Insulinoma is a neuroendocrine tumor that causes endogenous hyperinsulinism.
What is the Pathology of Insulinoma?
The pathology of insulinoma is:
-Etiology: The cause of insulinoma is endogenous hyperinsulinism.
-Genes involved: MEN 1 gene.
-Pathogenesis: The sequence of events that lead to insulinoma is not documented.
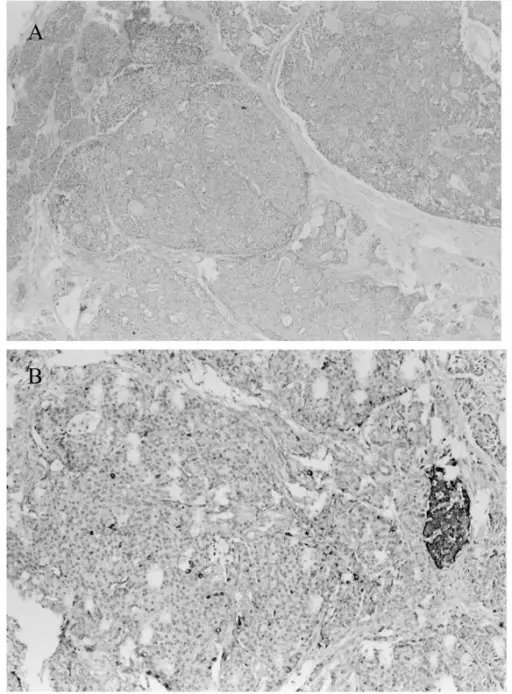
-Morphology: The morphology associated with insulinoma shows solitary well-encapsulated tumors and are alone and 0.5-10cm.
-Histology: None relevent.
How does Insulinoma Present?
Patients with insulinoma are typically more in females present at an age range of 30-60 years. The symptoms, features, and clinical findings associated with insulinoma include reduced sugar levels, diplopia, blurred vision, palpitations, weakness,
How is Insulinoma Diagnosed?
Insulinoma is diagnosed testing of serum insulin levels, glucose levels <40mg/dl, sulfonylurea negative, endoscopy, transabdominal high-resolution ultrasonography.
How is Insulinoma Treated?
Insulinoma is treated through medical care which include anti-hypoglycemics, and surgery.
What is the Prognosis of Insulinoma?
The prognosis of insulinoma is fair, but worsens if metastasis has occurred.