Cardiac pathology is any lesion, disease, or malignancy that involves the heart.
Examples of cardiac pathology includes:
- Conduction disorders
- Flow obstruction
- Pump failure
- Regurgitant flow
- Rupture of the heart
- Rupture of vessels
- Shunted flow
What are the Effects of Aging on the Heart?
Effects of aging on the heart are:
- Epicardial fat increases
- Basophilic degeneration
- Sigmoid septum
- Mitral annulus calcification
- Aortic valve calcification
- Prolapsing myxomatous mitral valve
- Lambl excrescences
What is Heart Failure?
Heart failure or congestive heart failure is an abnormality in the normal function of the heart, where the heart is not able to pump an adequate amount of blood to supply the tissues.
What is the Pathology of Heart Failure?
The pathology of heart failure is due to an injury in the myocardium caused by ischemia, hypertension, and diabetes.
How does Heart Failure Present?
Heart failure presents as exertional dyspnea, orthopnea, paroxysmal nocturnal dyspnea, dyspnea at rest, and acute pulmonary edema.
How is Heart Failure Diagnosed?
Diagnosis of heart failure includes a thorough history and physical exam, 2D echo, chest x-ray, and echocardiogram. Blood work is also required such as serum urea and electrolytes, creatinine, full blood count, and liver and thyroid function tests.
How is Heart Failure Treated?
Treatment of heart failure includes diuretics, inotropes, ACE-I, beta blockers, SGLT2 inhibitors, mineralocorticoid receptor antagonist, right heart catheterization, dapagliflozin and/ or heart transplantation for advanced cases.
What is the Prognosis of Heart Failure?
Heart failure prognosis is poor, with mortality at 10% 30 days after admission, and at 42% 5-years after diagnosis.
What is the Frank-Starling Mechanism?
The Frank-Starling mechanism describes the function of the heart in relation to its stretch and contraction. It states that as the left ventricular volume increases, its stroke volume will also increase as a result of the stretch that produces a more forceful systolic contraction.
What is Diastolic Dysfunction?
Diastolic dysfunction is a heart condition that causes left heart failure, where the heart chamber does not appropriately expand, causing inadequate filling of the chambers and blood backing up to the organs.
What is the Pathology of Diastolic Dysfunction?
Diastolic dysfunction is characterized by stiffening of the heart muscles, thereby limiting its stretch, leading to inadequate filling of blood.
How does Diastolic Dysfunction Present?
Diastolic dysfunction affects more than 25% of adults more than 40 years old. It presents as a progressive shortness of breath on exertion, easy fatigability, and water retention in lower extremities.
How is Diastolic Dysfunction Diagnosed?
Diastolic dysfunction can be diagnosed with the use of 2D echo.
How is Diastolic Dysfunction Treated?
Diastolic dysfunction is treated symptomatically with ACE inhibitors, calcium channel blockers, ARBs, and beta blockers. Prevention includes smoking cessation, lifestyle modification, and adequate control of hypertension.
What is the Prognosis of Diastolic Dysfunction?
Diastolic dysfunction prognosis is moderate with annual mortality of 5-8%.
What is Systolic Dysfunction?
Systolic dysfunction is an impairment in ventricular contraction, that is, the heart does not contract properly, due to changes in the regulation of excitation-contraction mechanisms. It may occur with or without preserved ejection fraction, with normal ejection fraction at 45% – 65%.
What is the Pathology of Systolic Dysfunction?
Systolic dysfunction occurs due to ineffective heart contraction that cannot effectively supply metabolic needs due to impaired intrinsic and extrinsic mechanisms. Mechanism of damage is due to destruction of myocytes resulting in infarction and eventual scar formation which leads to diminished function due to structural abnormality.
How does Systolic Dysfunction Present?
Systolic dysfunction presents as exertional dyspnea, orthopnea, paroxysmal nocturnal dyspnea, dyspnea at rest, and acute pulmonary edema.
How is Systolic Dysfunction Diagnosed?
Systolic dysfunction is diagnosed with history and physical examination, 2D echo and cardiac catheterization.
