Breast pathology is disease or disorder of the breast.
Breast pathology includes:
- Developmental disorders of the breast
- Inflammatory disorders of the breast
- Benign epithelial lesions of the breast
- Carcinomas of the breast
- Stromal tumors of the breast
What are Developmental Disorders of the Breast?
Developmental disorders of the breast are breast issues that are due to syndromic, genetic, acquired, or sporadic conditions. Developmental disorders of the breast typically present in childhood or adolescents, but the age of presentation may vary. The clinical presentation depends on the underlying cause. Developmental disorders of the breast may be bilateral or unilateral.
Examples of Developmental Disorders of the Breast include:
- Accessory axillary breast tissue
- Congenital nipple inversion
- Milk line remnants
What is Accessory Axillary Breast Tissue?
Accessory axillary breast tissue is due to residual breast tissue that remains after normal embryologic development. Accessory axillary breast tissue is an uncommon condition. Accessory axillary breast tissue is located in the axilla (armpits) where it can cause diagnostic difficulty, especially if it is large.
What is the Pathology of Accessory Axillary Breast Tissue?
The pathology of accessory axillary breast tissue is:
-Etiology: The cause of accessory axillary breast tissue is a hormonal stimulation and may become more evident during menarche, pregnancy, or lactation. The hormonal changes during pregnancy and lactation may cause accessory breast tissue to increase in size and stimulate lactation.
-Pathogenesis: The sequence of events that lead to accessory axillary breast tissue is the failure of regression or displacement of the milk line. The independently migrating nests of precursor primordial breast cells can develop in a completely random manner or accessory breast tissue develops from modified apocrine sweat glands.
-Morphology: Aberrant breast tissue is usually present along the milk line, either above or below the normal breast location. It is commonly located in the axilla, but may be located outside the milk line, which includes the face, neck, trunk, and extremities.
-Histology: The histology associated with accessory axillary breast tissue shows the accessory fragments of breast tissue outside the periphery of the gland lacks organized secretory systems.
How does Accessory Axillary Breast Tissue Present?
Patients with accessory axillary breast tissue typically are female although they may be male. Accessory axillary breast tissue may present at age range. The symptoms, features, and clinical findings associated with accessory axillary breast tissue include fluctuating swelling or tenderness of breasts. The accessory nipples and areolas may darken. Decreased progesterone may cause accessory axillary breast tissue to become engorged and painful, which is the case a few days after delivering a baby. Occasionally, milk ducts within the accessory axillary breast tissue may become engorged, causing pain in the armpit.
How is Accessory Axillary Breast Tissue Diagnosed?
Accessory axillary breast tissue is diagnosed by physical exam, which may further requir imaging evaluation that may include an ultrasound or mammography. Occasionally, diagnostic breast MRI is used in challenging circumstances.
How is Accessory Axillary Breast Tissue Treated?
Accessory axillary breast tissue is treated with surgery such as liposuction or excision. Patients may enjoy an elimination of undesirable contours in the underarm area.
What is the Prognosis of Accessory Axillary Breast Tissue?
The prognosis of accessory axillary breast tissue is good.
What is Congenital Nipple Inversion?
Congenital nipple inversion is a condition in which the nipple is retracted inwards, rather than pointing outwards.
What is the Pathology of Congenital Nipple Inversion?
The pathology of congenital nipple inversion is:
-Etiology: The cause of congenital nipple inversion is a benign congenital maldevelopment. Faulty developmental patterns in the mesoderm fail to raise the nipple above the areolar plane.
-Pathogenesis: The sequence of events that lead to congenital nipple inversion is the milk ducts that don’t fully develop or the nipple base that remained small while in the womb.
-Morphology: The morphology associated with congenital nipple inversion shows that the projection of the inverted nipple lies beneath the areolar plane.
How does Congenital Nipple Inversion Present?
Patients with congenital nipple inversion present with inverted nipples.
How is Congenital Nipple Inversion Diagnosed?
Congenital nipple inversion can be diagnosed with a physical exam.
How is Congenital Nipple Inversion Treated?
Congenital nipple inversion can be treated with non-invasive techniques. Methods mainly involve using devices to create suction on the nipple-areolar complex to protract the nipple and maintain the protraction.
What is the Prognosis of Congenital Nipple Inversion?
The prognosis of congenital nipple inversion is good.
What are Inflammatory Disorders of the Breast?
Inflammatory disorders of the breast are divided into three categories: infectious mastitis, non-infectious mastitis, and mastitis related to underlying malignancy.
Examples of Inflammatory Disorders of the Breast include:
- Acute mastitis
- Duct ectasia
- Fat necrosis
- Granulomatous mastitis
- Lymphocytic mastopathy aka sclerosing lymphocytic lobulitis
- Squamous metaplasia of lactiferous ducts
What is Acute Mastitis?
