis
Bacteria
Viruses
What is Chlamydiae Trachomatis?
Chlamydiae trachomatis is a sexually transmitted disease caused by bacteria called Chlamydia trachomati.
What is the Pathology of Chlamydiae Trachomatis?
The pathology of chlamydiae trachomatis is:
-Etiology: The cause of chlamydiae trachomatis is Chlamydia trachomatis bacteria.
-Genes involved: ompA.
-Pathogenesis: The sequence of events that lead to chlamydiae trachomatis are infectivity and organism exposure, survival inside host, virulence association, immunity, susceptibility of host to infection.
-Morphology: The morphology associated with chlamydiae trachomatis shows obligate intracellular parasites with elementary bodies and reticulate bodies.
-Histology: The histology associated with chlamydiae trachomatis shows lymphoid germinal centers, plasma cells, and reactive epithelial atypia.
How does Chlamydiae Trachomatis Present?
Patients with chlamydiae trachomatis typically are all genders at the age range of 15–24 years. The symptoms, features, and clinical findings associated with chlamydiae trachomatis include testicular pain, urethral discharge, and painful urination.
How is Chlamydiae Trachomatis Diagnosed?
Chlamydiae trachomatis is diagnosed by swab test and urine test.
How is Chlamydiae Trachomatis Treated?
Chlamydiae trachomatis is treated by antibiotics such as azithromycin, and doxycycline.
What is the Prognosis of Chlamydiae Trachomatis?
The prognosis of chlamydiae trachomatis is good. In women, untreated chlamydia can spread into the uterus or fallopian tubes and cause pelvic inflammatory disease.
What is Ureaplasma urealyticum?
Ureaplasma urealyticum is a type of bacteria that can cause infection of the urinary tract and vagina. It can be passed from mother to infant during birth, or be sexually transmitted.
What is the Pathology of Ureaplasma Urealyticum?
The pathology of ureaplasma urealyticum is:
-Etiology: The cause of ureaplasma urealyticum is sexual contact.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to ureaplasma urealyticum is unknown.
-Morphology: The morphology associated with ureaplasma urealyticum shows gram negative bacteria, bound by a triple-layered “unit membrane” that contains a sterol, causing them to stain as gram negative,125-250 nm in size, highly pleomorphic.
-Histology: The histology associated with ureaplasma urealyticum is not known. Organisms not seen on H&E; expect a chronic inflammatory response.
How does Ureaplasma Urealyticum Present?
Patients with ureaplasma urealyticum typically are all genders at the age range of 26–35years. The symptoms, features, and clinical findings associated with ureaplasma urealyticum include an unpleasant odor, burning sensation, urethral discharge, and pain during urination.
How is Ureaplasma Urealyticum Diagnosed?
Ureaplasma urealyticum is diagnosed by swab test, biopsy, and urine test.
How is Ureaplasma Urealyticum Treated?
Ureaplasma urealyticum is treated by antibiotics azithromycin, doxycycline.
What is the Prognosis of Ureaplasma Urealyticum?
The prognosis of ureaplasma urealyticum is good.
What is Trichomonas Vaginallis?
Trichomonas vaginallis is an anaerobic, flagellated protozoan parasite and the causative agent of trichomoniasis.
What is the Pathology of Trichomonas Vaginallis?
The pathology of trichomonas vaginallis is:
-Etiology: The cause of trichomonas vaginallis is one-celled protozoan.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to trichomonas vaginallis are: upon contact it destroys epithelial cells by the release of cytotoxic substances. It also binds to host plasma proteins, thereby preventing recognition of the parasite by the alternative complement pathway and host proteinases.
-Morphology: The morphology associated with trichomonas vaginallis shows pear shaped organisms that are cyanophilic.
-Histology: The histology associated with trichomonas vaginallis shows presence of eosinophilic cytoplasmic granules.
How does Trichomonas Vaginallis Present?
Patients with trichomonas vaginallis typically are females at the age range of 15 to 35 years. The symptoms, features, and clinical findings associated with trichomonas vaginallis include genital redness, frequent urge to urinate, vaginal discharge, vaginal spotting or bleeding, pain during urination or sexual intercourse.
How is Trichomonas Vaginallis Diagnosed?
Trichomonas vaginallis is diagnosed by swab test, urine test, and nucleic acid amplification test.
How is Trichomonas Vaginallis Treated?
Trichomonas vaginallis is treated by antibiotics such as metronidazole or tinidazole.
What is the Prognosis of Trichomonas Vaginallis?
The prognosis of trichomonas vaginallis is good.
What are Bacterial Sexually Transmitted Infections?
Bacterial sexually transmitted infections are infections caused by bacteria that are sexually transmitted.
Examples of Bacterial Sexually Transmitted Infections include:
Haemophilus ducreyi
Klebsiella granulomatis
Neisseria gonorrhoeae
Treponema pallidum
What is Haemophilus Ducreyi?
Haemophilus ducreyi is the gram-negative, facultative anaerobic bacterium that causes chancroid.
What is the Pathology of Haemophilus Ducreyi?
The pathology of haemophilus ducreyi is:
-Etiology: The cause of haemophilus ducreyi is bacteria.
-Genes involved: lspA1, lspA2 and tadA.
-Pathogenesis: The sequence of events that lead to haemophilus ducreyi are: the pathogen penetrates the skin through breaks in the mucosal barriers and microabrasions on the skin. It produces a cytocidal distending toxin which causes cell cycle arrest and apoptosis/necrosis of human cells and contributes to the aggravation of ulcers.
-Morphology: The morphology associated with haemophilus ducreyi shows gram-negative coccobacilli, non spore-forming, 1.5 µm long and 0.5 µm wide.
-Histology: The histology associated with haemophilus ducreyi shows zonation phenomenon at the ulcer base.
How does Haemophilus Ducreyi Present?
Patients with haemophilus ducreyi typically are all genders at the age range of 21-30 years old. The symptoms, features, and clinical findings associated with haemophilus ducreyi include: pain and bleeding of the sore, dysuria, urethritis, abnormal vaginal discharge.
How is Haemophilus Ducreyi Diagnosed?
Haemophilus ducreyi is diagnosed by PCR, and swab test.
How is Haemophilus Ducreyi Treated?
Haemophilus ducreyi is treated by antibiotics azithromycin, ciprofloxacin, and ceftriaxone.
What is the Prognosis of Haemophilus Ducreyi?
The prognosis of haemophilus ducreyi is good.
What is Klebsiella Granulomatis?
Klebsiella granulomatis is Gram-negative, rod-shaped bacterium which cause the sexually transmitted disease granuloma inguinale or donovanosis.
What is the Pathology of Klebsiella Granulomatis?
The pathology of klebsiella granulomatis is:
-Etiology: The cause of klebsiella granulomatis is bacteria.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to klebsiella granulomatis is not well characterized but may be due to ingestion by macrophages.
-Morphology: The morphology associated with klebsiella granulomatis shows marked reactive changes in surface epithelium secondary to inflammation and ulceration; marked pseudoepitheliomatous hyperplasia adjacent to ulcer.
-Histology: The histology associated with klebsiella granulomatis shows round shaped gram negative bacteria, non-sporulated capsules measuring 0.5 to 2.0 μm.
How does Klebsiella Granulomatis Present?
Patients with klebsiella granulomatis typically are all genders at an age range of 20-40 years. The symptoms, features, and clinical findings associated with klebsiella granulomatis include foul-smelling genitals, sores, and erythema.
How is Klebsiella Granulomatis Diagnosed?
Klebsiella granulomatis is diagnosed by biopsy, and urine test.
How is Klebsiella granulomatis Treated?
Klebsiella granulomatis is treated by antibiotics such as doxycycline.
What is the Prognosis of Klebsiella Granulomatis?
The prognosis of klebsiella granulomatis is good.
What is Neisseria Gonorrhoea?
Neisseria gonorrhoeae is a bacterial pathogen responsible for gonorrhea.
What is the Pathology of Neisseria Gonorrhoea?
The pathology of neisseria gonorrhoeae is:
-Etiology: The cause of neisseria gonorrhoeae is bacteria.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to neisseria gonorrhoeae shows that gonococci attach primarily to columnar and cuboidal epithelium. After 24-48 hours, they penetrate between and through the cells to reach the submucosal tissues where they stimulate a marked neutrophilic response resulting in sloughing of the epithelium, microabscess formation, and the exudation of pus.
-Morphology: The morphology associated with neisseria gonorrhoeae shows acute suppurative reaction, inflammation within mucosa and submucosa only.
-Histology: The histology associated with neisseria gonorrhoeae shows gram negative, non spore forming, nonmotile bacterium.
How does Neisseria Gonorrhoea Present?
Patients with neisseria gonorrhoeae typically are all genders at the age range of 20 and 24 years. The symptoms, features, and clinical findings associated with neisseria gonorrhea include an urge to urinate frequently, heavier periods or spotting, discharge from the vagina, pain or burning sensation while urinating.
How is Neisseria Gonorrhea Diagnosed?
Neisseria gonorrhoeae is diagnosed by urine test, and swab test.
How is Neisseria Gonorrhea Treated?
Neisseria gonorrhea is treated by antibiotics ceftriaxone, and azithromycin.
What is the Prognosis of Neisseria Gonorrhoea?
The prognosis of neisseria gonorrhoeae is good. However, untreated gonorrhea can cause serious and permanent health problems in both women and men.
What is Syphilis?
Syphilis is a disease caused by Treponema pallidum.
What is the Pathology of Syphilis?
The pathology of syphilis is:
-Etiology: The cause of syphilis is a spirochete organism called treponema pallidum.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to syphilis is when treponema pallidum enters an individual byby sexual contact, and penetrate through intact mucous membrane and invade the blood stream, enters other body parts causing the progressive tissue destruction.
-Morphology: The morphology associated with treponema pallidum shows a two-layered outer wall, a cytoplasmic membrane proper, cytoplasm and a bunch of fibrils following a different path in different places on the treponema.
-Histology: The histology associated with treponema pallidum shows papulosquamous thin papules, rash, moth-eaten alopecia and coiled spirochetes.
How does Syphilis Present?
Patients with syphilis typically are all genders at the age range of 25–34 years. The symptoms, features, and clinical findings associated with treponema pallidum include weight loss, muscle aches, fatigue, fever, swollen lymph glands.
How is Syphilis Diagnosed?
Syphilis is diagnosed by PCR, and blood test.
How is Syphilis Treated?
Syphilis is treated by antibiotics such as benzathine penicillin
What is the Prognosis of Syphilis
The prognosis of treponema pallidum is good if it does not enter the body organs. Antibiotics can cure the infection, but there’s no way to repair organs that have been damaged by syphilis.
What are Viral Sexually Transmitted Infections?
Viral sexually transmitted infections are caused by viruses.
Examples of viral sexually transmitted infections include:
Human papillomavirus
Herpes simplex virus
Hepatitis B virus
Human immunodeficiency virus
What is Human Papillomavirus?
Human papillomavirus is the most common sexually transmitted infection.it is usually harmless but some types can lead to cancer or genital warts.
What is the Pathology of Human Papillomavirus?
The pathology of human papillomavirus is:
-Etiology: The cause of human papillomavirus is skin-to-skin contact, sexual contact.
-Genes involved: E1, E7
-Pathogenesis: The sequence of events that lead to human papillomavirus is keratinocyte infection by human papillomavirus, resulting in cutaneous or mucosal excrescences known as warts.
-Morphology: The morphology associated with human papillomavirus shows warts or skin changes.
-Histology: The histology associated with human papillomavirus shows that the squamous intraepithelial lesions with nuclear atypia, chromatin that is coarse, and increased nuclear to cytoplasmic ratios.
How does Human Papillomavirus Present?