How is Systolic Dysfunction Treated?
Systolic dysfunction treatment includes pharmacologic management: ARBs, beta blockers, aldosterone antagonist, digoxin, diuretics, hydralazine and nitrates; and mechanical therapy using biventricular pacing, implantable cardioverter defibrillators, and left ventricular assist devices.
How is the Prognosis of Systolic Dysfunction?
Systolic dysfunction prognosis is good but survival rate decreases with time after diagnosis, with survival at 90% one year after diagnosis and decreases to 30% after a decade.
What is Cardiac Hypertrophy?
Cardiac Hypertrophy or Ventricular Hypertrophy is a result of a compensatory heart muscle thickening when the heart is under increased stress.
What is the Pathology of Cardiac Hypertrophy?
Cardiac hypertrophy pathology is characterized by a thickened heart muscle which results in smaller chambers and reduced pumping capacity of the heart.
How does Cardiac Hypertrophy Present?
Cardiac hypertrophy presents as shortness of breath with exertion, chest pain, arrhythmia, dizziness or syncope, chronic fatigue and leg edema.
How is Cardiac Hypertrophy Diagnosed?
Cardiac hypertrophy diagnosis is based on electrocardiogram, 2D echo, and MRI.
How is Cardiac Hypertrophy Treated?
Treatment for cardiac hypertrophy relies on early detection of the disease; medications such as beta blockers and calcium channel blockers relieve pressure on the heart, thereby preventing further thickening; surgery is also considered in advanced cases.
What is the Prognosis of Cardiac Hypertrophy?
Cardiac hypertrophy prognosis is good, with only 1% annual mortality.
What is Left-Sided Heart Failure?
Left-sided heart failure is a heart condition where the left ventricle is weakened, resulting in inadequate pumping of oxygen-rich blood to the body. It has two types: systolic failure with reduced ejection fraction and diastolic heart failure with preserved ejection fraction.
What is the Pathology of Left-Sided Heart Failure?
Left sided heart failure pathology is due to gradual weakening of the left ventricle.
How does Left-Sided Heart Failure Present?
Left sided heart failure presents as shortness of breath, difficulty breathing when lying down, and swelling of the lower extremities. Features generally resemble general features of heart failure.
How does Left-Sided Heart Failure Present?
Diagnosis of left sided heart failure is based on cardiac catheterization, chest x-ray, electrocardiogram, 2D echo, and treadmill stress test. Radionuclide imaging can also be used to assess extent of heart damage.
How does Left-Sided Heart Failure Present?
Treatment of left sided heart failure consists of pharmacologic approaches such as use of diuretics, ACE inhibitors, and beta blockers. Lifestyle changes and surgery that may include a left ventricular assist device (LVAD) surgery, pacemaker, repair surgery, and coronary artery bypass graft (CABG).
What is the Prognosis of Left-Sided Heart Failure?
Left sided heart failure prognosis is poor with a mortality of 25% 1 year after diagnosis, and patients with an ejection fraction of <15% have mortality of 50% in less than one year.
What is Right-Sided Heart Failure?
Right-sided heart failure or cor pulmonale is often caused by a left sided heart failure, causing blood to flow back to the lungs due to weakened left ventricle.
What is the Pathology of Right-Sided Heart Failure?
Right sided heart failure is due to impaired contractility caused by pressure, volume overload or contractile dysfunction.
How is Right-Sided Heart Failure?
Right sided heart failure presents as shortness of breath that awakens patients at night and during exercise or when lying flat, edema of the legs, ankles or feet, and abdominal distention.
How is Right-Sided Heart Failure Diagnosed?
Right sided heart failure diagnosis is based on blood tests, CT scan, chest x-ray, cardiac catheterization, coronary angiography, electrocardiogram, 2D and echo.
How is Right-Sided Heart Failure Treated?
Treatment for right sided heart failure is symptomatic, and drugs such as diuretics, beta blockers, pulmonary vasodilators, digoxin, and vasodilators may be used. Lifestyle changes are also essential and surgical procedures such as ventricular assist device (VAD) surgery and heart transplant may be done in advanced cases.