Acute mastitis is the infection or inflammation of breast tissue, usually bacterial, often seen in association with lactation. If inflammatory disorders are left untreated it may form abscess and fistulous tracts.
What is the Pathology of Acute Mastitis?
The pathology of acute mastitis is:
-Etiology: The cause of acute mastitis is associated with lactation, cracks in nipple, eczema, nipple dermatoses, and postreduction mammoplasty. Infections are usually due to Staphylococcus aureus. Nonpregnancy related infections may be polymicrobial or associated with diabetes.
-Pathogenesis: The sequence of events that lead to acute mastitis is the accumulation of inadequately drained milk in ducts and lobules that creates a microenvironment that fosters bacterial growth.
-Morphology: The morphology associated with acute mastitis shows a hypoechoic lesion on ultrasound with purulent material, well circumscribed, macrolobulated, irregular, or ill-defined with septa and thick echogenic rim. Staphylococcus aureus is the most common organism and the microscopic examination reveals a mixed dense acute inflammatory infiltrate.
-Histology: The histology associated with acute mastitis shows that it may obscure underlying normal breast tissue and the tissue necrosis may be present. Gram stain for microorganisms can reveal bacterial forms (gram positive cocci) associated with neutrophilic infiltrate, granulation tissue, and chronic inflammation with resolution.
How does Acute Mastitis Present?
Patients with acute mastitis typically are female that present at an age range of reproductive age groups. The symptoms, features, and clinical findings associated with acute mastitis include erythema, swelling, firmness, breast pain, fever, malaise, decreased milk outflow and, an abscess.
How is Acute Mastitis Diagnosed?
Acute mastitis is diagnosed based on physical exam. Ultrasound is preferred imagining modality. The biopsy may be warranted for suspected abscess, atypical presentation, recurrent infection.
How is Acute Mastitis Treated?
Acute mastitis may be treated by incision and drainage. Analgesia, warm compress, and targeted antibiotics may be utilized as well.
What is the Prognosis of Acute Mastitis?
The prognosis of acute mastitis is good. The recurrent breast abscesses are more likely to be smokers and have mixed bacterial and anaerobic infections.
What is Duct Ectasia?
Duct ectasia is a disorder of the extralobular ducts which is characterized by different degrees of periductal inflammation, periductal fibrosis, and duct dilatation.
What is the Pathology of Duct Ectasia?
The pathology of duct ectasia is:
-Etiology: The cause of duct ectasia is not well known. Possible causes may include smoking, hyperprolactinemia, and phenothiazine treatment.
-Pathogenesis: The sequence of events that lead to duct ectasia is the stasis caused by duct obstruction which is the inciting cause of duct inflammation with further obstruction.
-Morphology: The morphology associated with duct ectasia shows firm fibrotic breast tissue with prominent dilated and the thick walled ducts filled with a tan-white, beige, or granular secretions. Calcifications with abscess formation may also be present.
-Histology: The histology associated with duct ectasia shows duct dilation with foamy histiocytes within the luminal secretions and infiltrating the wall of the involved ducts.
How does Duct Ectasia Present?
Patients with duct ectasia are typically older females. The symptoms, features, and clinical findings associated with duct ectasia include pain, nipple discharge which can be clear, cloudy, or bloody and the nipple retraction which is worm-like doughy palpable mass beneath the nipple.
How is Duct Ectasia Diagnosed?
Duct ectasia is diagnosed by biopsy.
How is Duct Ectasia Treated?
For many women mammary duct ectasia resolves on its own with no treatment and some women find that simple care, like warm compresses applied to the breast, is enough to manage symptoms. Duct ectasia may be treated by surgery.
What is the Prognosis of Duct Ectasia?
The prognosis of duct ectasia is good. If it’s left untreated a bacterial infection causing duct ectasia may cause more widespread infection and tissue damage, but mammary duct ectasia doesn’t increase the risk for breast cancer.
What is Fat Necrosis?
Fat necrosis is characterized by necrotic adipose tissue with foamy histiocytes, chronic inflammatory cells, and multinucleated giant cells.
What is the Pathology of Fat Necrosis?
The pathology of fat necrosis is:
-Etiology: Fat necrosis may be caused by trauma, iatrogenic injury, or radiation therapy.
-Pathogenesis: Fat necrosis.
-Morphology: The morphology associated with fat necrosis shows lipid laden histiocytes (lipophages), multinucleated giant cells, and degenerating adipocytes.
-Histology: The histology associated with fat necrosis shows necrosis of adipocytes.
How does Fat Necrosis Present?
Patients with fat necrosis typically are older females. The symptoms, features, and clinical findings associated with fat necrosis include a painless superficial solitary mass which may mimic cancer.
How is Fat Necrosis Diagnosed?
Fat necrosis can be diagnosed by physical exam, diagnosed by palpation of the breast mass, radiographical findings, and correlation with clinical history of trauma or breast procedures.
How is Fat Necrosis Treated?