Patients with human papillomavirus typically are all genders at the age range of 15 and 25 years. The symptoms, features, and clinical findings associated with human papillomavirus include genital warts, cervical cancer, plantar warts, and flat warts.
How is Human Papillomavirus Diagnosed?
Human papillomavirus is diagnosed by DNA test, Pap test, and vinegar solution test.
How is Human Papillomavirus Treated?
Human papillomavirus is treated by medications, or surgery.
What is the Prognosis of Human Papillomavirus?
The prognosis of human papillomavirus is good.
What is Herpes Simplex Virus?
Herpes simplex virus is an infection that appears in various parts of the body, most commonly on the genitals or mouth.
What is the Pathology of Herpes Simplex Virus?
The pathology of herpes simplex virus is:
-Etiology: The cause of herpes simplex virus is direct contact, sexual contact.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to herpes simplex virus shows that during lytic replication HSV produces infectious viral particles to infect other cells and organisms, while during latency there is limited gene expression and lack of infectious virus particles.
-Morphology: The morphology associated with herpes simplex virus shows open scalloped sores, or sores in the process of healing.
-Histology: The histology associated with herpes simplex virus shows multinucleated giant cells with ground glass nuclei.
How does Herpes Simplex Virus Present?
Patients with herpes simplex virus typically are all genders at age range of 14 – 49years. The symptoms, features, and clinical findings associated with herpes simplex virus include fever, pain with urination, tingling sensations, and skin sores.
How is Herpes Simplex Virus Diagnosed?
Herpes simplex virus is diagnosed by blood test.
How is Herpes Simplex Virus Treated?
Herpes simplex virus is treated by antiviral medications such as acyclovir, famciclovir, and valacyclovir.
What is the Prognosis of Herpes Simplex Virus?
The prognosis of herpes simplex virus is fair.
What is Hepatitis B Virus?
Hepatitis B virus is a virus that causes hepatitis inflammation of the liver.
What is the Pathology of Hepatitis B Virus?
The pathology of hepatitis B virus is:
-Etiology: The cause of hepatitis B virus is a virus named hepatitis B.
-Genes involved: HLA-DPA1, HLA-DPB1.
-Pathogenesis: The sequence of events that lead to hepatitis B virus is becoming exposed to the virus.
-Morphology: The morphology associated with hepatitis B is typically appreciable on the liver.
-Histology: The histology associated with hepatitis B virus shows ground glass hepatocytes with ballooning degeneration.
How does Hepatitis B Virus Present?
Patients with hepatitis B virus typically are all genders at age range of 40-49 years.The symptoms, features, and clinical findings associated with hepatitis B virus include abdominal pain, dark urine, clay-colored bowel movements, nausea, vomiting, fatigue, and loss of appetite.
How is Hepatitis B Virus Diagnosed?
Hepatitis B virus is diagnosed by blood test, and liver ultrasound.
How is Hepatitis B Virus Treated?
Hepatitis B virus is treated by antiviral medications, and potentially a liver transplant.
What is the Prognosis of Hepatitis B Virus?
The prognosis of hepatitis B virus is good. Most adults with hepatitis B recover fully and disease does not become chronic, and there are no long-term health implications.
What is Human Immunodeficiency Virus?
Human immunodeficiency virus is a virus that attacks the body’s immune system. If it is not treated, it can lead to AIDS.
What is the Pathology of Human Immunodeficiency Virus?
The pathology of human immunodeficiency virus is:
-Etiology: The cause of human immunodeficiency virus is a virus.
-Genes involved: HLA class I.
-Pathogenesis: The sequence of events that lead to human immunodeficiency virus are: the virus enters the body and replicates inside T helper cells and kills them, which are required for almost all adaptive immune responses hence causing AIDS.
-Morphology: The morphology associated with human immunodeficiency virus shows conical or pear-shaped, lipid envelope and 100 nm in diameter.
-Histology: The histology associated with human immunodeficiency virus shows hyperplasia, multinucleated syncytia of T cells, and loss of the normal follicular dendritic network.
How does Human Immunodeficiency Virus Present?
Patients with human immunodeficiency virus typically are all genders at the age range of 25 to 29 years. The symptoms, features, and clinical findings associated with human immunodeficiency virus include swollen lymph nodes, diarrhea, weight loss, fatigue, night sweats, rash, sore throat, fever, and headache.
How is Human Immunodeficiency Virus Diagnosed?
Human immunodeficiency virus is diagnosed by ELISA test.
How is Human Immunodeficiency Virus Treated?
Human immunodeficiency virus is treated by antiretroviral therapy.
What is the Prognosis of Human Immunodeficiency Virus?
The prognosis of human immunodeficiency virus is poor. The average time from infection to death is 8-10 years without proper treatment.
What are the Inflammatory Responses to Infection?
The inflammatory response to Infection occurs when tissues are injured by bacteria, trauma, toxins, heat, or any other cause.
Examples of inflammatory responses to Infection include:
Cytopathic-cytoproliferative reaction
Tissue necrosis
Suppurative inflammation
Granulomatous inflammation
Chronic inflammation and scarring
How are Infectious Agents Diagnosed?
Infectious agents may be diagnosed with special techniques that include:
Acid-fast stain
Gram stain
Mucicarmine stain
Periodic acid-Schiff (PAS) stain
Silver stain
Antibody stain
Culture
DNA probes
Matrix-assisted laser desorption/ionization-time of flight (MALDI-TOF)
How does Acid-Fast Stain Help Diagnose Infectious Agents?
Acid-fast stain is used to differentiate acid fast organisms such as mycobacteria.
Acid-fast stain helps diagnose infectious agents by staining smear with carbol fuchsin, a lipid soluble phenol, which penetrates through lipoidal wall and enters into cytoplasm by heat application. Then the cell appears red, decolorized cells absorb the counter stain and take its color and appear blue while acid-fast cells retain the red color.
How does Gram stain help diagnose infectious agents?
Gram stain is a method of staining used to classify bacterial species into two large groups, gram-positive bacteria and gram-negative bacteria.
How does Mucicarmine stain help diagnose infectious agents?
Mucicarmine stain is intended for the staining of mucin, a secretion produced by a variety of epithelial cells and connective tissue cells.
How does Periodic Acid-Schiff PAS stain help diagnose infectious agents?
Periodic Acid-Schiff PAS stain is a staining method used to detect polysaccharides such as glycogen, and mucosubstances such as glycoproteins, glycolipids and mucins in tissues.
How does Silver Stain help diagnose infectious agents?
Silver Stain is a very sensitive method for detecting small amounts of proteins and low-molecular-weight nucleic acids in polyacrylamide gels.
How does Antibody stain help diagnose infectious agents?
Antibody stain is the use of an antibody-based method to detect a specific protein.
How does Culture help diagnose infectious agents?
Culture is a method used to identify the organisms suspected of causing an infection.
How do DNA Probes help diagnose infectious agents?
DNA probes are important tools in diagnostics to ensure high specificity and sensitivity. They are used in molecular biology methods like PCR, qPCR.
How does Matrix-assisted laser desorption/ionization-time of flight MALDI-TOF help diagnose infectious agents?
Matrix-assisted laser desorption/ionization-time of flight MALDI-TOF is high throughput technology based on the comparison of the protein fingerprint obtained by microbial cells with a database of reference spectra by means of the use of various algorithms.
What are Viral Infections?
Viral Infections are proliferation of a harmful virus inside the body.
Examples of viral infections include:
Coronavirus
Cytomegalovirus
Herpes simplex virus
Measles
Mumps
Polio
Varicella-zoster virus
Viral hemorrhagic fever
West Nile virus
What is Coronavirus?
Coronavirus is a virus that can cause mild to severe respiratory illness, including death.
What is the Pathology of Coronavirus?
The pathology of coronavirus is:
-Etiology: The cause of coronavirus is a virus strain.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to coronavirus are: the virus accesses host cells via the receptor for the enzyme angiotensin-converting enzyme 2 ACE2, which is most abundant on the surface of type II alveolar cells of the lungs.
-Morphology: The morphology associated with coronavirus shows host membrane-derived lipid bilayer encapsulating the helical nucleocapsid comprising viral RNA, 70-90nm in size.
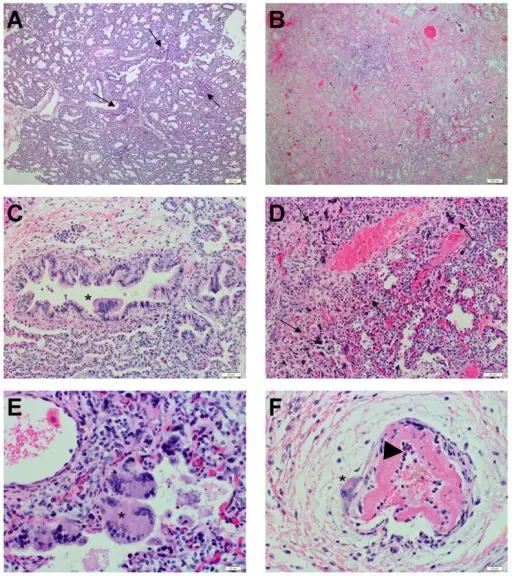
-Histology: The histology associated with coronavirus shows diffuse alveolar damage and fibrinoid necrosis.
How does Coronavirus Present?
Patients with coronavirus typically are all genders at the age range of 45 years and older. The symptoms, features, and clinical findings associated with coronavirus include: tiredness, loss of taste or smell, fever, cough.
How is Coronavirus Diagnosed?
Coronavirus is diagnosed by laboratory tests such as nasopharyngeal swab, throat swab or saliva.
How is Coronavirus Treated?
Coronavirus is treated by self-care, medication.
What is the Prognosis of CoronaVirus?
The prognosis of coronavirus is good.
What is Cytomegalovirus?
Cytomegalovirus is a kind of herpesvirus which usually produces very mild symptoms but may cause severe neurological damage in people with weakened immune systems and in the newborn.
What is the Pathology of Cytomegalovirus?
The pathology of cytomegalovirus is:
-Etiology: The cause of cytomegalovirus is direct contact with saliva or urine, sexual contact, bone marrow transplantation.
-Genes involved: UL35, UL73, UL74, UL75, UL100, and UL115.
-Pathogenesis: The sequence of events that lead to cytomegalovirus are: Upon initial infection, CMV infects the epithelial cells of the salivary gland, resulting in a persistent infection and viral shedding.
-Morphology: The morphology associated with cytomegalovirus shows outer lipid bilayer envelope, composed of various viral glycoproteins, followed by the tegument, a proteinaceous matrix, which holds double stranded linear DNA core in an icosahedral nucleocapsid. The virion is usually spherical in composition.
-Histology: The histology associated with cytomegalovirus shows thickened nuclear membrane, coarse red intracytoplasmic granules and increased apoptotic bodies.
How does Cytomegalovirus Present?
Patients with cytomegalovirus typically are all genders at all ages. The symptoms, features, and clinical findings associated with cytomegalovirus include feeling sick, sore throat, swollen glands, tiredness, skin rash, a high temperature, and aching muscles.
How is CytomegaloVirus Diagnosed?
Cytomegalovirus is diagnosed by laboratory tests such as PCR.
How is CytomegaloVirus Treated?
Cytomegalovirus is treated by antiviral medications.
What is the Prognosis of CytomegaloVirus?
The prognosis of cytomegalovirus is good. Most patients recover completely.
What is Measles?
Measles is an acute viral respiratory illness. It causes a total-body skin rash and flu.
What is the Pathology of Measles?
The pathology of measles is:
-Etiology: The cause of measles is a virus called morbillivirus.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to measles are: the virus first infects and replicates in epithelial cells of the respiratory tract, and then infects the regional lymphoid organs. From there, infected monocytes disseminate the virus during the viremic phase.