What is the Prognosis of Right-Sided Heart Failure?
Right sided heart failure prognosis is poor with a five-year survival rate of 47% and 2-year mortality of 25%.
What is Congenital Heart Disease?
Congenital heart disease is when a heart abnormalities present at birth that tend to produce shunting.
What are Left-to-Right Shunts?
Left-to-right shunts are characterized by backflow of blood from the systemic to pulmonary circulation.
Left-to-right shunts include:
- Atrial septal defect
- Patent ductus arteriosus
- Ventricular septal defect
What is an Atrial Septal Defect?
Atrial septal defect is characterized by an opening in the interatrial septum, which causes pulmonary circulation to pass directly to the right atrium, left-to-right shunt. Severity of manifestation varies depending on the extent of the defect. It has three types: ostium secundum, ostium primum, and sinus venosus.
What is the Pathology of Atrial Septal Defect?
Atrial septal defect pathology consists of an opening between the right and left atrium which leads to enlargement of the right and left atrium, as well as the main pulmonary artery. Most common cause is the non-closure of foramen ovale.
How does Atrial Septal Defect Present?
Atrial septal defect is 10% of all congenital heart diseases with ostium secundum consisting of 75% of all atrial septal defect cases. It occurs mostly in female patients and symptoms present by 40 years old in 90% of the untreated population. It presents as dyspnea on exertion, fatigue, palpitation, sustained arrhythmia, and/or evidence of heart failure.
How is Atrial Septal Defect Diagnosed?
Atrial septal defect is diagnosed based on chest x-ray, 2D echo, MRI, and electrocardiogram.
How is Atrial Septal Defect Treated?
Atrial septal defect can be managed with surgery or interventional catheterization.
What is the Prognosis of Atrial Septal Defect?
Atrial septal defect prognosis is good, with post-surgery improving the patient’s condition and reducing morbidity and mortality.
What is a Patent Ductus Arteriosus?
Patent ductus arteriosus is the persistent communication between the descending aorta and the pulmonary artery long after birth.
What is the Pathology of Patent Ductus Arteriosus?
Patent ductus arteriosus pathology is characterized by a persistent connection between the aorta and the pulmonary artery leading to a left-to-right shunt.
How does Patent Ductus Arteriosus Present?
Patent ductus arteriosus is one of the common congenital heart defects that is diagnosed in infants or detected in adulthood. It may present as exercise intolerance and pulmonary congestion with murmur. In infants, it typically presents as tachypnea, diaphoresis, feeding difficulties, and weight loss or gain. In adults, it presents as arrhythmia and cyanosis limited to the lower extremities.
How is Patent Ductus Arteriosus Diagnosed?
Patent ductus arteriosus is diagnosed with physical exam, electrocardiogram, chest x-ray, and 2D echo (gold standard).
How is Patent Ductus Arteriosus Treated?
Patent ductus arteriosus usually closes spontaneously, IV indomethacin can aid in closure of the ductus if given 10-14 days after birth. Closure using catheter and surgical ligation may be performed.
What is the Prognosis of Patent Ductus Arteriosus?
Patent ductus arteriosus prognosis is excellent with patients experiencing no symptoms after closure.
What is a Ventricular Septal Defect?
Ventricular septal defect is characterized by a hole between the right and left ventricles. Degree of symptom severity is dependent on the size of the defect: small, moderate, and large.
What is the Pathology of Ventricular Septal Defect?
Ventricular septal defect pathology is characterized by a hole in the interventricular symptom causing a left-to-right shunt.
How does Ventricular Septal Defect Present?
Ventricular septal defect can present as excessive sweating and increased sympathetic tone in infants, noted during feeding. Fatigue with feeding is usually noted. There is lack of adequate growth and frequent respiratory infections. A diastolic murmur due to aortic insufficiency is a classic finding.
How is Ventricular Septal Defect Diagnosed?
Ventricular septal defect is diagnosed with chest x-ray, MRI, and electrocardiogram. 2D echo is the imaging of choice.
