Urothelial Carcinomas are cancers that begin in cells called urothelial cells that line the urethra, bladder, ureters, renal pelvis, and some other organs. Urothelial cells are also called transitional cells. These cells can change shape and stretch without breaking apart. Also called transitional cell cancer.
What is the Pathology of Urothelial Carcinomas?
The pathology of urothelial carcinomas is:
-Etiology: The cause of urothelial carcinomas is smoking, schistosomiasis infection, and occupational exposure to certain chemicals.
-Genes involved: FGFR3, TP53, PIK3CA, KDM6A, ARID1A, KMT2D, HRAS, TERT, KRAS, CREBBP, RB1 and TSC1.
-Pathogenesis: The sequence of events that lead to urothelial carcinomas develops via two distinct pathways, the first relates to papillary lesions, and the second relates to flat lesions.
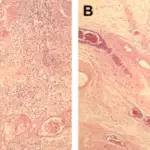
-Morphology: The morphology associated with urothelial carcinomas shows a polypoid, sessile, fungating ulcerated and/or infiltrative lesion.
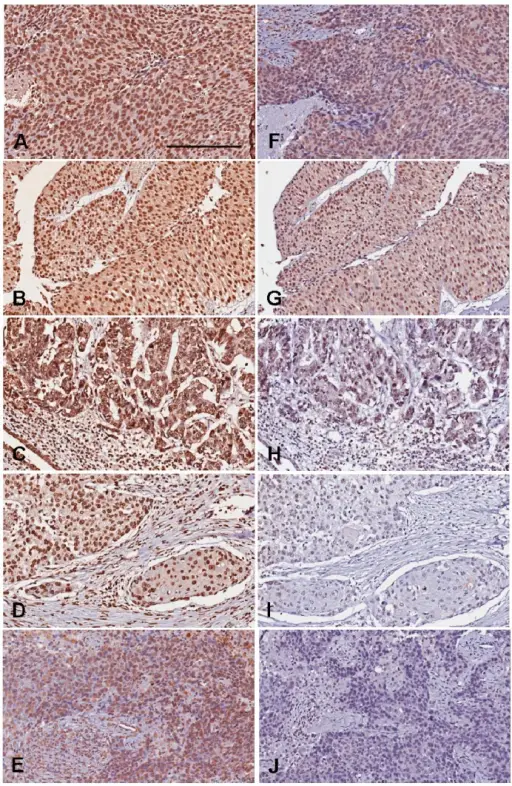
-Histology: The histology associated with urothelial carcinomas shows neoplastic cells invade the bladder wall as nests, cords, trabeculae, small clusters, or single cells that are usually separated by desmoplastic stroma.
How does Urothelial Carcinomas Present?
Patients with urothelial carcinomas typically affect males four times more than females in their adulthood. The symptoms, features, and clinical findings associated with urothelial carcinomas include bladder cancer characteristically causing blood in the urine. Blood in the urine is the most common symptom of bladder cancer and is painless. Other possible symptoms include pain during urination, frequent urination, or feeling the need to urinate without being able to do so. People with advanced disease may have pelvic or bony pain, lower-extremity swelling, or flank pain. Rarely, a palpable mass can be detected on physical examination.
How is Urothelial Carcinomas Diagnosed?
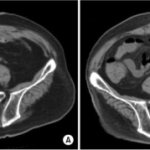
Diagnostic modalities used in diagnosing BC include Imaging (ultrasound, intravenous urography (IVU), computed tomography (CT), magnetic resonance imaging (MRI)), cystoscopy, and biopsy.
How is Urothelial Carcinomas Treated?
The treatment of bladder cancer is typically surgery.
What is the Prognosis of Urothelial Carcinomas?
The prognosis of urothelial carcinomas is good. The 5-year overall survival (OS) for pT1 is 75%, for pT2 is 50%, and for pT3 is 20%.