-Morphology: The morphology associated with measles shows enveloped, pleomorphic spheres 100-300 nm in diameter.
-Histology: The histology associated with measles shows epithelial giant cells with viral inclusions, nuclei may contain a single large Cowdry type A inclusion, and reticuloendothelial giant cells in lymphoid tissue.
How does Measles Present?
Patients with measles typically are all genders at an age range of 5 to 20 years. The symptoms, features, and clinical findings associated with measles include: watery eyes, cough, runny nose, high fever, small red spots.
How is Measles Diagnosed?
Measles is diagnosed by laboratory blood and tissue tests.
How is Measles Treated?
Measles is treated by antibiotics, vaccination.
What is the Prognosis of Measles?
The prognosis of measles is good.
What are Mumps?
Mumps is a contagious disease caused by a virus and it occurs with a few days of fever, headache, muscle aches, tiredness, and loss of appetite.
What is the Pathology of Mumps?
The pathology of mumps is:
-Etiology: The cause of mumps is a virus that spreads through infected saliva.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to mumps are not exactly known, but upon virus infection, lymphocytic infiltration and destruction of periductal cells occur which leads to blockage of the ducts in the salivary glands and the seminiferous tubules of the testes, respectively.
-Morphology: The morphology associated with mumps shows single stranded, non-segmented negative RNA, 15384 nucleotides long.
-Histology: The histology associated with mumps shows enlarged lymph nodes.
How does Mumps Present?
Patients with mumps typically are all genders, mostly males at an age range of between 4 and 6 years of age. The symptoms, features, and clinical findings associated with mumps include muscle aches, fatigue, loss of appetite, headache, and fever.
How is Mumps Diagnosed?
Mumps is diagnosed by swab test, blood test.
How is Mumps Treated?
Mumps is treated by medications, diet.
What is the Prognosis of Mumps?
The prognosis of mumps is good. Children fully recover within a few weeks while in adults, the illness is more likely to be severe.
What is Polio?
Polio or poliomyelitis is a disabling and life-threatening disease caused by the poliovirus.
What is the Pathology of Polio?
The pathology of polio is:
-Etiology: The cause of polio is infected feces, contaminated food, and the polio virus.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to polio are: virus enters in intestines and replicates there, then invades local lymphoid tissue and may enter the bloodstream, and then infect cells of the central nervous system. The virus-induced destruction of motor neurons of the spinal cord and brain stem cells results in distinctive paralysis.
-Morphology: The morphology associated with polio shows a diameter of 25 to 30 nm. Its outer coat or capsid is composed of 60 protomers each made of 4 virion proteins VP1, VP2, VP3, and VP4 arranged in icosahedral symmetry.
-Histology: The histology associated with polio shows vacuolation and infiltration.
How does Polio Present?
Patients with polio typically are children at an age range under 5 years . The symptoms, features, and clinical findings associated with polio include neck pain, stiffness, pain in the arms fatigue, and back pain.
How is Polio Diagnosed?
Polio is diagnosed by cerebrospinal fluid, saliva, and stool tests.
How is Polio Treated?
Polio is treated by medications, physiotherapy.
What is the Prognosis of Polio?
The prognosis of polio is good. The majority recover with no complications; however, patients with paralytic polio may become disabled for their whole life.
What is Varicella-Zoster Virus?
Varicella-Zoster virus is ubiquitous human alpha herpesvirus that causes varicella chicken pox and herpes zoster shingles
What is the Pathology of Varicella-Zoster Virus?
The pathology of varicella-zoster virus is:
-Etiology: The cause of varicella-zoster virus is varicella-zoster virus.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to varicella-zoster virus are: the virus enters the host through the respiratory tract and replicates at the site of entry in the nasopharynx and in regional lymph nodes, and then enters other organs causing the infection of skin.
-Morphology: The morphology associated with varicella-zoster virus shows sores on a dermatome .
-Histology: The histology associated with varicella-zoster virus shows keratinocytes are multinucleated, acantholytic with distinct nuclear inclusions, found initially in follicular epithelium. The Tzanck preparation shows characteristic findings of giant cells with multiple nuclei.
How does Varicella-Zoster Virus Present?
Patients with varicella-zoster virus typically are all genders at an age range of 45-64 years. The symptoms, features, and clinical findings associated with varicella-zoster virus include loss of appetite, fever, tiredness, and headache.
How is Varicella-Zoster Virus Diagnosed?
Varicella-zoster virus is diagnosed by lab test blood test, a culture of lesion samples.
How is Varicella-Zoster Virus Treated?
Varicella-zoster virus is treated by medications oral acyclovir, famciclovir, and valacyclovir.
What is the Prognosis of Varicella-Zoster Virus?
The prognosis of varicella-zoster virus is good. Very rarely, shingles can lead to pneumonia, hearing problems, blindness, brain inflammation encephalitis or death.
What is Viral Hemorrhagic Fever?
Viral Hemorrhagic Fever is an infectious disease that can cause severe, and life-threatening illness.
What is the Pathology of Viral Hemorrhagic Fever?
The pathology of viral hemorrhagic fever is:
-Etiology: The cause of disease in lower case is virus, infected animals or insects.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to viral hemorrhagic fever shows deficiency of hepatic synthesis of coagulation factors owing to hepatocellular necrosis, cytokine storm, increased permeability by vascular endothelial growth factor, complement activation.
-Morphology: The morphology associated with viral hemorrhagic fever shows that the arena-, bunya-, and flaviviruses are spherical, while the filoviruses are long and filamentous. All of the hemorrhagic fever viruses are ‘enveloped’ – that is, their surface glycoprotein molecules are anchored in a lipid bilayer derived from host cell membranes.
-Histology: The histology associated with viral hemorrhagic fever is unclear.
How does Viral Hemorrhagic Fever Present?
Patients with viral hemorrhagic fever typically are all genders at the age range of 25–45 years old. The symptoms, features, and clinical findings associated with viral hemorrhagic fever include Muscle aches, Loss of strength, Exhaustion, Dizziness, Fatigue, fever.
How is Viral Hemorrhagic Fever Diagnosed?
Viral hemorrhagic fever is diagnosed by blood and urine tests.
How is Viral Hemorrhagic Fever Treated?
Viral hemorrhagic fever is treated by antiviral drug ribavirin.
What is the Prognosis of Viral Hemorrhagic Fever?
The prognosis of viral hemorrhagic fever is fair. Severe cases can cause life-threatening complications including edema, failure of organs including lungs, kidneys and brain, and internal bleeding.
What is West Nile Virus?
West Nile virus is a single-stranded RNA virus that causes West Nile fever by biting an infected mosquito.
What is the Pathology of West Nile Virus?
The pathology of west nile virus is:
-Etiology: The cause of West Nile virus is the bite of an infected female mosquito.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to west Nile virus are the virus enters through peripheral inoculation and initial replication of virus is occured in skin Langerhans dendritic cells. These cells migrate to and seed draining lymph nodes, resulting in a primary viremia and subsequent infection of peripheral tissues such as the spleen and kidney.
-Morphology: The morphology associated with west nile virus shows positive-stranded RNA virus surrounding an icosahedral capsid of approximately 50 nm in size.
-Histology: The histology associated with west nile virus shows perivascular lymphocytic infiltrates, microglial nodules, neuronal loss, and neuronophagia.
How does West Nile Virus Present?
Patients with west nile virus typically are all genders of all ages. The symptoms, features, and clinical findings associated with west nile virus include: vomiting, diarrhea, rash, body aches, joint pains, headache.
How is West Nile Virus Diagnosed?
West Nile virus is diagnosed by special laboratory tests.
How is West Nile Virus Treated?
West Nile virus is treated by antiemetic therapy, and medications.
What is the Prognosis of West Nile Virus?
The prognosis of west nile virus is excellent. Most infections 70%-80% are asymptomatic and self-limited.
What are Bacterial Infections?
Bacterial Infections occur when bacteria enter the body, increase in number, and cause a reaction in the body.
Bacterial Infections include:
Gram-positive bacterial infections
Gram-negative bacterial infections
Mycobacteria bacterial infections
Spirochete bacterial infections
Anaerobic bacterial infections
Obligate intracellular bacterial infections
What are Gram-Positive Bacterial Infections?
Gram-positive bacterial Infections are caused by gram-positive bacteria such as methicillin-resistant Staphylococcus aureus MRSA, vancomycin-resistant enterococci VRE, and Clostridium difficile.
Examples of gram-positive bacterial infections include:
Anthrax
Diphtheria
Enterococcal
Listeriosis
Nocardia
Staphylococcal
Streptococcal
What is Anthrax Bacterial Infection?
Anthrax bacterial infection is a serious infectious disease caused by gram-positive, rod-shaped bacteria known as Bacillus anthracis.
What is the Pathology of Anthrax Bacterial Infection?
The pathology of anthrax bacterial infection is:
-Etiology: The cause of anthrax bacterial infection is exposure to Bacillus anthracis bacteria.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to anthrax bacterial infection are: the bacteria responsible for the disease enters the body and release the toxins called as anthrax toxins which alter cell signaling pathways in the host to interfere with innate immune responses in early stages of infection and to induce vascular collapse at late stages.
-Morphology: The morphology associated with anthrax bacterial infection shows a gram positive, non-motile, rectangular, aerobic, rod-shaped bacterium.
-Histology: The histology associated with anthrax bacterial infection shows is poorly understood.
How does Anthrax Bacterial Infection Present?
Patients with anthrax bacterial infection typically are all genders at the age range of 30–60 years old. The symptoms, features, and clinical findings associated with anthrax bacterial infection include nausea and vomiting, especially bloody vomiting, diarrhea or bloody diarrhea, headache, sore throat, painful swallowing, and hoarseness.
How is Anthrax Bacterial Infection Diagnosed?
Anthrax bacterial infection is diagnosed by biopsy of skin lesion, blood tests, and chest X-ray.
How is Anthrax Bacterial Infection Treated?
Anthrax bacterial infection is treated by antibiotics, and vaccination.
What is the Prognosis of Anthrax Bacterial Infection?
The prognosis of anthrax bacterial infection is good to poor.
What is Diphtheria Bacterial Infection?
Diphtheria bacterial infection is a serious infection caused by strains of bacteria called Corynebacterium diphtheriae that make a toxin poison.
What is the Pathology of Diphtheria Bacterial Infection?
The pathology of diphtheria bacterial infection is:
-Etiology: The cause of diphtheria bacterial infection is strains of bacteria Corynebacterium diphtheriae.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to diphtheria bacterial infection is the strain of C diphtheriae enters the body and colonizes in the nasopharyngeal cavity or skin, and produces diphtheria toxin in the body hence causing the disease.
-Morphology: The morphology associated with diphtheria bacterial infection shows rod-shaped, Gram-positive, non spore-forming, and nonmotile bacteria.
-Histology: The histology associated with diphtheria bacterial infection shows hyaline degeneration and necrosis with inflammation in the interstitial spaces.
How does Diphtheria Bacterial Infection Present?
Patients with diphtheria bacterial infection typically are all genders with an age range of 5 over 60 years old. The symptoms, features, and clinical findings associated with diphtheria bacterial infection include fever and chills, tiredness, sore throat and hoarseness.
How is Diphtheria Bacterial Infection Diagnosed?
Diphtheria bacterial infection is diagnosed by swab test.
How is Diphtheria Bacterial Infection Treated?
Diphtheria bacterial infection is treated by antibiotics.
What is the Prognosis of Diphtheria Bacterial Infection?
The prognosis of diphtheria bacterial infection is good to poor depending upon how early the patient is treated, and how the patient responds to treatment.
What is Enterococcal Bacterial Infection?
