Autoimmune gastritis is an increasingly prevalent, organ-specific, immune-mediated disorder characterized by the destruction of gastric parietal cells, leading to the loss of intrinsic factor and reduced acid output.
What is the Pathology of Autoimmune Gastritis?
The pathology of autoimmune gastritis is:
-Etiology: The cause of autoimmune gastritis is unknown but affected people are likely to have other autoimmune disorders including autoimmune thyroiditis, diabetes type I, Addison’s disease, and vitiligo.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to autoimmune gastritis are restricted to oxyntic acid-producing mucosa in the corpus anatomic body and fundus of the stomach. Normally, the parietal cells in the oxyntic mucosa produce hydrochloric acid and intrinsic factor.
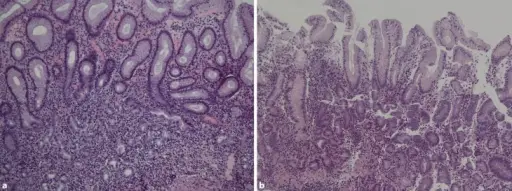
-Histology: The histology associated with autoimmune gastritis shows diffuse mononuclear infiltrates within the lamina propria that are heavier in the deeper, glandular portions. Patchy lymphocytic infiltrates and damage to oxyntic glands.
How does Autoimmune Gastritis Present?
Patients with autoimmune gastritis typically are all sexes at any age. The symptoms, features, and clinical findings associated with autoimmune gastritis include nausea, vomiting, a feeling of fullness in the upper abdomen after eating, or abdominal pain.
How is Autoimmune Gastritis Diagnosed?
Autoimmune gastritis is diagnosed by certain blood test, biopsy of stomach lining.
How is Autoimmune Gastritis Treated?
Autoimmune gastritis is treated by treating vitamin B12 and iron deficiencies, antibiotics for bacterial infections.
What is the Prognosis of Autoimmune Gastritis?
The prognosis of autoimmune gastritis is good. In some cases, acute gastritis can lead to serious or life-threatening complications, such as gastrointestinal hemorrhage.