Seminomas are malignancies accounting for around a 1/3 of all germ cell tumors.
What is the Pathology of Seminomas?
The pathology of seminomas is:
-Etiology: The cause of seminomas is not well identified, but seems to be associated with cryptorchidism.
-Genes involved: KIT
-Pathogenesis: The sequence of events that lead to seminomas originates from the germinal epithelium. Trapped gonocyte maturation results in the propagation of undeveloped spermatogonia. This causes increased genomic volatility.
-Morphology: The morphology associated with seminomas shows testis enlarged with normal contour, smaller tumor looks like circumscribed mass in the testis.
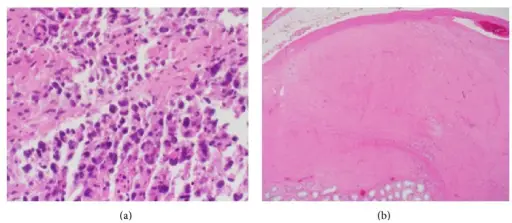
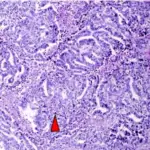
-Histology: The histology associated with seminomas shows tumor cells fairly even in size with clear cytoplasm and well-defined cell borders.
How does Seminomas Present?
Patients with seminomas typically affect middle-aged men between 30 to 50 years old. The symptoms, features, and clinical findings associated with seminomas include enlarged painless testis. Upsurge in hCG levels, and gynecomastia.
How are Seminomas Diagnosed?
Seminomas are diagnosed through laboratory studies such as AFP, B-HCG, and LDH. Imaging studies such as testicular ultrasonography, abdominal and pelvis CT scans may be useful. Biopsy is confirmatory.
How are Seminomas Treated?
Seminomas are treated through radical orchiectomy, radiation therapy, and chemotherapy.
What is the Prognosis of Seminomas?
The prognosis of seminomas is good with a survival rate >95% if diagnosed early while still confined in the testis.