Enterococcal bacterial infection is gram-positive facultative anaerobic cocci in short and medium chains, which cause difficult to treat infections in the nosocomial setting.
What is the Pathology of Enterococcal Bacterial Infection?
The pathology of enterococcal bacterial infection is:
-Etiology: The cause of enterococcal bacterial infection is poor hygiene spread from person to person.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to enterococcal bacterial infection involves by inducing platelet aggregation and tissue factor-dependent fibrin production.
-Morphology: The morphology associated with enterococcal bacterial infection shows gram-positive spherical or ovoid cells arranged in pairs or chains, non-spore-forming facultative anaerobes and obligate fermentative chemoorganotrophs.
-Histology: The histology associated with enterococcus bacteria is non specific.
How does Enterococcal Bacterial Infection Present?
Patients with enterococcal bacterial infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with enterococcal bacterial infection include: pain or burning when you urinate, nausea, vomiting, fever, chills, fatigue, headache, and abdominal pain.
How is Enterococcal Bacterial Infection Diagnosed?
Enterococcal bacterial infection is diagnosed by blood test, and urine test.
How is Enterococcal Bacterial Infection Treated?
Enterococcal bacterial infection is treated by antibiotics penicillin, ampicillin, amoxicillin, piperacillin, or vancomycin
What is the Prognosis of Enterococcal Bacterial Infection?
The prognosis of enterococcal bacterial infection is fair. Such infections can often be difficult to treat, as ordinary doses of antibiotics typically aren’t strong enough to effectively treat them.
What is Listeriosis Bacterial Infection?
Listeriosis bacterial infection is a serious infection usually caused by eating food contaminated with the bacterium Listeria monocytogenes.
What is the Pathology of Listeriosis Bacterial Infection?
The pathology of listeriosis bacterial infection is:
-Etiology: The cause of listeriosis bacterial infection is eating improperly processed meats and unpasteurized milk products.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to listeriosis bacterial infection are: the bacteria pass directly from cell to cell by a mechanism involving host cell actin polymerization, and the bacteria penetrate the intestinal wall and then invade neighboring enterocytes by basolateral spread, leading to enteritis.
-Morphology: The morphology associated with listeriosis bacterial infection shows gram-positive, short rods.
-Histology: The histology associated with listeriosis bacterial infection shows mixed acute and chronic inflammatory infiltrate in the dermis including prominent macrophages with intracellular and free coccobacillus.
How does Listeriosis Bacterial Infection Present?
Patients with listeriosis bacterial infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with listeriosis bacterial infection include nausea, diarrhea, chills, muscle aches, and fever.
How is Listeriosis Bacterial Infection Diagnosed?
Listeriosis bacterial infection is diagnosed by laboratory test.
How is Listeriosis Bacterial Infection Treated?
Listeriosis bacterial infection is treated by antibiotics.
What is the Prognosis of Listeriosis Bacterial Infection?
The prognosis of listeriosis bacterial infection is good.
What is Nocardia Bacterial Infection?
Nocardia bacterial infection is a disease caused by bacteria found in soil and water.
What is the Pathology of Nocardia Bacterial Infection?
The pathology of nocardia bacterial infection is:
-Etiology: The cause of nocardia bacterial infection is bacteria.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to nocardia bacterial infection involves virulence factors which include filamentous growth, mycolic acid, catalases and superoxide dismutases
-Morphology: The morphology associated with nocardia bacterial infection shows gram positive, catalase positive bacilli with thin filamentous branching, often with a beaded appearance
-Histology: The histology associated with nocardia bacterial infection shows pyogranulomatous inflammation and fibrosis and may contain tissue granules of variable diameter.
How does Nocardia Bacterial Infection Present?
Patients with nocardia bacterial infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with nocardia bacterial infection include bloody sputum, sweats, chills, weakness, lack of appetite, weight loss, chest pain, cough, and labored breathing.
How is Nocardia Bacterial Infection Diagnosed?
Nocardia bacterial infection is diagnosed by biopsy.
How is Nocardia Bacterial Infection Treated?
Nocardia bacterial infection is treated by antibiotics.
What is the Prognosis of Nocardia Bacterial Infection?
The prognosis of nocardia bacterial infection is fair.
What is Staphylococcal Bacterial Infection?
Staphylococcal bacterial infection is caused by staphylococcus bacteria commonly found on the skin or in the nose of even healthy individuals.
What is the Pathology of Staphylococcal Bacterial Infection?
The pathology of staphylococcal bacterial infection is:
-Etiology: The cause of staphylococcal bacterial infection is staphylococcus bacteria.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to staphylococcal bacterial infection are when S. aureus inoculates into an open wound, and upon contact with mucosal surface it upregulates the virulence genes which cause the activation of the immune system.
-Morphology: The morphology associated with staphylococcal bacterial infection shows gram-positive, non spore forming, facultatively anaerobic, nonmotile, catalase-positive or negative, small, spherical bacteria from pairs to, and grape-like clusters.
-Histology: The histology associated with staphylococcal bacterial infection shows gram positive cocci in clusters.
How does Staphylococcal Bacterial Infection Present?
Patients with staphylococcal bacterial infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with staphylococcal bacterial infection include sore, red eyelids or eyes, and painful red lump or bump on the skin.
How is Staphylococcal Bacterial Infection Diagnosed?
Staphylococcal bacterial infection is diagnosed by echocardiogram, tissue sample or nasal secretions.
How is Staphylococcal Bacterial Infection Treated?
Staphylococcal bacterial infection is treated by antibiotics and drainage of the infected area.
What is the Prognosis of Staphylococcal Bacterial Infection?
The prognosis of staphylococcal bacterial infection is fair. When these infections are left untreated, they can lead to organ failure and death.
What is Streptococcal Bacterial Infection?
Streptococcal bacterial infection is any type of infection caused by the group of bacteria.
What is the Pathology of Streptococcal Bacterial Infection?
The pathology of streptococcal bacterial infection is:
-Etiology: The cause of streptococcal bacterial infection is Streptococcus.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to streptococcal bacterial infection the bacteria enters and colonizes the upper respiratory tract and invades epithelial cells, where it produces toxins which are responsible for host cell damage and inflammatory response.
-Morphology: The morphology associated with streptococcal bacterial infection shows gram-positive cocci in chains or clusters.
-Histology: The histology associated with streptococcal bacterial infection shows inflammation with polymorph neutrophil infiltration, cytotoxic effects, and necrosis.
How does Streptococcal Bacterial Infection Present?
Patients with streptococcal bacterial infection typically are all genders of all age groups. The symptoms, features, and clinical findings associated with streptococcal bacterial infection include fever, headache, tender lymph nodes, and pain with swallowing.
How is Streptococcal Bacterial Infection Diagnosed?
Streptococcal bacterial infection is diagnosed by swab test.
How is Streptococcal Bacterial Infection Treated?
Streptococcal bacterial infection is treated by medications such as penicillin and amoxicillin.
What is the Prognosis of Streptococcal Bacterial Infection?
The prognosis of streptococcal bacterial infection is fair. An untreated infection with a pus-filled discharge can remain infectious for months.
What are Gram-Negative Bacterial Infections?
Gram-negative bacterial infections are caused infections including pneumonia, bloodstream infections, wound or surgical site infections, and meningitis.
Examples of gram-negative bacterial infections:
Chancroid
Granuloma inguinale
Neisseria
Pertussis
Plague
What is Chancroid?
Chancroid is caused by the bacterium Haemophilus ducreyi and results in painful, superficial ulcers, often with regional lymphadenopathy.
What is the Pathology of Chancroid?
The pathology of chancroid is:
-Etiology: The cause of chancroid is Haemophilus ducreyi bacteria.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to chancroid is: the bacteria enter the skin through disrupted mucosa and cause a local inflammatory reaction.
-Morphology: The morphology associated with chancroid shows small gram-negative rods.
-Histology: The histology associated with chancroid shows the zonation phenomenon at the ulcer base.
How does Chancroid Present?
Patients with chancroid typically are all genders with an age range of 21-30 years old. The symptoms, features, and clinical findings associated with chancroid include: rectal bleeding, pain with bowel movements, dyspareunia, painful urination, vaginal discharge.
How is Chancroid Diagnosed?
Chancroid is diagnosed by antigen detection, serology, and genetic amplification methods.
How is Chancroid Treated?
Chancroid is treated by antibiotics azithromycin.
What is the Prognosis of Chancroid?
The prognosis of chancroid is good. Untreated chancroid conditions may cause permanent scarring on the penis or lead to serious complications in those with a vagina.
What is Granuloma Inguinale?
Granuloma Inguinale is a genital ulcerative disease caused by the intracellular gram-negative bacterium Klebsiella granulomatis.
What is the Pathology of Granuloma Inguinale?
The pathology of granuloma inguinale is:
-Etiology: The cause of granuloma inguinale is intracellular gram-negative bacterium Klebsiella granulomatis.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to granuloma inguinale includes bacterial infection associated with sexually transmitted disease or via childbirth with infected genital tract
-Morphology: The morphology associated with granuloma inguinale shows papules or nodules that arise at the site of inoculation. The nodule is soft, often pruritus and erythematous, and eventually ulcerates.
-Histology: The histology associated with granuloma inguinale shows massive plasma cells infiltrate without lymphocytes in granulation tissue.
How does Granuloma Inguinale Present?
Patients with granuloma inguinale typically. The symptoms, features, and clinical findings associated with granuloma inguinale include destroyed genital tissue, beefy-red bumps, and sores in the anal area.
How is Granuloma Inguinale Diagnosed?
Granuloma inguinale is diagnosed by biopsy.
How is Granuloma Inguinale Treated?
Granuloma inguinale is treated by antibiotics trimethoprim-sulfamethoxazole, doxycycline, erythromycin, and ciprofloxacin.
What is the Prognosis of Granuloma Inguinale?
The prognosis of granuloma inguinale is good if appropriate treatment is started early. If left untreated, it can cause significant scarring and tissue destruction.
What is Neisseria bacterial infection?
Neisseria bacterial infection causes meningococcal disease. About 1 in 10 people have these bacteria in the back of their nose and throat without being ill.
What is the Pathology of Neisseria Bacterial Infection?
The pathology of neisseria bacterial infection is:
-Etiology: The cause of neisseria bacterial infection is bacteria, close contact with infected people.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to neisseria bacterial infection shows that gonococci attach primarily to columnar and cuboidal epithelium. After 24-48 hours, they penetrate between and through the cells to reach the submucosal tissues where they stimulate a marked neutrophilic response resulting in sloughing of the epithelium, microabscess formation, and the exudation of pus.
-Morphology: The morphology associated with neisseria Bacterial Infection shows gram negative, non-spore-forming, nonmotile bacterium.
-Histology: The histology associated with neisseria bacterial infection shows acute suppurative reaction, inflammation within mucosa and submucosa only.
How does Neisseria Bacterial Infection Present?
Patients with neisseria bacterial infection typically are all genders but mostly children with age less than 1 year old. The symptoms, features, and clinical findings associated with neisseria bacterial infection include nausea or vomiting, cold hands and feet, rapid breathing, fever, chills, and severe aches and pain.
How is Neisseria Bacterial Infection Diagnosed?
Neisseria bacterial infection is diagnosed by lab tests.
How is Neisseria Bacterial Infection Treated?
Neisseria bacterial infection is treated by antibiotics.
What is the Prognosis of Neisseria Bacterial Infection?
The prognosis of neisseria bacterial infection is fair. In women, the bacteria can spread into the uterus or fallopian tubes and cause pelvic inflammatory disease.
What is Pertussis bacterial infection?
Pertussis bacterial infection also called whooping cough. It is a serious lung infection caused by bacteria and gets into the nose and throat.