How is Ventricular Septal Defect Treated?
Ventricular septal defect treatment is symptomatic, with large septal defects repaired as young as 6-12 months old. Increase in caloric intake is suggested, and medications such as diuretics, ACE inhibitors, and digoxin may be used.
What is the Prognosis of Ventricular Septal Defect?
Ventricular septal defect prognosis is good, with condition improvement after infancy, and after-repair mortality of less than 1%.
What are Right-to-Left Shunts?
Right-to-left shunts are abnormal connections between the systemic and pulmonary vessels that cause deoxygenated blood to bypass pulmonary circulation and return to the body.
Examples of right-to-left shunts include:
- Tetralogy of fallot
- Transposition of the great arteries
What is Tetralogy of Fallot?
Tetralogy of fallot is one of the most common congenital heart problems that consist of heart defects that impede normal blood flow in the heart.
What is the Pathology of Tetralogy of Fallot?
Tetralogy of fallot consists of ventricular septal defect, pulmonary stenosis, a misplaced aorta, and right ventricular hypertrophy.
How does Tetralogy of Fallot Present?
Tetralogy of fallot is the most common cyanotic congenital heart disease. It presents as failure to thrive in infants, with cyanosis if it occurs with pulmonary atresia. Tet spells may be observed in infants in which their skin turns blue when they feed or cry.
How is Tetralogy of Fallot Diagnosed?
Tetralogy of fallot is diagnosed with laboratory studies such as CBC, coagulation studies, arterial blood gas and blood cultures. For imaging, the following may be utilized: chest x-ray (boot-shaped heart), 2D echo and MRI. Squatting in older children produces a compensatory mechanism that increases peripheral vascular resistance and reduces the extent of right-to-left shunt.
How is Tetralogy of Fallot Treated?
Tetralogy of fallot treatment is mostly surgical with pulmonary valve replacement most commonly performed in adults.
What is the Prognosis of Tetralogy of Fallot?
Tetralogy of fallot prognosis is excellent with treatment, but for the untreated, mortality rate is at 50% by the age of 6 years old.
What is Transposition of the Great Arteries?
Transposition of the great arteries is a defect where the main pulmonary artery and the aorta’s position are switched. It is the most common cyanotic congenital defect in neonates.
What is the Pathology of Transposition of the Great Arteries?
Transposition of the great arteries results in a parallel blood circulation wherein oxygenated blood is pumped back to the lungs, and deoxygenated blood is pumped back to the body resulting in deficient oxygen supply in tissues and ventricular overload.
How does Transposition of the Great Arteries Present?
Transposition of the great arteries presents as cyanosis hours after birth. Presentation differs depending on the extent of defect: with intact ventricular septum, a progressive central cyanosis is note; with large ventricular septal defect, cyanosis becomes more prominent with crying; with ventricular septal defect and left ventricular outflow tract obstruction, presentation is the same as in tetralogy of fallot, and with ventricular septal defect and pulmonary vascular obstructive disease, there is progressive obstructive disease with a loud S2 sound.
How is Transposition of the Great Arteries Diagnosed?
Transposition of the great arteries is diagnosed with abnormal pulse oximetry findings in upper and lower extremity, hyperoxia, ABG, cardiac catheterization, chest x-ray, 2D echo, and MRI.
How is Transposition of the Great Arteries Treated?
Transposition of the great arteries treatment is to maintain ductal patency for inter circulatory mixing of blood flow with IV prostaglandin. Cardiac catheterization, balloon atrial septostomy, and mechanical ventilation may be utilized.
What is the Prognosis of Transposition of the Great Arteries?
Transposition of the great arteries prognosis is good with 90% survival after treatment.
What are Obstructive Lesions of the Heart?
Obstructive lesions of the heart are a common congenital heart disease that causes impedance to the blood flow in the left heart chamber and left ventricular outflow.
Examples of obstructive lesions of the heart include:
- Aortic atresia
- Aortic stenosis
- Coarctation of the aorta
- Pulmonary atresia
- Pulmonary stenosis
What is Aortic Atresia?