Fat necrosis is treated by surgical excision, but it’s used only for painful or aesthetically undesirable lesions. Biopsy of the lesion is necessary to confirm the diagnosis.
What is the Prognosis of Fat Necrosis?
The prognosis of fat necrosis is good. It should resolve or regress over time, but the degenerated fat may persist for years within a fibrotic scar.
What is Granulomatous Mastitis?
Granulomatous mastitis is the inflammatory process of the breast usually due to Corynebacterium species.
What is the Pathology of Granulomatous mastitis?
The pathology of granulomatous mastitis is:
-Etiology: The cause of granulomatous mastitis inflammation and granulomas.
-Genes involved: 16S rRNA and rpoB gene sequencing.
-Pathogenesis: The sequence of events that lead to granulomatous mastitis is the nonspecific lobulitis, a granulomatous formation with central suppurative necrosis, abscesses, trauma, and non-puerperal secretion.
-Morphology: The morphology associated with granulomatous mastitis shows granulomas comprised of epithelioid histiocytes and giant cells with central lipid vacuoles containing bacteria and polymorphonuclear cells.
-Histology: The histology associated with granulomatous mastitis shows the lobulocentric mixed inflammatory infiltrate composed of lymphocytes, neutrophils, and scattered multinucleated giant cells.
How does Granulomatous Mastitis Present?
Patients with granulomatous mastitis typically are female. The symptoms, features, and clinical findings associated with granulomatous mastitis include a painful breast mass, nipple inversion or sinus formation.
How is Granulomatous Mastitis Diagnosed?
Granulomatous mastitis is diagnosed by microscopic examination and Gram stain with or without microbiologic culture.
How is Granulomatous Mastitis Treated?
Granulomatous mastitis is treated with antibiotics and steroids. Empirical antimicrobial therapy may be started prior to histologic diagnosis and lipophilic antibiotics, such as doxycycline, trimethoprim sulfamethoxazole, clarithromycin, and rifampicin. Surgery may involve incision, drainage, excision, or mastectomy.
What is the Prognosis of Granulomatous Mastitis?
The prognosis of granulomatous mastitis is fair.
What is Lymphocytic Mastopathy aka Sclerosing Lymphocytic Lobulitis?
Lymphocytic mastopathy aka sclerosing lymphocytic lobulitis is an uncommon fibroinflammatory lesion that courses with the presence of benign breast nodules.
What is the Pathology of Lymphocytic Mastopathy aka Sclerosing Lymphocytic Lobulitis?
The pathology of lymphocytic mastopathy aka sclerosing lymphocytic lobulitis is:
-Etiology: The cause of lymphocytic mastopathy aka sclerosing lymphocytic lobulitis is not clear.
-Pathogenesis: The sequence of events that lead to lymphocytic mastopathy aka sclerosing lymphocytic lobulitis includes persistent high blood glucose levels, as well as previously having a diabetic complication, such as neuropathy.
-Morphology: The morphology associated with lymphocytic mastopathy shows a dense fibrous tissue with hard lesion.
How does Lymphocytic Mastopathy aka Sclerosing Lymphocytic Lobulitis Present?
Patients with lymphocytic mastopathy aka sclerosing lymphocytic lobulitis are typically female. The symptoms, features, and clinical findings associated with lymphocytic mastopathy aka sclerosing lymphocytic lobulitis include a palpable mass, which can be painful.
How is Lymphocytic Mastopathy aka Sclerosing Lymphocytic Lobulitis Diagnosed?
Lymphocytic mastopathy aka sclerosing lymphocytic lobulitis is diagnosed using a core biopsy.
How is Lymphocytic Mastopathy aka Sclerosing Lymphocytic Lobulitis Treated?
Lymphocytic mastopathy aka sclerosing lymphocytic lobulitis is treated with a core biopsy which is performed under ultrasound guidance and it removes the central part of lumps.
What is the Prognosis of Lymphocytic Mastopathy aka Sclerosing Lymphocytic Lobulitis?
The prognosis of lymphocytic mastopathy aka sclerosing lymphocytic lobulitis is fair.
What is Squamous Metaplasia of Lactiferous Ducts?
Squamous metaplasia of lactiferous ducts is when the normal cuboidal epithelium lining the lactiferous ducts is replaced by squamous epithelium, leading to intraluminal accumulation of epithelial debris.
What is the Pathology of Squamous Metaplasia of Lactiferous Ducts?
The pathology of squamous metaplasia of lactiferous ducts is:
-Etiology: The cause of squamous metaplasia of lactiferous ducts is strongly correlated with smoking.
-Pathogenesis: The sequence of events that lead to squamous metaplasia of lactiferous ducts is the normal cuboidal epithelium lining the lactiferous ducts which is replaced by squamous epithelium.
-Morphology: The morphology associated with squamous metaplasia of lactiferous ducts shows a retro-areolar asymmetrical density, squamous cells, and mixed inflammation including macrophages.