What is the Pathology of Pertussis Bacterial Infection?
The pathology of pertussis bacterial infection is:
-Etiology: The cause of pertussis bacterial infection is Bordetella pertussis.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to pertussis bacterial infection is when the bacteria is transmitted by aerosols and infects the ciliated epithelium of the airways, bacteria produces toxins in the respiratory tract which kills ciliated cells and causes their extrusion from the mucosa.
-Morphology: The morphology associated with pertussis bacterial infection shows small (approximately 0.8 μm by 0.4 μm), rod-shaped, coccoid, or ovoid Gram-negative bacterium that is encapsulated and does not produce spores. It is a strict aerobe. It is arranged singly or in small groups and is not easily distinguished from Haemophilus species.
-Histology: The histology associated with pertussis bacterial infection shows descending infection dominated by necrotizing bronchiolitis, intra-alveolar hemorrhage, and fibrinous edema.
How does Pertussis Bacterial Infection Present?
Patients with disease in lower case typically are all genders of all ages. The symptoms, features, and clinical findings associated with pertussis bacterial infection include exhaustion, Paroxysms, Vomiting.
How is Pertussis Bacterial Infection Diagnosed?
Pertussis bacterial infection is diagnosed by blood test, samples of mucus in the nose and throat.
How is Pertussis Bacterial Infection Treated?
Pertussis bacterial infection is treated by antibiotics.
What is the Prognosis of Pertussis Bacterial Infection?
The prognosis of pertussis bacterial infection is fair. The infection gradually resolves over weeks, but the coughing paroxysms can persist for several months.
What is the Plague?
The plague is a serious bacterial infection that can be deadly that affects humans and other mammals.
What is the Pathology of Plague?
The pathology of plague is:
-Etiology: The cause of plague is bacterium, Yersinia pestis.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to plague are: when the flea bites the host, the bacteria migrates to the regional lymph nodes, are phagocytosed by mononuclear phagocytes, and multiply intracellularly, subsequently lysis of the phagocytes occur and may lead to invasion of distant organs.
-Morphology: The morphology associated with plague shows coccobacillus-shaped, gram negative bacterium.
-Histology: The histology associated with plague shows necrosuppurative inflammation in the lymph nodes.
How does Plague Present?
Patients with plague typically are all genders of all ages. The symptoms, features, and clinical findings associated with plague include: weakness, swollen lymph nodes, fever, headache, chills.
How is Plague Diagnosed?
Plague is diagnosed by laboratory test blood samples.
How is Plague Treated?
Plague is treated by Antibiotics streptomycin, gentamicin, doxycycline, ciprofloxacin
What is the Prognosis of Plague?
The prognosis of plague is poor. About 50% of people die if their illness is not treated. Treatment reduces the death rate to 50%.
What are Mycobacteria Bacterial Infections?
Mycobacteria Bacterial Infections are a group of multisystem infections caused by the members of the family Mycobacteriaceae.
Examples of mycobacteria bacterial infections include:
Leprosy
Mycobacterium avium complex
Tuberculosis
What is Leprosy?
Leprosy is an infection caused by slow-growing bacteria called Mycobacterium leprae that causes skin lesions and nerve damage.
What is the Pathology of Leprosy?
The pathology of leprosy is:
-Etiology: The cause of leprosy is Mycobacterium leprae.
-Genes involved: HLA-DRB1, HLA-DQA, HLA genes
-Pathogenesis: The sequence of events that lead to leprosy spreads through contact with the mucosal secretions of a person with the infection. This usually occurs when a person with leprosy sneezes or coughs.
-Morphology: The morphology associated with leprosy shows strongly acid-fast, rod-shaped bacterium. It has parallel sides and rounded ends, measuring 1-8 microns in length and 0.2-0.5 micron in diameter, and closely resembles the tubercle bacillus.
-Histology: The histology associated with leprosy shows epithelioid histiocytes surround small cutaneous nerves, Langhans giant cells may be seen but without necrosis.
How does Leprosy Present?
Patients with leprosy typically are all genders of all ages. The symptoms, features, and clinical findings associated with leprosy include thick or dry skin, painless ulcers on the soles of feet, growths on the skin, loss of eyebrows or eyelashes, and discolored patches of skin.
How is Leprosy Diagnosed?
Leprosy is diagnosed by skin biopsy.
How is Leprosy Treated?
Leprosy is treated by antibiotics dapsone and rifampicin.
What is the Prognosis of Leprosy?
The prognosis of leprosy is good.
What is Mycobacterium Avium Complex?
Mycobacterium Avium Complex is a group of bacteria related to tuberculosis. These germs are very common in food, water, and soil.
What is the Pathology of Mycobacterium Avium Complex?
The pathology of mycobacterium avium complex is:
-Etiology: The cause of mycobacterium avium complex is Mycobacterium avium and Mycobacterium intracellular.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to mycobacterium avium complex are: the bacteria spreads through the submucosal tissue, lymphatic drainage transports mycobacteria to abdominal lymph nodes, from which the organisms enter the bloodstream, from where the hematogenous spread occurs to many sites such as spleen, bone marrow, and liver.
-Morphology: The morphology associated with mycobacterium avium complex shows strains that are known to exhibit variation in colony morphology. In addition to the smooth transparent, smooth opaque, and rough opaque.
-Histology: The histology associated with mycobacterium avium complex shows necrotizing and non necrotizing granulomas and positive AFB smear results.
How does Mycobacterium Avium Complex Present?
Patients with mycobacterium avium complex typically are all genders of all ages. The symptoms, features, and clinical findings associated with mycobacterium avium complex include shortness of breath, abdominal pain, anemia, fatigue, diarrhea, sweating, and weight loss.
How is Mycobacterium Avium Complex Diagnosed?
Mycobacterium avium complex is diagnosed by x-rays or CT scan.
How is Mycobacterium Avium Complex Treated?
Mycobacterium avium complex is treated by antimicrobials.
What is the Prognosis of Mycobacterium Avium Complex?
The prognosis of mycobacterium avium complex is good.
What is Tuberculosis?
Tuberculosis is caused by a bacterium called Mycobacterium tuberculosis. The bacteria can attack any part of the body such as the kidney, spine, and brain.
What is the Pathology of Tuberculosis?
The pathology of tuberculosis is:
-Etiology: The cause of tuberculosis is bacteria that spread from person to person through microscopic droplets released into the air.
-Genes involved: EREG gene.
-Pathogenesis: The sequence of events that lead to tuberculosis are: Infection occurs when a person inhales tubercle bacteria which then reaches the alveoli of the lungs and are ingested by alveolar macrophages, then these bacilli may spread by way of lymphatic channels or through the bloodstream to more distant tissues and organs where the disease is developed.
-Morphology: The morphology associated with tuberculosis shows nonmotile rod-shaped bacterium distantly related to the Actinomycetes. The rods are 2-4 micrometers in length and 0.2-0.5 um in width.
-Histology: The histology associated with tuberculosis shows caseating granulomas, cavities show approximation of walls, granulation tissue, fibrosis and stellate scar, may have metaplastic bone formation.
How does Tuberculosis Present?
Patients with tuberculosis typically are all genders of all ages. The symptoms, features, and clinical findings associated with tuberculosis include fever, chills, night sweats, cough, and loss of appetite.
How is Tuberculosis Diagnosed?
Tuberculosis is diagnosed by blood test, or skin test.
How is Tuberculosis Treated?
Tuberculosis is treated by antibacterial medications.
What is the Prognosis of Tuberculosis?
The prognosis of tuberculosis is good if they complete the treatment protocols.
What are Spirochete Bacterial Infections?
Spirochete Bacterial Infections are a group of spiral-shaped bacteria, which are serious pathogens for humans and cause diseases.
Examples of spirochete bacterial infections include:
Lyme disease
Syphilis
What is Lyme Disease?
Lyme Disease is the most common vector-borne disease caused by the bacterium Borrelia burgdorferi.
What is the Pathology of Lyme Disease?
The pathology of lyme disease is:
-Etiology: The cause of lyme disease is bacterium Borrelia burgdorferi and Borrelia mayonii.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to lyme disease are: the bacterium enters the skin at the site of the tick bite, after some days the organisms migrate locally in the skin around the bite, spread via the lymphatics to cause regional adenopathy or disseminate in blood to organs or other skin sites.
-Morphology: The morphology associated with lyme disease shows helical shaped spirochete bacterium. It has an inner and outer membrane as well as a flexible cell wall. Inside the bacteria’s cell membranes is the protoplasm, which, due to the spiral shape of the bacteria, is long and cylindrical.
-Histology: The histology associated with lyme disease shows superficial and deep perivascular polymorphic infiltrate of neutrophils, lymphocytes, plasma cells, eosinophils and mast cells.
How does Lyme Disease Present?
Patients with lyme disease typically are all genders of all ages. The symptoms, features, and clinical findings associated with lyme disease include a characteristic skin rash, headache, fatigue, and fever.
How is Lyme Disease Diagnosed?
Lyme disease is diagnosed by laboratory test antibody tests.
How is Lyme Disease Treated?
Lyme disease is treated by medications such as doxycycline, amoxicillin, and cefuroxime.
What is the Prognosis of Lyme Disease?
The prognosis of lyme disease is excellent when patients are treated early with appropriate antibiotic regimens.
What is Syphilis?
Syphilis is a sexually transmitted infection that can cause serious health problems if it is not treated.
What is the Pathology of Syphilis?
The pathology of syphilis is:
-Etiology: The cause of syphilis is a bacterium called Treponema pallidum.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to syphilis are: bacteria usually transmitted via direct contact, and incubated in the body, and then disseminated to the lymphatics and blood stream to gain access to any organ of the body.
-Morphology: The morphology associated with syphilis shows spiral-shaped bacteria.
-Histology: The histology associated with syphilis shows ulcers with lymphoplasmacytic inflammation.
How does Syphilis Present?
Patients with syphilis typically all genders of age ranges 20–39 years. The symptoms, features, and clinical findings associated with syphilis include: muscle aches, headaches, weight loss, sore throat, patchy hair loss, fever, swollen lymph glands.
How is Syphilis Diagnosed?
Syphilis is diagnosed by blood tests, and enzyme immunoassay tests.
How is Syphilis Treated?
Syphilis is treated by antibiotic medication penicillin.
What is the Prognosis of Syphilis?
The prognosis of syphilis is fair. Antibiotics can cure the infection, but there’s no way to repair organs that have been damaged by syphilis
What are Anaerobic Bacterial Infections?
Anaerobic Bacterial Infections are infections caused by anaerobic bacteria, these bacteria occur naturally and are the most common flora in the body.
Examples of Anaerobic Bacterial Infections include:
Anaerobes causing abscesses
Clostridial infections
What are Anaerobes Causing Abscesses?
Anaerobes causing abscesses are anaerobes that can cause an abscess.
What is the Pathology of Anaerobes Causing Abscesses?
The pathology of anaerobes causing abscesses is:
-Etiology: The cause of anaerobes causing abscesses occurs when deep tissues become injured or exposed.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to anaerobes causing abscesses are: bacteria enters from the gingival crevice and reaches the lower airways and infection is initiated if not cleared by the host defense system. This results in aspiration pneumonitis and progression to tissue necrosis 7-14 days later, resulting in formation of lung abscess.
-Morphology: The morphology associated with anaerobes causing abscesses shows gram-negative bacilli.
-Histology: The histology associated with anaerobes causing abscesses shows abscess formation and necrosis at the site of inoculation.
How does Anaerobes Causing Abscesses Present?
Patients with anaerobes causing abscesses typically in all genders at all ages. The symptoms, features, and clinical findings associated with anaerobes causing abscesses include: smooth swelling under skin, pain and tenderness on affected area, redness, high temperature.
