Autoimmune hepatitis is liver inflammation that occurs when the body’s immune system turns against liver cells.
What is the Pathology of Autoimmune Hepatitis?
The pathology of autoimmune hepatitis is:
-Etiology: The cause of autoimmune hepatitis is related to autoimmune factors.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to autoimmune hepatitis includes genetic predisposition, molecular mimicry, and/or impairment of regulatory T-cells are involved in the initiation and perpetuation of the autoimmune liver attack.
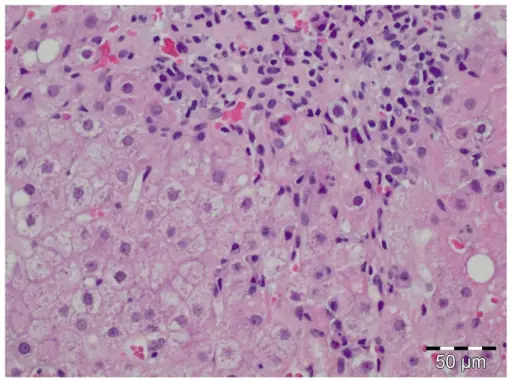
-Histology: The histology associated with autoimmune hepatitis shows a chronic hepatitis pattern of injury with portal inflammation and interface activity, the predominance of plasma cells in the portal infiltrate, emperipolesis, and hepatocellular rosette formation.
How does Autoimmune Hepatitis Present?
Patients with autoimmune hepatitis typically affect females present in the age range of the 50s. The symptoms, features, and clinical findings associated with autoimmune hepatitis include anorexia, arthralgias, maculopapular rash, fatigue, and also acute hepatitis manifestations.
How is Autoimmune Hepatitis Diagnosed?
Autoimmune hepatitis is diagnosed based on a combination of characteristic clinical features and typical laboratory abnormalities.
How is Autoimmune Hepatitis Treated?
Autoimmune hepatitis is treated with corticosteroid therapy and liver transplantation.
What is the Prognosis of Autoimmune hepatitis?
The prognosis of autoimmune hepatitis is good with a 10-year survival rate.