-Histology: The histology associated with squamous metaplasia shows squamous epithelium extending beyond the normal transition point to ductal epithelium. The duct spaces are filled with keratin debris.
How does Squamous Metaplasia of Lactiferous Ducts Present?
Patients with squamous metaplasia of lactiferous ducts typically are either male or female present at age range of wide age groups. The symptoms, features, and clinical findings associated with squamous metaplasia of lactiferous ducts include a retro-areolar, predominately medial, ill-defined, hypoechoic lesion with either abscess or sinus and fistula formation.
How is Squamous Metaplasia of Lactiferous Ducts Diagnosed?
Squamous metaplasia of lactiferous ducts is diagnosed through mammography and ultrasonography. Pathology tissue confirmation is always required and this can be by histology of a core biopsy or excision specimen, or fine-needle aspiration (FNA) cytology.
How is Squamous Metaplasia of Lactiferous Ducts Treated?
Squamous metaplasia of lactiferous ducts is treated by duct excision of the affected duct.
What is the Prognosis of Squamous Metaplasia of Lactiferous Ducts?
The prognosis of squamous metaplasia of lactiferous ducts is fair.
What are Benign Epithelial Lesions of the Breast?
Benign epithelial lesions of the breast are lumps that grow in non-cancerous areas where breast cells grow abnormally and rapidly.
Examples of Benign Epithelial Lesions of the Breast include:
- Fibrocystic Changes
- Gynecomastia
- Atypical Ductal Hyperplasia
- Atypical Lobular Hyperplasia
What are Fibrocystic Changes?
Fibrocystic changes are also called diffuse cystic mastopathies. It is a general category for numerous entities, described separately.
What is the Pathology of Fibrocystic Changes?
The pathology of fibrocystic changes is:
-Etiology: The cause of fibrocystic changes is associated with hormonal imbalance or increased estrogen to progesterone ratio, decreased risk with oral contraceptives, perhaps due to balanced supply of estrogens and progesterone.
-Pathogenesis: The sequence of events that lead to fibrocystic changes is determined by estrogen predominance and progesterone deficiency that result in hyperproliferation of connective tissue or fibrosis.
-Morphology: The morphology associated with fibrocystic changes shows clear or blue domed cysts.
-Histology: The histology associated with fibrocystic changes shows the variably-sized cysts scattered in fibrotic breast tissue.
How does Fibrocystic Changes Present?
Patients with fibrocystic changes typically are female. The symptoms, features, and clinical findings associated with fibrocystic changes include that they’re usually bilateral, although one breast may be affected more than the other.
How is Fibrocystic Changes Diagnosed?
Fibrocystic changes are diagnosed through a clinical breast exam. They also can be diagnosed through imaging tests, such as mammography and ultrasound.
How is Fibrocystic Changes Treated?
Fibrocystic changes is treated by estrogen replacement therapy or estrones in adipose tissue.
What is the Prognosis of Fibrocystic Changes?
The prognosis of fibrocystic changes is fair.
What is Gynecomastia?
Gynecomastia is the benign enlargement of the male breast, typically presenting as a palpable subareolar mass. Histologically, identical gynecomastoid hyperplasia can be seen in the female breast.
What is the Pathology of Gynecomastia?
The pathology of gynecomastia is:
-Etiology: The cause of gynecomastia is imbalance of estrogens and androgens.
-Genes involved: p63
-Pathogenesis: The sequence of events that lead to gynecomastia is that it seems to primarily result from an imbalance of androgenic and estrogenic influences on breast tissue. Estrogens stimulate the proliferation of breast tissue. Androgens inhibit.
-Morphology: The morphology associated with gynecomastia is enlarged breast tissue.
-Histology: The morphology associated with gynecomastia shows biphasic epithelial with stromal fragments in the background of scattered single bipolar nuclei.
How does Gynecomastia Present?
Patients with gynecomastia are typically male with enlarged breast tissue.
How is Gynecomastia Diagnosed?
Gynecomastia is diagnosed through histologic changes.
How is Gynecomastia Treated?
Gynecomastia is treated medically with aromatase inhibitor, anti-estrogen, and androgen therapy (tamoxifen, danazol). Surgical intervention may be utilized as well.
What is the Prognosis of Gynecomastia?
The prognosis of gynecomastia is fair.
What is Atypical Ductal Hyperplasia?
Atypical ductal hyperplasia is the intraductal clonal epithelial cell proliferation with similar histologic features, but insufficient involvement or volume for the diagnosis of the low grade ductal carcinoma in situ.
What is the Pathology of Atypical Ductal Hyperplasia?
The pathology of atypical ductal hyperplasia is:
-Etiology: The cause of atypical ductal hyperplasia is EZH2 (enhancer of zeste homolog 2) and its overexpression has an important role in oncogenesis. The lifelong exposure to estrogen causes a continued accumulation of genomic changes leading to defective growth control.