How is Anaerobes Causing Abscesses Diagnosed?
Anaerobes causing abscesses is diagnosed by physical examination, CT scan, and MRI.
How is Anaerobes Causing Abscesses Treated?
Anaerobes causing abscesses is treated by abscess drainage.
What is the Prognosis of Anaerobes Causing Abscesses?
The prognosis of anaerobes causing abscesses is excellent but some individuals may suffer from recurrent abscesses requiring medical attention. Most people do not require antibiotics.
What are Clostridial Infections?
Clostridial Infections are any of several infectious conditions in animals and humans resulting from bacteria Clostridium species that are found in soil and enter the body via wounds or contaminated food.
What is the Pathology of Clostridial Infections?
The pathology of clostridial infections is:
-Etiology: The cause of clostridial infections is bacteria Clostridium species.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to clostridial infections.
-Morphology: The morphology associated with clostridial infections shows gram-positive rods, measuring 3–5 μm in length and 0.5 μm in width. They are encapsulated, motile by peritrichous flagella and sporulating in nature.
-Histology: The histology associated with clostridial infections shows rods, box car shaped, spores with intracellular clearings.
How do Clostridial Infections Present?
Patients with clostridial infections typically are all genders of all ages. The symptoms, features, and clinical findings associated with clostridial infections include dehydration, rapid heart rate, nausea, loss of appetite, diarrhea, and cramping.
How is Clostridial Infections Diagnosed?
Clostridial infections are diagnosed by blood test, and x-rays.
How is Clostridial Infections Treated?
Clostridial infections are treated by antibiotics such as penicillin, and clindamycin.
What is the Prognosis of Clostridial Infections?
The prognosis of clostridial infections is poor.
What are Obligate Intracellular Bacterial Infections?
Obligate intracellular bacterial infections are bacteria that infect human cells.
Examples of obligate intracellular bacterial infections include:
Chlamydia
Rickettsia
What is Chlamydia?
Chlamydia is a common STD that can infect both men and women. It can cause serious, permanent damage to a woman’s reproductive system.
What is the Pathology of Chlamydia?
The pathology of chlamydia is:
-Etiology: The cause of chlamydia is bacteria called Chlamydia trachomatis.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to chlamydia are: exposure to the organism and infectivition which survives within the host cell and innate and acquired immunity activated, and then host genetic susceptibility to infection causes the disease.
-Morphology: The morphology associated with chlamydia shows obligate intracellular bacterium and serovars D-K are tropic for the columnar and transitional epithelial cells of the genital tract
-Histology: The histology associated with chlamydia shows lymphoid germinal centers (follicular cervicitis – sensitive but not specific for chlamydia), plasma cells, reactive epithelial atypia.
How does Chlamydia Present?
Patients with chlamydia typically are all genders of all ages. The symptoms, features, and clinical findings associated with chlamydia include: Discharge from penis and testicular pain in men, Bleeding between periods and after sex in women, Painful urination, Vaginal discharge in women.
How is Chlamydia Diagnosed?
Chlamydia is diagnosed by nucleic acid amplification tests NAATs, swab tests.
How is Chlamydia Treated?
Chlamydia is treated by antibiotics doxycycline, azithromycin.
What is the Prognosis of Chlamydia?
The prognosis of chlamydia is fair. In women, untreated chlamydia can spread into the uterus or fallopian tubes and cause pelvic inflammatory disease.
What is Rickettsia?
Rickettsia are a diverse collection of obligately intracellular Gram-negative bacteria that require other living cells for growth.
What is the Pathology of Rickettsia?
The pathology of rickettsia is:
-Etiology: The cause of rickettsia is an unusual type of bacteria.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to rickettsia are: by the entry of pathogens in the skin, it spreads via the bloodstream to infect the endothelium and sometimes the vascular smooth muscle cells.
-Morphology: The morphology associated with rickettsia shows the typical envelope consists of three major layers: an innermost cytoplasmic membrane, a thin electron dense rigid cell wall and an outer layer.
-Histology: The histology associated with rickettsia shows endothelial damage with necrosis.
How does Rickettsia Present?
Patients with rickettsia typically are all genders of all ages. The symptoms, features, and clinical findings associated with rickettsia include cough, rash, muscle aches, swollen lymph glands, fever, and headache.
How is Rickettsia Diagnosed?
Rickettsia is diagnosed by biopsy.
How is Rickettsia Treated?
Rickettsia is treated by antibiotics doxycycline.
What is the Prognosis of Rickettsia?
The prognosis of rickettsia is fair.
What are Fungal Infections?
Fungal Infections are caused by fungus, when an invasive fungus becomes too much for the immune system.
Fungal Infections include:
Yeast fungal infections
Mold fungal infections
Dimorphic fungal infections
What are Yeast Fungal Infections?
Yeast Fungal Infections are fungal infections caused by a yeast.
Examples of yeast fungal infections include:
Candidiasis fungal infection
Cryptococcosis fungal infection
What is Candidiasis Fungal Infection?
Candidiasis fungal Infection is caused by a yeast, a type of fungus called candida.
What is the Pathology of Candidiasis Fungal Infection?
The pathology of candidiasis fungal infection is:
-Etiology: The cause of candidiasis fungal infection is yeast, a type of fungus called Candida.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to candidiasis fungal infection are: the yeast cells adhere to mucosal tissue followed by hyphal invasion causing extensive damage in the tissues.
-Morphology: The morphology associated with candidiasis fungal infection shows small, oval findings.
-Histology: The histology associated with candidiasis fungal infection shows predominantly spongiotic changes in the epidermis with irregular acanthosis, mild spongiosis and inflammatory changes
How does Candidiasis Fungal Infection Present?
Patients with candidiasis fungal infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with candidiasis fungal infection include digestive iIssues, sinus infections, joint pain, oral thrush, tiredness and fatigue.
How is Candidiasis Fungal Infection Diagnosed?
Candidiasis fungal infection is diagnosed by blood sample, or tissue sample.
How is Candidiasis Fungal Infection Treated?
Candidiasis fungal infection is treated by fluconazole, an antifungal medication.
What is the Prognosis of Candidiasis Fungal Infection?
The prognosis of candidiasis fungal infection is good, uncontrolled infections can lead to life-threatening problems especially in those with weakened immune systems.
What is Cryptococcosis Fungal Infection?
Cryptococcosis fungal Infection is an infection caused by the fungus Cryptococcus neoformans or Cryptococcus gattii.
What is the Pathology of Cryptococcosis Fungal Infection?
The pathology of cryptococcosis fungal infection is:
-Etiology: The cause of cryptococcosis fungal infection is a fungus known as Cryptococcus neoformans.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to cryptococcosis fungal infection are: after inhalation, the yeast spores are deposited into the pulmonary alveoli, where they survive the neutral-to-alkaline pH and physiologic concentrations of carbon dioxide and then are phagocytized by alveolar macrophages but if not they may form cystic cluster
-Morphology: The morphology associated with cryptococcosis fungal infection shows an encapsulated, environmental yeast. Cryptococcus neoformans is a round or oval yeast measuring 4–6 µm in diameter, surrounded by a capsule that can be up to 30 µm thick
-Histology: The histology associated with cryptococcosis fungal infection shows yeast cell proliferation with a histiocytic response.
How does Cryptococcosis Fungal Infection Present?
Patients with cryptococcosis fungal infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with cryptococcosis fungal infection include fatigue, fever, excessive sweating, nausea, blurred or double vision, dry cough, headache, and chest pain.
How is Cryptococcosis Fungal Infection Diagnosed?
Cryptococcosis fungal infection is diagnosed by Chest x-ray, urine collection, and lumbar puncture.
How is Cryptococcosis Fungal Infection Treated?
Cryptococcosis fungal infection is treated by medications amphotericin B, flucytosine, Fluconazole.
What is the Prognosis of Cryptococcosis Fungal Infection?
The prognosis of cryptococcosis fungal infection is fair. The type of treatment and prognosis usually depends on the severity of the infection and the parts of the body that are affected.
What are Mold Fungal Infections?
Mold Fungal Infections are caused by a common mold, a type of fungus that lives indoors and outdoors.
Mold fungal infections include:
Aspergillosis fungal infection
Mucormycosis fungal infection
Zygomycosis
What is Aspergillosis Fungal Infection?
Aspergillosis fungal Infection is an infection caused by a type of mold fungus. The illnesses resulting from aspergillosis infection usually affect the respiratory system.
What is the Pathology of Aspergillosis Fungal Infection?
The pathology of aspergillosis fungal infection is:
-Etiology: The cause of aspergillosis fungal infection is Aspergillus, a common mold.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to aspergillosis fungal infection includes the inhalation of airborne conidia and deposition in the bronchioles or alveolar spaces
-Morphology: The morphology associated with aspergillosis fungal infection shows filamentous fungi, which means that they tend to form filaments. A. niger consists of smooth and colorless conidiophores and spores.
-Histology: The histology associated with aspergillosis fungal infection shows dense acute infiltrate in the dermis and deep soft tissue associated with necrosis and scarring.
How does Aspergillosis Fungal Infection Present?
Patients with aspergillosis fungal infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with aspergillosis fungal infection include skin lesions, shortness of breath, chest pain, joint pain, headaches, fever, and chills.
How is Aspergillosis Fungal Infection Diagnosed?
Aspergillosis fungal infection is diagnosed by biopsy, x-rays, antigen skin tests, tissue culture or blood tests.
How is Aspergillosis Fungal Infection Treated?
Aspergillosis fungal infection is treated by voriconazole, and Amphotericin B.
What is the Prognosis of Aspergillosis Fungal Infection?
The prognosis of aspergillosis fungal infection is poor if pulmonary aspergillosis occurs. Invasive aspergillosis is associated with significant mortality, with a rate of 30-95%.
What is Mucormycosis Fungal Infection?
Mucormycosis fungal Infection is previously called zygomycosis, a serious but rare fungal infection caused by a group of molds called mucormycetes.
What is the Pathology of Mucormycosis Fungal Infection?
The pathology of mucormycosis fungal infection is:
-Etiology: The cause of mucormycosis fungal infection is a group of molds called mucormycetes.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to mucormycosis fungal infection are:
-Morphology: The morphology associated with mucormycosis fungal infection shows large, ribbon-like hyphae with irregular diameter and only occasional septae, hence, their frequent characterization in tissue as aseptate fungi.
-Histology: The histology associated with mucormycosis fungal infection shows broad pauciseptate ribbon-like hyphae with irregular branching at 90° angles.
How does Mucormycosis Fungal Infection Present?
Patients with mucormycosis fungal infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with mucormycosis fungal infection include nasal or sinus congestion, black lesions on the nasal bridge, fever, and headache.
How is Mucormycosis Fungal Infection Diagnosed?
Mucormycosis fungal infection is diagnosed by laboratory tests or tissue samples.
How is Mucormycosis Fungal Infection Treated?
Mucormycosis fungal infection is treated by antifungal medicine amphotericin B, posaconazole, or isavuconazole.
What is the Prognosis of Mucormycosis Fungal Infection?
The prognosis of mucormycosis fungal infection is poor.
What are Dimorphic Fungal Infections?
Dimorphic Fungal Infections are caused by fungal pathogens which can overcome the physiological and cellular defenses of the normal human host by changing their morphological form.
Dimorphic fungal infections include:
Blastomyces fungal infection
Coccidioides fungal infection
Histoplasma fungal infection
What is Blastomyces Fungal Infection?
Blastomyces fungal infection is a rare fungal infection usually acquired by breathing in the spores of the fungi blastomyces dermatitidis or blastomyces gilchristii.
What is the Pathology of Blastomyces Fungal Infection?
