Allergic rhinitis is the inflammation of the nasal passages mucosal precipitated by sensitivity responses to one of a hefty cluster of allergens characterized by obvious redness, mucosal edema, and mucus discharge, convoyed by a leukocytic infiltration.
What is the Pathology of Allergic Rhinitis?
The pathology of allergic rhinitis is:
-Etiology: The cause of allergic rhinitis is caused by an immunoglobulin E–mediated reaction due to several allergens to nasal mucosa.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to allergic rhinitis is due to sensitization to allergic causing factors.
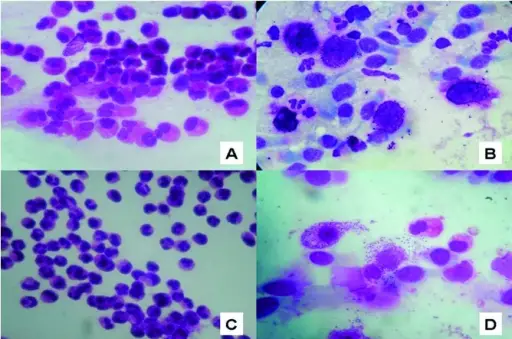
-Histology: The histology associated with allergic rhinitis shows eosinophils, basophils, mast cells, and T cells.
How does Allergic Rhinitis Present?
Patients with allergic rhinitis typically are wide ranging. The condition can begin in patients as young as two years. The symptoms, features, and clinical findings associated with allergic rhinitis include Rhinorrhea, nasal congestion, postnasal drainage, Repetitive sneezing, snoring, frequent sore throat, constant clearing of the throat, cough, headaches, and pale nasal turbinate among others.
How is Allergic Rhinitis Diagnosed?
Allergic rhinitis is diagnosed mainly through history and allergic tests.
How is Allergic Rhinitis Treated?
Allergic rhinitis is treated through allergen elimination or avoidance. Topical nasal steroids may be helpful.
What is the Prognosis of Allergic Rhinitis?
The prognosis of allergic rhinitis is good a majority of patients live normal lives with the signs. Roughly, improve throughout the teenaged years, but most symptoms reappear later.