-Pathogenesis: The sequence of events that lead to atypical ductal hyperplasia is the low grade model of progression from normal breast or benign proliferative breast disease to atypical ductal hyperplasia.
-Morphology: The morphology associated with atypical ductal hyperplasia may be a lump.
-Histology: The histology associated with atypical ductal hyperplasia shows well defined, monomorphic cells with evenly spaced small rounded nuclei.
How does Atypical Ductal Hyperplasia Present?
Patients with atypical ductal hyperplasia typically are female with breast concerns.
How is Atypical Ductal Hyperplasia Diagnosed?
Atypical ductal hyperplasia is diagnosed by biopsy.
How is Atypical Ductal Hyperplasia Treated?
Atypical ductal hyperplasia is treated by excision, with some variation directed by imaging findings.
What is the Prognosis of Atypical Ductal Hyperplasia?
The prognosis of atypical ductal hyperplasia is fair.
What is Atypical Lobular Hyperplasia?
Atypical lobular hyperplasia is a clonal proliferation of discohesive epithelial cells arising in terminal duct lobular units.
What is the Pathology of Atypical Lobular Hyperplasia?
The pathology of atypical lobular hyperplasia is:
-Etiology: The cause of atypical lobular hyperplasia is the increased expression of ESR1 and decreased expression of SFRP1.
-Pathogenesis: The sequence of events that lead to atypical lobular hyperplasia is the 16q loss or CDH1 deletion and loss of function of E-cadherin.
-Morphology: The morphology associated with atypical lobular hyperplasia shows loosely cohesive cell clusters composed of uniform cells with occasional intracytoplasmic lumina with minimal nuclear atypia.
-Histology: The histology associated with atypical lobular hyperplasia shows the solid, discohesive proliferation of cells that are monomorphic, small, have pale pink cytoplasm, uniform oval nuclei, and indistinct nuclei.
How does Atypical Lobular Hyperplasia Present?
Patients with atypical lobular hyperplasia typically are more female present at age range of wide age groups, but most commonly diagnosed in 50s.
How is Atypical Lobular Hyperplasia Diagnosed?
Atypical lobular hyperplasia is diagnosed by core biopsy, mammography, ultrasound, or MRI.
How is Atypical Lobular Hyperplasia Treated?
Atypical lobular hyperplasia is treated with selective estrogen receptor modulators (SERMs) and aromatase inhibitors (AIs).
What is the Prognosis of Atypical Lobular Hyperplasia?
The prognosis of atypical lobular hyperplasia is fair.
What are Carcinomas of the Breast?
Carcinomas of the breast are the diseases in which cells in the breast grow out of control.
Examples of Carcinomas of the Breast include:
- Ductal carcinoma in situ
- Lobular carcinoma in situ
- Invasive carcinoma
- Pagets disease of the breast
What is Ductal Carcinoma in Situ?
Ductal carcinoma in situ is a neoplastic proliferation of mammary ductal epithelial cells confined to the ductal-lobular system without evidence of invasion through the basement membrane into the surrounding stroma.
What is the Pathology of Ductal Carcinoma in Situ?
The pathology of ductal carcinoma in situ is:
-Etiology: The cause of ductal carcinoma in situ is not clear, but is thought to be due to genetic mutations occur in the DNA of breast duct cells.
-Genes involved: Mutation in BRCA1 or BRCA2.
-Pathogenesis: The sequence of events that lead to ductal carcinoma in situ is the high estrogen states, such as use of oral contraceptive (OC) pills, nulliparity, advanced age at first birth, and also family history and genetic mutations.
-Morphology: The morphology associated with ductal carcinoma in situ may be a lump.
-Histology: The morphology associated with ductal carcinoma in situ shows cohesive sheets and aggregates. Microcalcifications may be present.
How does Ductal Carcinoma in Situ Present?
Patients with ductal carcinoma in situ typically are female present at age range of 50 – 59 years. The symptoms, features, and clinical findings associated with ductal carcinoma in situ include that majority are non-palpable and detected mammographically as microcalcifications.
How is Ductal Carcinoma in Situ Diagnosed?
Ductal carcinoma in situ is diagnosed by screening and diagnostic mammography, with final diagnosis confirmed by biopsy.
How is Ductal Carcinoma in Situ Treated?
Ductal carcinoma in situ is treated by breast conserving surgery alone or breast conserving surgery with radiotherapy or mastectomy and the adjuvant therapy.
What is the Prognosis of Ductal Carcinoma in Situ?
The prognosis of ductal carcinoma in situ is good and patients diagnosed with DCIS have an excellent long-term breast-cancer-specific survival.
What is Lobular Carcinoma in Situ?
Lobular Carcinoma in Situ is the lobulocentric proliferation of small uniform cells which fill and distend most of the acini in the involved lobule.
What is the Pathology of Lobular Carcinoma in Situ?