Aortic atresia is a rare congenital heart defect where the connection of the left ventricle to the aorta is blocked, affecting the flow of blood from the left ventricle to the body.
What is the Pathology of Aortic Atresia?
Aortic atresia pathology is characterized by congenital fusion of aortic cusps that can be subvalvular, valvular, or supra-valvular in location.
How does Aortic Atresia Present?
Aortic atresia presents as a murmur, cyanosis, rapid or difficulty breathing, irritability, low energy, and clammy skin.
How is Aortic Atresia Diagnosed?
Aortic atresia diagnosis is based on chest x-ray, 2D echo, electrocardiogram, cardiac catheterization and MRI.
How is Aortic Atresia Treated?
Aortic atresia treatment involves giving IV prostaglandin to keep the ductus arteriosus open for an alternative blood flow. Cardiac catheterization and balloon atrial septostomy may also be done.
What is the Prognosis of Aortic Atresia?
Aortic atresia prognosis is poor with incidence of more than 8 in 1000 live births, a serious defect that can lead to mortality without immediate intervention.
What is Aortic Stenosis?
Aortic stenosis is the narrowing of the aortic valve, reducing or blocking blood flow from the heart to the body.
What is the Pathology of Aortic Stenosis?
Aortic stenosis pathology includes narrowing of the aortic valve in the valvular, subvalvular, or supra-valvular area that may be due to a fibrous ring or membrane.
How Does Aortic Stenosis Present?
Aortic stenosis is more common in males and asymptomatic in children with mild to moderate aortic stenosis. Severe aortic stenosis may present as chest pain with exertion, low exercise tolerance, and syncope.
How is Aortic Stenosis Diagnosed?
Aortic stenosis diagnosis includes electrocardiogram, chest x-ray, serum electrolyte levels, cardiac biomarkers, and CBC. 2D echo confirms diagnosis.
How is Aortic Stenosis Treated?
Aortic stenosis treatment includes IV prostaglandin to maintain an open ductus arteriosus for an alternative blood flow. Mild to moderate aortic stenosis only requires supportive management; severe cases are treated with balloon valvuloplasty.
What is the Prognosis of Aortic Stenosis?
Aortic stenosis prognosis is excellent for the asymptomatic with less than 1% mortality per year; however, patients with severe aortic stenosis have a poor prognosis with 40% mortality in all patients.
What is Coarctation of the Aorta?
Coarctation of the aorta is a congenital defect that is characterized by a narrowed portion of the aorta which may be isolated or in association with other heart defects such as a bicuspid aortic valve and ventricular septal defect.
What is the Pathology of Coarctation of the Aorta?
Coarctation of the aorta pathology consists of a constricted aortic segment that affects thickening of the medial aspect of the vessel. The constriction is mostly located in the thoracic aorta.
How does Coarctation of the Aorta Present?
Coarctation of the aorta with upper extremity hypertension or decreased lower extremity blood flow. It is characterized by weak, delayed, or absent femoral pulses and a systolic pressure in the lower extremity that is lower than in the upper extremity by >10 mmHg. A heave is commonly palpated.
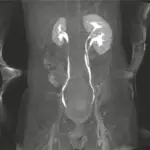
How is Coarctation of the Aorta Diagnosed?
Coarctation of the aorta is diagnosed with septic workup, ABG, electrocardiogram, chest x-ray (inverted E or 3 sign), 2D echo, and MRI.
How is Coarctation of the Aorta Treated?
Coarctation of the aorta is treated with angioplasty at 18-24 months old; however, presence of hypertension may necessitate earlier repair. An IV prostaglandin may be given to maintain ductus arteriosus open for alternative blood flow.
What is the Prognosis of Coarctation of the Aorta?
Coarctation of the aorta prognosis is poor with high mortality following surgical repair, and a mortality of 90% in patients with uncorrected defects by the mean age of 35 years old.
What is Pulmonary Atresia?
Pulmonary atresia is a congenital defect that is characterized by absence of a pulmonary valve responsible for the regulation of blood flow from the heart to the lungs.
