Amniotic fluid embolism is a sudden and unexpected life-threatening birth complication that can affect both mother and baby.
What is the Pathology of Amniotic Fluid Embolism?
The pathology of amniotic fluid embolism is:
-Etiology: The cause of amniotic fluid embolism is the breakdown in the placental barrier, such as from trauma
-Genes involved: None.
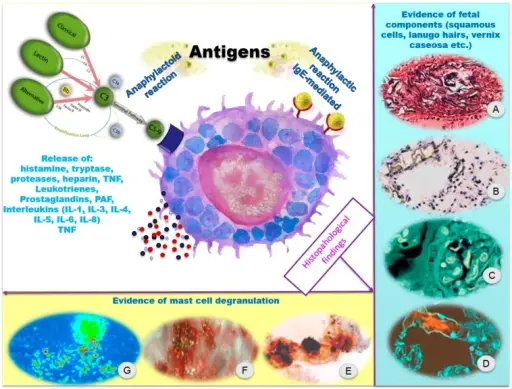
-Pathogenesis: The sequence of events that lead to amniotic fluid embolism is not clear. A possible cause is that any breach of the barrier between maternal blood and amniotic fluid forces the entry of amniotic fluid into the systemic circulation and results in a physical obstruction of the pulmonary circulation.
-Morphology: The morphology associated with amniotic fluid embolism shows that during labor, if the placental membranes tear at the same time the uterine veins rupture, then amniotic fluid can get into the bloodstream and travels to the lungs.
-Histology: The histology associated with amniotic fluid embolism shows fetal debris, epithelial squames in a peripheral pulmonary artery.
How does Amniotic Fluid Embolism Present?
Patients with amniotic fluid embolism typically affect females present at the age range of 35 and above. The symptoms, features, and clinical findings associated with amniotic fluid embolism include sudden shortness of breath, pulmonary edema, sudden low blood pressure, cardiovascular collapse, disseminated intravascular coagulopathy, bleeding from the uterus, cesarean incision or intravenous (IV) sites, altered mental state, fetal distress, seizures, and loss of consciousness.
How is Amniotic Fluid Embolism Diagnosed?
Amniotic fluid embolism is diagnosed using blood tests, ECG, pulse oximetry, chest X-ray, and echocardiogram.
How is Amniotic Fluid Embolism Treated?
Amniotic fluid embolism is treated with catheter placement as an emergency treatment, others include supplemental oxygen, medications, and blood/fluid transfusions.
What is the Prognosis of Amniotic Fluid Embolism?
The prognosis of amniotic fluid embolism is very poor as most women do not survive.