The pathology of lobular carcinoma in situ is:
-Etiology: The cause of lobular carcinoma in situ are the genetic mutations developed in a milk-producing gland of a breast.
-Genes involved: Mutations in the CDH1.
-Pathogenesis: The sequence of events that lead to lobular carcinoma in situ is when genetic mutations occur in the DNA of breast duct cells.
-Morphology: The morphology associated with lobular carcinoma in situ may include breast assymetry or a mass lesion.
-Histology: The histology associated with lobular carcinoma in situ shows terminal duct lobular unit with expanding acini and proliferation loosley cohesive of monomorphic cells.
How does Lobular Carcinoma in Situ Present?
Patients with lobular carcinoma in situ typically are older females.
How is Lobular Carcinoma in Situ Diagnosed?
Lobular carcinoma in situ is diagnosed by biopsy and histologic examination.
How is Lobular Carcinoma in Situ Treated?
Lobular carcinoma in situ is treated with lumpectomy or mastectomy, and possible sentinel lymph node biopsy.
What is the Prognosis of Lobular Carcinoma in Situ?
The prognosis of lobular carcinoma in situ is fair.
What is Invasive Papillary Carcinoma?
Invasive papillary carcinoma is a rare type of invasive ductal carcinoma.
What is the Pathology of Invasive Papillary Carcinoma?
The pathology of with invasive papillary carcinoma is:
-Etiology: The cause of with invasive papillary carcinoma may be due to radiation exposure.
-Genes involved: MMPs, NGF/NTRK1
-Pathogenesis: The sequence of events that lead to invasive papillary carcinoma are thought to be due to major chromosomal changes: 16p gain, 16q loss, 1q gain and 7q loss.
-Morphology: The morphology associated with with invasive papillary carcinoma shows the solitary mass, solid and cystic, round, oval, lobulated, or irregular.
-Histology: The histology associated with invasive papillary carcinoma shows invasive carcinoma with papillary architecture and an invasive growth pattern without a surrounding fibrous capsule. The growth pattern is arborizing fibrovascular stalks lined by epithelial cells.
How does Invasive Papillary Carcinoma Present?
Patients with invasive papillary carcinoma typically are female present at age range of sixth to eighth decade that present with breast concerns.
How is Invasive Papillary Carcinoma Diagnosed?
Invasive carcinoma is diagnosed through mammogram, breast ultrasound (US), and breast MRI, and biopsy.
How is Invasive Papillary Carcinoma Treated?
Invasive carcinoma is treated by surgical excision followed by adjuvant radiation and systemic therapy based on the predictive and prognostic factors.
What is the Prognosis of Invasive Papillary Carcinoma?
The prognosis of invasive papillary carcinoma is good when compared with invasive ductal carcinoma. Poor prognostic factors include old age, advanced pathologic stage, and patients without radiation.
What is Pagets Disease of the Breast?
Pagets disease of the breast is a proliferation of malignant glandular epithelial cells in the nipple areolar epidermis.
What is the Pathology of Pagets Disease of the Breast?
The pathology of Pagets disease of the breast is:
-Etiology: The cause of pagets disease of the breast is an underlying ductal breast cancer in which the malignant cells travel through milk ducts to the nipple and its surrounding skin.
-Genes involved: HER2/NEU
-Pathogenesis: The sequence of events that lead to Pagets disease of the breast is the epidermis of the nipple is infiltrated by large neoplastic cells of glandular origin induced by a motility factor that acts via the HER2/NEU receptor.
-Morphology: The morphology associated with Pagets disease of the breast is typically a lump or assymetry.
-Histology: The histology associated with pagets disease of the breast shows isolated and loosely clustered malignant glandular cells with enlarged nuclei, prominent nucleoli, and pale cytoplasm detected among squamous cells.
How does Pagets Disease of the Breast Present?
Patients with Pagets disease of the breast typically are either male or female with nipple concerns.
How is Pagets Disease of the Breast Diagnosed?
Pagets disease of the breast is diagnosed clinically and confirmed by histologic examination.
How is Pagets Disease of the Breast Treated?
Pagets disease of the breast is treated with breast conserving therapy with central lumpectomy and whole breast irradiation for patients with limited disease. Surgical intervention may be utilized for larger lesions.
What is the Prognosis of Pagets Disease of the Breast?
The prognosis of pagets disease of the breast is fair.
What is Familial Breast Cancer?
Familial breast cancer is a cluster of breast cancer within a family.
What is the Pathology of Familial Breast Cancer?
The pathology of familial breast cancer is:
-Etiology: The cause of familial breast cancer are mutations in the high penetrance genes.
-Genes involved: p53, PTEN, ATM and STK11, BRCA1 and BRCA2, CHEK2, TP53, LKB1, CDH1, NBS1, RAD50, BRIP1, and PALB2.
-Pathogenesis: The sequence of events that lead to familial breast cancer is that the patient with one or more first-degree relatives with breast cancer in this familial breast cancer category has a substantial excess lifetime risk of breast cancer when compared with patients in the general population who do not have affected first-degree relatives.