The pathology of blastomyces fungal infection is:
-Etiology: The cause of blastomyces fungal infection is inhaling airborne spores from contaminated soil into the lungs.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to blastomyces fungal infection occurs when aerosolized conidia are inhaled, and once in the lungs at body temperature, these conidia transform to the yeast phase. A self-limited infection develops in the majority of persons.
-Morphology: The morphology associated with blastomyces fungal infection shows small raised pus-filled (papulopustular) lesions. They may be violet colored and have very small abscesses around the borders of the lesions.
-Histology: The histology associated with blastomyces fungal infection shows marked pseudoepitheliomatous hyperplasia of epidermis, granulomatous and neutrophilic infiltrate, fungi are within giant cells.
How does Blastomyces Fungal Infection Present?
Patients with blastomyces fungal infection typically are all genders of age range 2 – 93 years. The symptoms, features, and clinical findings associated with blastomyces fungal infection include back pain, chest pain, fatigue, weight loss, poor appetite, shortness of breath, and fever.
How is Blastomyces Fungal Infection Diagnosed?
Blastomyces fungal infection is diagnosed by blood sample, urine sample, chest x-rays or CT scans of your lungs.
How is Blastomyces Fungal Infection Treated?
Blastomyces fungal infection is treated by antifungal medication Itraconazole.
What is the Prognosis of Blastomyces Fungal Infection?
The prognosis of blastomyces fungal infection is fair. Although some may recover completely, the mortality rate is about 30%.
What is Coccidiomyces Fungal Infection?
Coccidioides Fungal Infection is an infection caused by the fungus Coccidioides.
What is the Pathology of Coccidioides Fungal Infection?
The pathology of coccidioides fungal infection is:
-Etiology: The cause of coccidioides fungal infection is inhaling spore-laden dust.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to coccidioides fungal infection are: through inhalation of fungal spores, it leads to primary pulmonary infection and then to hematogenous dissemination to other sites.
-Morphology: The morphology associated with coccidioides fungal infection shows morphological variation in its mycelial and parasitic forms. It exists in the desert soil as a mold. As the cells degenerate, barrel-shaped arthroconidia break off from the hyphae and become airborne.
-Histology: The histology associated with coccidioides fungal infection shows massive pseudoepitheliomatous hyperplasia and granulomatous dermal inflammation.
How does Coccidiomyces Fungal Infection Present?
Patients with coccidioides fungal infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with coccidioides fungal infection include muscle aches or joint pain, rash, headache, night sweats, cough, and fatigue.
How is Coccidiomyces Fungal Infection Diagnosed?
Coccidioides fungal infection is diagnosed by chest x-ray, CT scans, and biopsy.
How is Coccidiomyces Fungal Infection Treated?
Coccidioides fungal infection is treated by antifungal medication such as fluconazole.
What is the Prognosis of Coccidioides Fungal Infection?
The prognosis of coccidioides fungal infection is poor. The chronic form of the infection can cause lung abscesses and scarring in your lungs.
What is Histoplasma Fungal Infection?
Histoplasma fungal infection is an infection caused by breathing in spores of a fungus often found in bird and bat droppings.
What is the Pathology of Histoplasma Fungal Infection?
The pathology of histoplasma fungal infection is:
-Etiology: The cause of histoplasma fungal infection is breathing in spores of a fungus often found in bird and bat droppings.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to histoplasma fungal infection are:
-Morphology: The morphology associated with histoplasma fungal infection shows delicate, septate hyphae, 1 – 2 microns thick, with large rough walled macroconidia 5 – 15 microns.
-Histology: The histology associated with histoplasma fungal infection shows isolated intracellular organisms and large aggregates surrounded by chronic inflammatory cells and fibroblasts.
How does Histoplasma Fungal Infection Present?
Patients with histoplasma fungal infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with histoplasma fungal infection include chest pain, body aches, fever, chils, and headaches.
How is Histoplasma Fungal Infection Diagnosed?
Histoplasma fungal infection is diagnosed by blood test or a urine test.
How is Histoplasma Fungal Infection Treated?
Histoplasma fungal infection is treated by antibiotics such as Itraconazole.
What is the Prognosis of Histoplasma Fungal Infection?
The prognosis of histoplasma fungal infection is fair to poor. If untreated, subacute progressive disseminated histoplasmosis results in death within 2-24 months.
What are Parasitic Infections?
Parasitic Infections are caused by organisms that live in or on another organism as host, they spread infections which can lead to sepsis.
Examples of parasitic infections include:
Protozoal parasitic infections
Metazoal parasitic infections
What are Protozoal Parasitic Infections?
Protozoal parasitic infections are characterized by hyperproliferation of the infectious agent living intracellularly or extracellularly of their respective host cells.
Examples of protozoan parasitic Infections include:
African trypanosomiasis infection
Babesiosis infection
Chagas disease infection
Leishmaniasis infection
Malaria infection
What is African Trypanosomiasis Infection?
African trypanosomiasis Infection is an infection with protozoa of the species Trypanosoma brucei, transmitted by the bite of a tsetse fly.
What is the Pathology of African Trypanosomiasis Infection?
The pathology of african trypanosomiasis infection is:
-Etiology: The cause of african trypanosomiasis infection is microscopic parasites of the species Trypanosoma brucei.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to african trypanosomiasis infection are infected tsetse inoculate metacyclic trypanosomes into the skin of animals, where the trypanosomes reside for a few days and cause localized inflammation chancres. They enter the lymph and lymph nodes, then the bloodstream, where they divide rapidly by binary fission and cause tissue damage.
-Morphology: The morphology associated with african trypanosomiasis infection shows a single flagellum and a compact disc of mitochondrial DNA termed the kinetoplast.
-Histology: The histology associated with african trypanosomiasis infection shows ganglionitis with neuronal cell depopulation, fibrosis and mast cell infiltrates are also present.
How does African Trypanosomiasis Infection Present?
Patients with disease in lower case typically are all genders of all ages. The symptoms, features, and clinical findings associated with african trypanosomiasis infection include fatigue, swollen lymph nodes, aching muscles, severe headaches, irritability, and fever.
How is African Trypanosomiasis Infection Diagnosed?
African trypanosomiasis infection is diagnosed by blood sample, bone marrow aspirate, and cerebrospinal fluid.
How is African Trypanosomiasis Infection Treated?
African trypanosomiasis infection is treated by medications suramin, pentamidine, melarsoprol, or eflornithine
What is the Prognosis of African Trypanosomiasis Infection?
The prognosis of african trypanosomiasis infection is fair to poor. It may be fatal if not treated.
What is Babesiosis Infection?
Babesiosis Infection is a disease caused by microscopic parasites that infect red blood cells.
What is the Pathology of Babesiosis Infection?
The pathology of babesiosis infection is:
-Etiology: The cause of babesiosis infection is microscopic parasites that infect red blood cells. -Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to babesiosis infection caused by protozoa of the genus Babesia and is transmitted primarily by tick vectors. Transmission rarely occurs through blood transfusion, organ transplantation, or congenitally.
-Morphology: The morphology associated with babesiosis infection shows intraerythrocytic stages appear singly as small round, ovoid or elongate trophozoites (2-4µm), in pairs.
-Histology: The histology associated with babesiosis infection shows multiple small forms within a single cell that are not a clear schizont form of Plasmodium, easily identified extracellular forms, and lack of malaria pigment.
How does Babesiosis Infection Present?
Patients with babesiosis infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with babesiosis infection include body aches, loss of appetite, nausea, or fatigue, fever, chills, sweats, headache.
How is Babesiosis Infection Diagnosed?
Babesiosis infection is diagnosed by blood tests and microscopic examination of blood smears.
How is Babesiosis Infection Treated?
Babesiosis infection is treated by medications such as Atovaquone, azithromycin, Clindamycin PLUS quinine.
What is the Prognosis of Babesiosis Infection?
The prognosis of babesiosis infection is excellent and most patients recover spontaneously.
What is Chagas Disease Infection?
Chagas disease infection, also known as American trypanosomiasis, is a tropical parasitic disease caused by Trypanosoma cruzi.
What is the Pathology of Chagas Disease Infection?
The pathology of chagas disease infection is:
-Etiology: The cause of chagas disease infection is a parasite Trypanosoma cruzi.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to chagas disease infection occurs when a kissing bug bites an infected person or animal, then bites another person. While biting, infected bugs deposit feces containing metacyclic trypomastigotes on the skin.
-Morphology: The morphology associated with chagas disease infection shows three morphological forms: the trypomastigote, the epimastigote, and the amastigote. Trypanosomes are present in the circulating blood. They are approximately 20 mm long and generally slender. They have a thin, irregularly shaped membrane, which can be seen using scanning electron microscopy.
-Histology: The histology associated with chagas disease infection shows mononuclear cell infiltration, edema, myocyte destruction, and fibrosis.
How does Chagas Disease Infection Present?
Patients with chagas disease infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with chagas disease infection include eyelid swelling, headache, rash, loss of appetite, body aches, and swelling at the infection site.
How is Chagas Disease Infection Diagnosed?
Chagas disease infection is diagnosed by blood tests.
How is Chagas Disease Infection Treated?
Chagas disease infection is treated by medications such as benznidazole, or nifurtimox.
What is the Prognosis of Chagas Disease Infection?
The prognosis of chagas disease infection is good.
What is Leishmaniasis Infection?
Leishmaniasis Infection is a parasitic disease caused by infection with Leishmania parasites, which are spread by the bite of phlebotomine sand flies.
What is the Pathology of Leishmaniasis Infection?
The pathology of leishmaniasis infection is:
-Etiology: The cause of leishmaniasis infection is Leishmania parasites.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to leishmaniasis infection are: After inoculation by sandflies, the flagellated promastigotes bind to macrophages in the skin, activate complement system, the parasitized macrophages disseminate infection to all parts of the body but more so to the spleen, liver, and bone marrow.
-Morphology: The morphology associated with leishmaniasis infection shows a structure similar to a volcano, with a raised edge and central crater. Some sores are covered by a scab.
-Histology: The histology associated with leishmaniasis infection shows dermal granulomatous inflammation with predominant lymphocytes, histiocytes contain small oval organisms with bar shaped paranuclear kinetoplast.
How does Leishmaniasis Infection Present?
Patients with leishmaniasis infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with leishmaniasis infection include decreased production of blood cells, bleeding, enlarged spleen, enlarged liver, weight loss, and fever.
How is Leishmaniasis Infection Diagnosed?
Leishmaniasis infection is diagnosed by tissue specimens from skin lesions, and bone marrow.
How is Leishmaniasis Infection Treated?
Leishmaniasis infection is treated by medications intravenous liposomal amphotericin B.
What is the Prognosis of Leishmaniasis Infection?
The prognosis of leishmaniasis infection is fair. It spontaneously resolves in 3-6 months without therapy, although some infections persist indefinitely.
What is Malaria Infection?
Malaria Infection is a serious and sometimes fatal disease caused by a parasite that commonly infects a certain type of mosquito which feeds on humans.
What is the Pathology of Malaria Infection?
The pathology of malaria infection is:
-Etiology: The cause of malaria infection is a single-celled parasite of plasmodium genus.
-Genes involved: Not applicable.
Pathogenesis: The sequence of events that lead to malaria infection spreads exclusively by female anopheline mosquitoes.
-Morphology: The morphology associated with malaria infection shows four developmental stages in humans.
-Histology: The histology associated with malaria infection shows rings of P. falciparum can be found in blood smears, some may exhibit Maurer clefts, gametocytes may be present in blood smears.
How does Malaria Infection Present?
Patients with malaria infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with malaria infection include nausea, vomiting, diarrhea, fever, flu, tiredness, anemia, and jaundice.
How is Malaria Infection Diagnosed?
