Others syndromes that have malignancies that affect the central nervous system include:
- Cowden syndrome
- Gorlin syndrome
- Li-Fraumeni syndrome
- Turcot syndrome
What is Cowden Syndrome?
Cowden syndrome is a genetic disorder characterized by multiple noncancerous, tumor-like growths called hamartomas and an increased risk of developing certain cancers. Almost everyone with Cowden syndrome develops hamartomas.
What is the Cowden Syndrome?
Etiology: The cause of Cowden syndrome mutations in a gene known as PTEN.
Genes involved: PTEN.
Pathogenesis: PTEN acts as a tumor suppressor gene through the action of it’s phosphatase protein product. This phosphatase is involved in the regulation of the cell cycle, preventing cells from growing and dividing too rapidly. It is a target of many anticancer drugs.
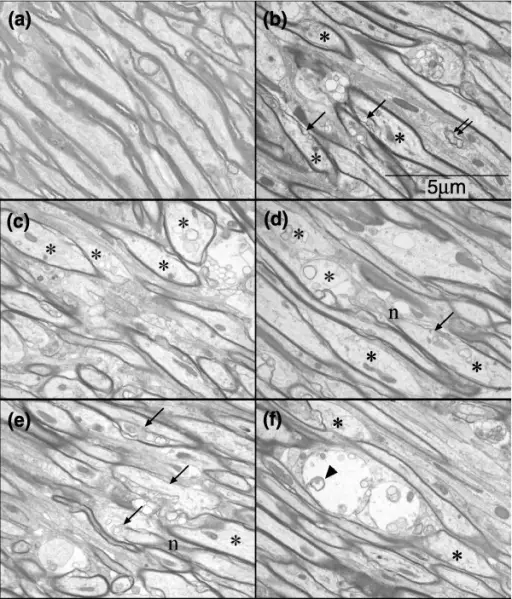
Histology: The histology associated with Cowden syndrome shows glycogenic acanthosis, ganglioneuroma, and hamartomatous polyp.
How does Cowden Syndrome Present?
Patients with Cowden syndrome are typically more females than males, and symptoms appear by the age of 20 years old. The symptoms, features, and clinical findings associated with Cowden syndrome include macrocephaly, intellectual disability, and skin lesions.
How is Cowden Syndrome Diagnosed?
Cowden syndrome is diagnosed by a diagnostic criteria.
Major criteria:
- Breast cancer
- Endometrial cancer
- Thyroid carcinoma
- Gastrointestinal hamartomas excluding hyperplastic polyps >3
- Lhermitte-Duclos disease
- Macrocephaly (58cm females, 60cm males)
- Macular pigmentation of the glans penis
- Multiple mucocutaneous lesions
- Multiple trichilemmomas >3
- Acral keratosis >3
- Mucocutaneous neuromas >3
- Oral papillomas, multiple >3, OR biopsy proven, or dermatologist diagnosed
Minor criteria:
- Autism spectrum disorder
- Colon cancer
- Esophegal glycogenic acanthosis
- Lipomas >3
- Mental retardation <75 IQ
- Renal cell carcinoma
- Testicular lipomatosis
- Thyroid cancer
- Thyroid structural lesions
- Vascular anomalies
- CT and MRI can also be used for diagnosis
How is Cowden Syndrome Treated?
Cowden syndrome is treated in the same fashion as those that occur sporadically in patients without a hereditary cancer syndrome. The benign mucocutaneous lesions observed in Cowden syndrome are typically not treated unless they become symptomatic or disfiguring. Numerous treatment options include topical agents, cryosurgery, curettage, laser ablation, and excision, may be utilized.
What is the Prognosis of Cowden Syndrome?
The prognosis of Cowden syndrome is poor and there is no cure.