Acute pancreatitis is a group of reversible lesions characterized by inflammation of the pancreas with severity ranging from edema, fat necrosis to parenchymal necrosis with severe hemorrhage.
What is the Pathology of Acute Pancreatitis?
The pathology of acute pancreatitis is:
-Etiology: The cause of acute pancreatitis is biliary tract disease, drugs, trauma, alcoholism, infectious, and post-ERCP.
-Genes involved: Cationic Trypsinogen (PRSS1), CFTR gene.
-Pathogenesis: The sequence of events that lead to acute pancreatitis; injures the acinar cell and impairs the secretion of zymogen granules, believed that both extracellular factors and intracellular factors play a role. Also results from ductal cell injury which leads to the absence or delayed enzymatic secretion. Acute pancreatitis is an inflammatory process by which there is autodigest gland by pancreatic enzymes. The gland may restore without any loss of function or any morphologic variations.
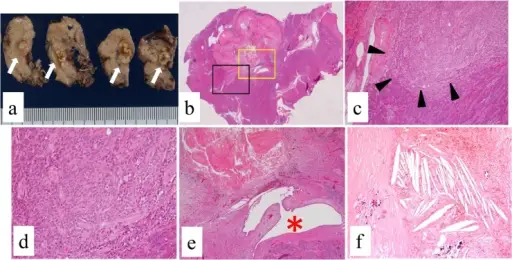
-Morphology: The morphology associated with acute pancreatitis shows interstitial edema.
-Histology: The histology associated with acute pancreatitis shows inflammatory infiltrate hemorrhage and necrosis.
How does Acute Pancreatitis Present?
Patients with acute pancreatitis are typically more common in males present at an age range of 35-75 years. The symptoms, features, and clinical findings associated with acute pancreatitis include abdominal pain, nausea, and vomitting.
How is Acute Pancreatitis Diagnosed?
Acute pancreatitis is diagnosed through laboratory studies- raised serum amylase and lipase levels, BUN, creatinine, serum electrolytes, cholesterol, glucose, and triglycerides. A 48 hour C-reactive protein (CRP) value. Radiological studies- abdominal ultrasonography, endoscopic ultrasonography, abdominal CT scan, magnetic resonance cholangiopancreatography (MRCP), and endoscopic retrograde cholangiopancreatography (ERCP).
How is Acute Pancreatitis Treated?
Acute pancreatitis is treated through medical care, antibiotic therapy, fluid resuscitation. Surgical intervention and nutritional support may be needed.
What is the Prognosis of Acute Pancreatitis?
The prognosis of acute pancreatitis is fair with an overall mortality of 15%.