Malaria infection is diagnosed by blood tests.
How is Malaria Infection Treated?
Malaria infection is treated by medications such as Atovaquone-proguanil, Quinine sulfate, and doxycycline.
What is the Prognosis of Malaria Infection?
The prognosis of malaria infection is poor. Most patients with uncomplicated malaria exhibit marked improvement within 48 hours after the initiation of treatment and are fever free after 96 hours.
What are Metazoal Parasitic Infections?
Metazoal Parasitic Infections are caused by parasitic flatworms, tapeworms, trematodes, roundworms, acanthocephalans, crustaceans.
Metazoal parasitic infections include:
Lymphatic filariasis infection
Onchocerciasis infection
Schistosomiasis infection
Strongyloides infection
Trichinosis infection
Tapeworms infection
What is Lymphatic Filariasis Infection?
Lymphatic filariasis infection is a neglected tropical disease NTD, is a parasitic disease caused by microscopic, thread-like worms.
What is the Pathology of Lymphatic Filariasis Infection?
The pathology of lymphatic filariasis infection is:
-Etiology: The cause of lymphatic filariasis infection are parasites.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to lymphatic filariasis infection includes bite from an infected mosquito introduces third stage infective filarial larvae onto the human skin, they penetrate into the bite wound to reach the lymphatics where they reside and develop into adults.
-Morphology: The morphology associated with lymphatic filariasis infection shows microfilariae, or larval stage of W. bancrofti, are sheathed, and range from approximately 245 to 300 µm.
-Histology: The histology associated with lymphatic filariasis infection shows microfilariae are the diagnostic form, intact adult filariae in lymph nodes are pathognomonic; may see dead filariae with surrounding granulomatous inflammation and calcifications.
How does Lymphatic Filariasis Infection Present?
Patients with lymphatic filariasis infection typically are all genders but males are at greater risk at age ranges from 9 to 16 years. The symptoms, features, and clinical findings associated with lymphatic filariasis infection include pain in the limbs, swollen lymph nodes, and fever.
How is Lymphatic Filariasis Infection Diagnosed?
Lymphatic filariasis infection is diagnosed by blood tests.
How is Lymphatic Filariasis Infection Treated?
Lymphatic filariasis infection is treated by medications Diethylcarbamazine citrate.
What is the Prognosis of Lymphatic Filariasis Infection?
The prognosis of lymphatic filariasis infection is good if infection is recognized and treated early.
What is Onchocerciasis Infection?
Onchocerciasis Infection is an infection caused by the parasitic worm Onchocerca volvulus, spread by the bite of an infected Simulium blackfly.
What is the Pathology of Onchocerciasis Infection?
The pathology of onchocerciasis infection is:
-Etiology: The cause of onchocerciasis infection is parasitic worm Onchocerca volvulus.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to onchocerciasis infection involves many blackfly bites are needed before disease develops. Infective larvae inoculated into the skin during the bite of a blackfly develop into adult worms in 12 to 18 months. Adult female worms may live up to 15 years in subcutaneous nodules.
-Morphology: The morphology associated with onchocerciasis infection is unsheathed and measures 300-315 µm in length. The tail tapers to a point and is often sharply bent. The nuclei do not extend to the tip of the tail.
-Histology: The histology associated with onchocerciasis infection shows microfilariae concentrate in the papillary dermis with clusters of inflammatory cells surrounding vessels and adnexa.
How does Onchocerciasis Infection Present?
Patients with onchocerciasis infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with onchocerciasis infection include disfiguring skin conditions, visual impairment, and itching.
How is Onchocerciasis Infection Diagnosed?
Onchocerciasis infection is diagnosed by skin biopsy.
How is Onchocerciasis Infection Treated?
Onchocerciasis infection is treated by medications ivermectin.
What is the Prognosis of Onchocerciasis Infection?
The prognosis of onchocerciasis infection is poor.
What is Schistosomiasis Infection?
Schistosomiasis Infection also known as bilharzia, is a disease caused by parasitic worms.
What is the Pathology of Schistosomiasis Infection?
The pathology of schistosomiasis infection is:
-Etiology: The cause of schistosomiasis infection is parasitic worms.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to schistosomiasis infection includes immunologic reactions to Schistosoma eggs trapped in tissues. Antigens released from the egg stimulate a granulomatous reaction involving T cells, macrophages, and eosinophils that results in clinical disease.
-Morphology: The morphology associated with schistosomiasis infection is large, tapered and slightly curved. When the eggs are excreted in stool, they contain a mature miracidium.
-Histology: The histology associated with schistosomiasis infection shows focal ulcers, eggs may be calcified, surrounded by fibrosis or granuloma
How does Schistosomiasis Infection Present?
Patients with schistosomiasis infection are typically higher in males and children with an age range of 12–15 years. The symptoms, features, and clinical findings associated with schistosomiasis infection include: fever, chills, cough, muscle aches.
How is Schistosomiasis Infection Diagnosed?
Schistosomiasis infection is diagnosed by urine test, and blood test.
How is Schistosomiasis Infection Treated?
Schistosomiasis infection is treated by medications such as praziquantel.
What is the Prognosis of Schistosomiasis Infection?
The prognosis of schistosomiasis infection is good.
What is Strongyloides Infection?
Strongyloides Infection is a human pathogenic parasitic roundworm causing the disease strongyloidiasis.
What is the Pathology of Strongyloides Infection?
The pathology of strongyloides infection is:
-Etiology: The cause of strongyloides infection is a parasite.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to strongyloides infection includes strongyloides filariform larvae in fecally contaminated ground that penetrate skin, enter the systemic circulation and migrate to the lungs where they induce inflammation.
-Morphology: The morphology associated with strongyloides infection shows female filariform larvae (males are thought to be non-parasitic) are slender and fast-moving, being approximately 50 µm in diameter and between 350-600 µm in length.
-Histology: The histology associated with strongyloides infection shows tissue eosinophilia and granulocytic infiltration that may cause abscess formation are present.
How does Strongyloides Infection Present?
Patients with strongyloides infection typically are all genders of all ages. The symptoms, features, and clinical findings associated with strongyloides infection include heartburn, diarrhea, constipation, a dry cough, skin rashes, abdominal pain, bloating.
How is Strongyloides Infection Diagnosed?
Strongyloides infection is diagnosed by blood test.
How is Strongyloides Infection Treated?
Strongyloides infection is treated by antiparasitic medication ivermectin, and albendazole.
What is the Prognosis of Strongyloides Infection?
The prognosis of strongyloides infection is good. However, in people with weak immune systems, it can be life-threatening.
What is Trichinosis Infection?
Trichinosis Infection is a food-borne disease caused by a microscopic parasite called Trichinella.
What is the Pathology of Trichinosis Infection?
The pathology of trichinosis infection is:
-Etiology: The cause of trichinosis infection is the larvae of the Trichinella roundworm.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to trichinosis infection are: the infection due to eating raw, undercooked, or under-processed meat from infected animals, most commonly pigs, wild boar, or bear. Larvae cysts enter the small bowel, then penetrate the mucosa, and then become adults in 6 to 8 days causing infection.
-Morphology: The morphology associated with trichinosis infection shows measurements between 1.4 and 1.6 mm long, and are more flat anteriorly than posteriorly. The anus can be found in the terminal end, and they have a large copulatory pseudobursa on each side.
-Histology: The histology associated with trichinosis infection shows mucosa in the vicinity of embedded worms is edematous and friable with increased histiocytes within the lamina propria.
How does Trichinosis Infection Present?
Patients with trichinosis infection typically in all genders and at all ages, but mostly at 20-49 years age. The symptoms, features, and clinical findings associated with trichinosis infection include: diarrhea, nausea, fatigue, stomach pain, fever, headaches, chills, muscle soreness, pain and swelling around the eyes.
How is Trichinosis Infection Diagnosed?
Trichinosis infection is diagnosed by blood samples tests for white blood cells level, muscles biopsy, and ELISA test.
How is Trichinosis Infection Treated?
Trichinosis infection is treated by antiparasitic medicines: albendazole, mebendazole.
What is the Prognosis of Trichinosis Infection?
The prognosis of trichinosis infection is good. Trichinosis usually isn’t serious and often gets better on its own, usually within a few months.
What are Tapeworms Infections?
Tapeworm infections are caused by ingesting food or water contaminated with tapeworm eggs or larvae.
Tapeworms Infections include:
Cysticercosis
Hydatid Disease
What is Cysticercosis?
Cysticercosis is a parasitic tissue infection caused by larval cysts of the tapeworm Taenia solium. These larval cysts infect brain, muscle, or other tissue, and are a major cause of adult onset seizures in most low-income countries.
What is the Pathology of Cysticercosis?
The pathology of cysticercosis is:
-Etiology: The cause of cysticercosis is larvae of the parasite Taenia solium
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to cysticercosis are: after the ingestion of embryonated Taenia solium eggs, oncospheres hatch from the eggs, penetrate the intestinal wall into the circulation then penetrate the tissues of several organs neural or extra neural cells to form cysticerci in them.
-Morphology: The morphology associated with cysticercosis shows fluid-filled cystic structures consisting of a thin bladder wall and parenchymatous portion containing a single invaginated scolex surrounded by a convoluted spiral canal. The hooks of the armed scolex may be visible in tissue sections.
-Histology: The histology associated with cysticercosis shows the cystic cavity contains the larval form: scolex with hooklets and two pairs of suckers.
How does Cysticercosis Present?
Patients with cysticercosis typically in children and young females aged 10-40 years. The symptoms, features, and clinical findings associated with cysticercosis include headaches, seizures, nausea, and vomiting.
How is Cysticercosis Diagnosed?
Cysticercosis is diagnosed by MRI, CT scans of the brain, blood tests to diagnose infection.
How is Cysticercosis Treated?
Cysticercosis is treated by antiparasitic therapy, corticosteroids, antiepileptic drugs, or surgery.
What is the Prognosis of Cysticercosis?
The prognosis of cysticercosis is good generally, however, it is mostly affected by the number of lesions and extent of inflammation. Individuals with one brain lesion have a very good chance of survival with no seizure relapses.
What is Hydatid Disease?
Hydatid disease is a form of echinococcosis caused by the development of hydatids of a tapeworm of the genus Echinococcus.
What is the Pathology of Hydatid Disease?
The pathology of hydatid disease is:
-Etiology: The cause of hydatid disease is the larval stage of Echinococcus granulosus.
-Genes involved: Not applicable.
-Pathogenesis: The sequence of events that lead to hydatid disease are: The egg larvae invade the bowel wall and mesenteric vessels of the host, and then circulation to the liver. In the liver, the larvae grow and become encysted. The hydatid cyst develops an outer layer of inflammatory tissue and an inner germinal membrane that produces daughter cysts.
-Morphology: The morphology associated with hydatid disease shows three different developmental stages: eggs; larvae; and adults.
-Histology: The histology associated with hydatid disease shows granulomatous palisading reaction and pseudocyst formation as seen in cutaneous lesions.
How does Hydatid Disease Present?
Patients with hydatid disease typically are all genders at all ages. The symptoms, features, and clinical findings associated with hydatid disease include blood or the fluid from a ruptured cyst, cough, weakness, weight loss, diarrhea, stomach upset, abdominal pain, and anemia.
How is Hydatid Disease Diagnosed?
Hydatid disease is diagnosed by ultrasound, CT-scan, MRI, ELISA or immunoblotting.
How is Hydatid Disease Treated?
Hydatid disease is treated by percutaneous treatment of the hydatid cysts with the PAIR technique, surgery, and albendazole therapy.
What is the Prognosis of Hydatid Disease?
The prognosis of hydatid disease is good. It is a potentially serious but treatable infection that may be fatal in a small number of cases.