-Morphology: The morphology associated with familial breast cancer typically is a breast lump.
-Histology: The histology associated with familial breast cancer shows a high-grade invasive ductal carcinoma of no special type and display minimal if any tubule or glandular formation, markedly pleomorphic nuclei, vesicular chromatin, prominent nucleoli, and high mitotic activity.
How does Familial Breast Cancer Present?
Patients with familial breast cancer typically are female with a family history of breast cancer.
How is Familial Breast Cancer Diagnosed?
Familial breast cancer is diagnosed through medical history, symptoms, physical exam, and laboratory test results, and biopsy.
How is Familial Breast Cancer Treated?
Familial breast cancer may be treated with prophylactic bilateral mastectomy which reduces the risk of breast cancer by almost 100% in mutation carriers.
What is the Prognosis of Familial Breast Cancer?
The prognosis of familial breast cancer is poor.
What is Sporadic Breast Cancer?
Sporadic breast cancer is the cancer which develops from damage to a person’s genes that occurs by chance after they are born.
What is the Pathology of Sporadic Breast Cancer?
The pathology of sporadic breast cancer is:
-Etiology: The cause of sporadic breast cancer is alteration to a person’s genes.
-Genes involved: BRCA1 or BRCA2, MLH1, MSH2, MSH6, and PMS2, PTEN, TP53, STK11, ATM, CDH1, PALB2, and CHEK2.
-Pathogenesis: The sequence of events that lead to sporadic breast cancer is the spontaneous non-inherited genetic alteration that leads to breast malignancy.
-Morphology: The morphology associated with sporadic breast cancer tends to be a palpable breast mass.
-Histology: The histology associated with sporadic breast cancer varies widely, but is characterized by the presence of malignant cells.
How does Sporadic Breast Cancer Present?
Patients with sporadic breast cancer typically are female present at age range of older than 50 years. The symptoms, features, and clinical findings associated with sporadic breast cancer include palpable breast mass or breast pain. A change in the size or shape of the breast may be noted. Nipple discharge, tenderness, retraction (turning inward), skin irritation, dimpling, redness, or scaliness may also be present.
How is Sporadic Breast Cancer Diagnosed?
Sporadic breast cancer is diagnosed through the breast examinations and biopsy evaluation.
How is Sporadic Breast Cancer Treated?
Sporadic breast cancer may be treated by surgical intervention.
What is the Prognosis of Sporadic Breast Cancer?
The prognosis of sporadic breast cancer is fair. The late-onset familial breast cancers need more intensive therapy and a closer follow-up.
What are Stromal Tumors of the Breast?
Stromal tumors of the breast are biphasic tumors of the breast that exhibit low-grade malignant potential. Stromal tumors of the breast are characterized by proliferation of atypical spindle cells surrounding benign mammary ducts and infiltrating adjacent adipose tissue.
Examples of Stromal Tumors of the Breast include:
- Fibroadenoma
- Phyllodes Tumor
- Myofibroblastoma
- Fibromatosis
What is Fibroadenoma?
A fibroadenoma is a benign biphasic tumor composed of both glandular epithelial and stromal components of the terminal duct lobular unit.
What is the Pathology of Fibroadenoma?
The pathology of fibroadenoma is:
-Etiology: The cause of fibroadenoma is associated with cyclosporine immunosuppression.
-Genes involved: MED12 exon 2 mutations.
-Pathogenesis: The sequence of events that lead to fibroadenoma isn’t completely understood. Myxoid fibroadenoma is associated with Carney complex.
-Morphology: The morphology associated with fibroadenoma shows a palpable breast mass.
-Histology: The histology associated with fibroadenoma shows well circumscribed, unencapsulated, biphasic tumor, and proliferation of both glandular and stromal elements.
How does Fibroadenoma Present?
Patients with fibroadenoma typically are younger females with palpable breast masses.
How is Fibroadenoma Diagnosed?
Fibroadenoma is diagnosed by biopsy and histologic examination of involved tissue.
How is Fibroadenoma Treated?
Fibroadenoma is treated depending on patient’s risk factors and patient’s preference.
What is the Prognosis of Fibroadenoma?
The prognosis of fibroadenoma is good.
