Transplant rejection is a process in which the transplanted tissue or organ is rejected by the immune system in the recipient.
What is the Mechanism of Allograft Rejection?
The recipient’s immune system recognizes two types of antigens on the transplant: Major histocompatibility complex (MHC) antigens also known as human leukocyte antigens (HLA) and Minor histocompatibility antigens.
What is Allorecognition of MHC Antigens?
The immune system of the host identifies its own cells and differentiated them from the foreign antigens present on the cellular surface of the transplant. There are two pathways of allorecognition: Direct allorecognition and indirect allorecognition.
The direct pathway of allorecognition involves intact allo-MHC molecules expressed on the transplant cells that are recognized by T cells. The direct allo-recogntion response is rapid and results in acute cellular rejection.
The indirect pathway of allorecogntion, involves allo-MHC molecules that are not intact that are shed from the donor cell surface. These are taken up by antigen-presenting cells (APC) and are presented to T cells. The activated T cells take up further signaling by secreting the cytokines. The indirect allorecognition is slower and results in chronic rejection.
What are T Cell-mediated reactions in Transplant Rejection?
When an organ is transplanted into another body, it experiences some immunological response in the host which is initiated by the T cells of the host immune system. This is a T cell-mediated reaction involved in this process and it can be acute or chronic.
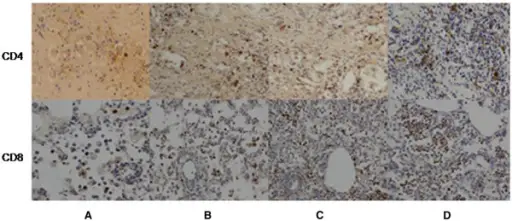
In acute cellular rejection, the T cells recognize the graft MHC molecules early. The CD4 receptors present on the T cells recognize the MHC class II molecules and CD8 receptors from T cells bind with the MHC class I molecules. This binding activates the T cells which releases the inflammatory cytokines which cause the attraction and accumulation of the phagocytic cells into the organ.
The chronic cellular rejection is carried out by the indirect pathway of allorecognition. In this pathway, the MHC molecules are not intact and these are shed off from the cellular surface of the transplant. Antigen-presenting cells identify and take up these molecules and then present these to T cells. The activated T cells then initiate the inflammatory response which ultimately leads to the accumulation of the phagocytes into the target organ.
What are the Antibody-Mediated Rejections in Transplant Rejections?
These are considered the major cause the graft rejection. This includes hyperacute, acute, and chronic antibody-mediated rejection.
What is Hyperacute Rejection?
The hyperacute rejection can occur in minutes of the transplant due to the presence of donor-specific antibodies. This is a very rare phenomenon and usually occurs in a patient with a history of transplantation. The CD4 T-cells react with HLA-class II molecules expressed by the cells of the transplant which initiates the immune response in the recipient and causes rejection of the organ within a few minutes of the transplant.
What are Acute Antibody-Mediated Rejections?
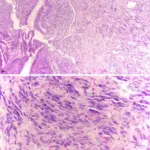
This is the dysfunction or the rejection of the graft within days after the transplant. This is the result of donor-specific antibodies. Histopathology reveals the endothelial injury mediated by the antibodies. It is less severe than hyperacute antibody-mediated rejections.
What are the Chronic Antibody-Mediated Rejections?
This is mediated by the antibodies and occurs after days of the transplant. In this rejection, immunoglobulin G antibodies are produced by the activation of the B cells against the transplanted organ or tissue.
What is the Method to Increase Organ Transplant Life?
The organ transplants are mostly done in the life threatening condition but rejections of the transplanted organs in the recipient body are one of the major problem. There are several methods that can help to increase the post-transplant life of the transplanted organ.
HLA markers matching is done between the donor and recipient in the transplant. This helps the development of new blood cells reducing the complications like graft-versus-host disease.
The chances of post-transplant rejection can also be minimized if the transplant is done between identical twins. In this way, there will be very little chance of rejection. But it is not possible to have identical twins in every case, so it is much easier to have the transplanted organ or tissue from close family members.
Apart from the pre-transplant selection & testing, transplant life can be increased by using immune-suppressive therapies. Various immunosuppressive agents are used for life along with some antifungals to protect the fungal growth due to suppressed immune system.
What are Stem Cell Transplants?
Stem cell transplant also called one marrow transplant, is the procedure involving the replacement of damaged stem cells in the patient with healthy stem cells. The new stem cells can be taken from the patient’s own healthy stem cells or from a healthy donor. The use of hematopoietic stem cells is very common in which stem cells are introduced into the bloodstream of the patient after conditioning the patient. A potential risk of hematopoietic stem cells is graft versus host disease.
What is the Graft Versus Host Disease?
This is an immune response in which the transplanted tissue or organ reacts to the host body and rejects it instead of being rejected by the host. The T cell of the transplant identifies and recognizes the host antigens as foreign and start an inflammatory cascade. This results in the attack on the host tissues by the graft. There are two types of the Graft Versus Host Disease which are acute and chronic.
If the reaction occurs within 100 days, it is the acute graft versus host disease. The conditioning of the patient causes the release of inflammatory cytokines which results in the expression of MHC antigens. The donor T cells recognize the host cells as antigens. The activated T cells release the inflammatory cytokines which stimulate the production of inflammatory chemokines, thus recruiting phagocytes into the target cells. If the reaction occurs after 100 days, it is chronic graft versus host disease. The T cells are involved in this disease.