Autoimmune adrenalitis is a disorder in which the adrenal cortex is destroyed, resulting in the loss of mineralocorticoid, glucocorticoid, and adrenal androgen hormone production.
What is the Pathology of Autoimmune Adrenalitis?
The pathology of autoimmune adrenalitis is:
-Etiology: The cause of autoimmune adrenalitis is autoimmune adrenal destruction.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to autoimmune adrenalitis is that it results from the destruction of the adrenal cortex.
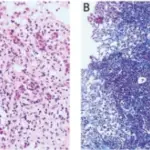
-Morphology: The morphology associated with autoimmune adrenalitis shows edema and hemorrhage that may also cause adrenomegaly with systemic infections, depending on the inciting cause.
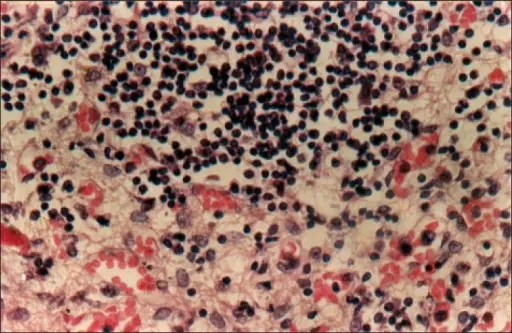
-Histology: The histology associated with autoimmune adrenalitis shows granulomatous inflammation that can be seen with fungal organisms, whereas some protozoal infections elicit mild histiocytic infiltration and necrosis.
How does Autoimmune Adrenalitis Present?
Patients with autoimmune adrenalitis typically are from all age groups. The symptoms, features, and clinical findings associated with autoimmune adrenalitis include fatigue, weakness, weight loss, and gastrointestinal upset.
How is Autoimmune Adrenalitis Diagnosed?
Autoimmune adrenalitis is diagnosed with laboratory testing to check for low cortisol level and determine whether the adrenal insufficiency is primary or secondary, measurement of 21-hydroxylase antibody levels.
How is Autoimmune Adrenalitis Treated?
Autoimmune adrenalitis is treated with lifelong hormone therapy with glucocorticoids and mineralocorticoids.
What is the Prognosis of Autoimmune Adrenalitis?
The prognosis of autoimmune adrenalitis is fair.