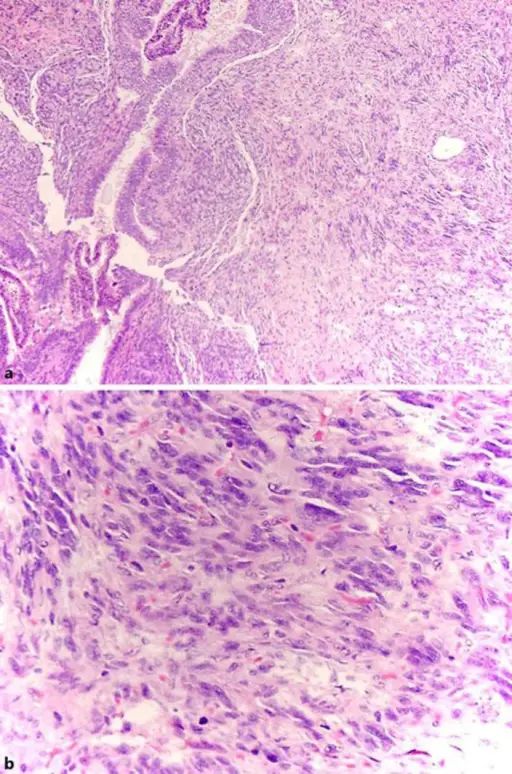
What is Phyllodes Tumor?
Phyllodes tumor is a biphasic fibroepithelial neoplasm with leaf-like epithelial (phyllodal) pattern and stromal proliferation.
What is the Pathology of Phyllodes Tumor?
The pathology of phyllodes tumor is:
-Etiology: The cause of phyllodes tumor is currently unclear.
-Genes involved: MED12 and RARA mutations.
-Pathogenesis: The sequence of events that lead to phyllodes tumor is the loss of epithelial interaction with stromal components. There is increased incidence of Phyllodes tumor in Li-Fraumeni syndrome.
-Morphology: The morphology associated with phyllodes tumor shows a palpable breast mass.
-Histology: The histology associated with phyllodes tumor shows the leaf-like epithelial pattern formed by an exaggerated intracanalicular pattern, subepithelial condensation with increased stromal cellularity adjacent to epithelium, cystic degeneration, hemorrhage, stromal hyalinization, and myxoid change.
How does Phyllodes Tumor Present?
Patients with phyllodes tumor typically are female with breast masses
How is Phyllodes Tumor Diagnosed?
Phyllodes tumor is diagnosed through the histologic diagnosis. .
How is Phyllodes Tumor Treated?
Phyllodes tumor is treated by local excision with clear margins.
What is the Prognosis of Phyllodes Tumor?
The prognosis of phyllodes tumor is fair.
What is Myofibroblastoma?
Myofibroblastoma is a benign spindle cell tumor of mammary stroma composed of fibroblasts and myofibroblasts.
What is the Pathology of Myofibroblastoma?
The pathology of myofibroblastoma is:
-Etiology: The cause of myofibroblastoma is the pathogenetic role of hormones due to ER, PR and AR expression.
-Genes involved: Loss of 13q14 region, including RB1 and FOXO1 loci
-Pathogenesis: The sequence of events that lead to myofibroblastoma is the proliferation of CD34+ mammary stromal fibroblasts and myofibroblasts capable of multidirectional mesenchymal differentiation.
-Morphology: The morphology associated with myofibroblastoma shows a palpable breast mass.
-Histology: The histology associated with myofibroblastoma shows a well-circumscribed lesion that lacks a true capsule with bland, uniform, monotonous short to elongated spindle cells arranged as short haphazard intersecting fascicles admixed with bands of hyalinized collagen.
How does Myofibroblastoma Present?
Patients with myofibroblastoma may be male or female. The symptoms, features, and clinical findings associated with myofibroblastoma include a painless, nontender, slow growing, mobile breast mass.
How is Myofibroblastoma Diagnosed?
Myofibroblastoma is diagnosed by imaging which includes ultrasound, mammogram, and MRI. The invasive procedures include biopsy and fine needle aspiration (FNA).
How is Myofibroblastoma Treated?
Myofibroblastoma is treated by surgical excision.
What is the Prognosis of Myofibroblastoma?
The prognosis of myofibroblastoma is good.
What is Fibromatosis?
Fibromatosis is the low grade’s infiltrative spindle cell neoplasm composed of fibroblasts and myofibroblasts.
What is the Pathology of Fibromatosis?
The pathology of fibromatosis is:
-Etiology: The cause of fibromatosis may include surgery or trauma.
-Genes involved: CTNNB1 mutation or inactivating APC mutation
-Pathogenesis: The sequence of events that lead to fibromatosis is through the WNT or beta catenin pathway these mutations motivate cells to proliferate while destabilizing beta catenin that then accumulates within the nucleus.
-Morphology: The morphology associated with fibromatosis shows a palpable breast mass.
-Histology: The histology associated with fibromatosis shows long intersecting fascicles composed of bland spindle cells with indistinct borders, hyperchromatic nuclei with occasional nucleoli, and eosinophilic cytoplasm.
How does Fibromatosis Present?
Patients with fibromatosis typically females with a complaint of a slow growing breast mass.
How is Fibromatosis Diagnosed?
Fibromatosis is diagnosed through mammography.
How is Fibromatosis Treated?
Fibromatosis is treated by surgical local excision.
What is the Prognosis of Fibromatosis?
The prognosis of fibromatosis is fair.