Splenic infarcts are common lesions caused by the occlusion of the major splenic artery or any of its branches. Splenic infarction may be the result of arterial or venous occlusion usually caused by bland or septic emboli as well as venous congestion by abnormal cells.
What is the Pathology of Splenic Infarcts?
The pathology of splenic infarcts is:
-Etiology: The causes of splenic infarcts are may include bloodborne malignancy (lymphoma, leukemia), myelofibrosis, infections, trauma, or clotting issues.
-Genes involved: HBB (hemoglobin subunit beta).
-Pathogenesis: The sequence of events that lead to splenic infarcts are due to an abnormality of splenic circulation.
How does Splenic Infarcts Present?
Patients with splenic infarcts typically affect both genders. Present at an age range of 40-years-old. Splenic infarcts are typically due to thromboembolic ailments. The symptoms, features, and clinical findings associated with splenic infarcts include left-upper-quadrant abdominal pain. Additional symptoms of splenic infarcts include nausea and vomiting, fever and chills, pleuritic chest ache, and left shoulder agony.
How is Splenic Infarcts Diagnosed?
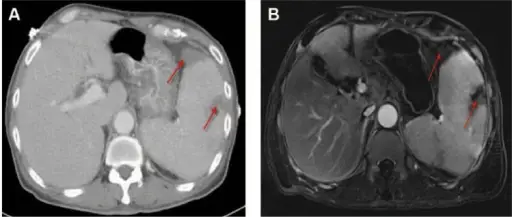
Splenic Infarcts is diagnosed through: Computed tomography (CT), performed with intravenous (IV) nonionic contrast. Magnetic resonance imaging (MRI), made with IV gadolinium contrast to identify infarcted splenic parenchyma. Other diagnosis modes include radioisotope scans and ultrasonographic evaluation of the spleen.
How is Splenic Infarcts Treated?
Splenic Infarcts is treated through analgesia, nonsteroidal anti-inflammatory drugs (NSAIDs), and close follow-up. An isolated splenic abscess can be treated with percutaneous drainage, and splenectomy avoided. Surgical intervention may be indicated in certain cases such as sepsis, hemorrhage, abscess, or tenacious pseudocyst formation.
What is the Prognosis of Splenic Infarcts?
The prognosis of splenic infarcts varies according to the primary disease accountable for the infarct. Massively enlarged spleens splenectomies, associated hematologic malignancies, are allied with mortalities of as high as above 35%. At the other end, many infarcts are clinically mysterious, with no significant long-term sequelae.