What is the Pathology of Pulmonary Atresia?
Pulmonary atresia pathology is characterized by the non-formation of the pulmonary valve, preventing blood from going to the lungs for oxygenation.
How does Pulmonary Atresia Present?
Pulmonary atresia is a critical congenital defect that necessitates intervention soon after birth; features of the condition include cyanosis, poor feeding, sleepiness, and difficulty breathing.
How is Pulmonary Atresia Diagnosed?
Pulmonary atresia is diagnosed through physical exam, 2D echo, cardiac catheterization and electrocardiogram.
How is Pulmonary Atresia Treated?
Pulmonary atresia treatment includes maintaining opening of ductus arteriosus for alternative blood flow, use of cardiac catheterization, and surgery for pulmonary valve repair of replacement.
What is the Prognosis of Pulmonary Atresia?
Pulmonary atresia prognosis is good for treated patients with no significant limitations, however, the untreated patients have a mortality rate of 50% at 1 year old.
What is Pulmonary Stenosis?
Pulmonary stenosis is narrowing of the pulmonary valve located between the right ventricle and the pulmonary artery.
What is the Pathology of Pulmonary Stenosis?
Pulmonary stenosis is characterized by a dome shaped pulmonary valve with thickened and stiff leaflets.
How does Pulmonary Stenosis Present?
Pulmonary stenosis presents as exertional dyspnea and fatigue in patients with severe type; as well as a prominent wave and a precordial heave along the left parasternal border.
How is Pulmonary Stenosis Diagnosed?
Pulmonary stenosis is diagnosed with chest x-ray (prominent pulmonary arteries), 2D echo, cardiac catheterization, electrocardiogram, and MRI.
How is Pulmonary Stenosis Treated?
Pulmonary stenosis treatment includes percutaneous balloon valvuloplasty and beta blockers.
What is the Prognosis of Pulmonary Stenosis?
Pulmonary stenosis prognosis is excellent with long term course of the disease not different from the normal population.
What is Ischemic Heart Disease?
Ischemic heart disease is also called coronary heart disease; a heart condition caused by narrowed heart arteries affecting the oxygen supply of heart muscles.
Examples of ischemic heart disease include:
- Angina pectoris
- Chronic ischemic heart disease
- Myocardial infarction
What is Angina Pectoris?
Angina pectoris is caused by ischemia due to the imbalance of blood supply and oxygen demand. Angina pectoris is a common presenting symptom in patients with coronary artery disease.
What is the Pathology of Angina Pectoris?
Angina pectoris pathology is due to oxygen deprived heart muscles, resulting in accumulation of waste products that irritate local nerve endings leading to pain.
How does Angina Pectoris Present?
Angina pectoris presents as retrosternal chest pain or discomfort which is often felt as pressure, heaviness, squeezing, burning, or choking. Pain is often localized in the epigastrium, back, neck, jaw, or shoulders, and is precipitated by exertion, eating, cold temperatures, or emotional stress that lasts 1-5 minutes relieved by rest. Pain is not influenced by respiration, position, or cough.
How is Angina Pectoris Diagnosed?
Underlying cause of angina pectoris may be diagnosed through chest x-ray, stress test, electrocardiogram, and coronary angiography.
How is Angina Pectoris Treated?
Angina pectoris treatment includes lifestyle changes, treatment of risk factors, and pharmacologic: sublingual nitroglycerin, beta blockers, calcium channel blockers, and ACE inhibitors.
What is the Prognosis of Angina Pectoris?
Angina pectoris prognosis is dependent on left ventricle function, atherosclerosis location and severity, and response to medical treatment. Left ventricular ejection with reduced ejection fraction has a poor prognosis.
What is Chronic Ischemic Heart Disease?
Chronic ischemic heart disease is a condition of recurring chest pain due to inadequate blood supply to the heart caused by narrowed heart arteries.
What is the Pathology of Chronic Ischemic Heart Disease?
Chronic ischemic heart disease pathology is caused by narrowing of heart arteries.
How does Chronic Ischemic Heart Disease Present?
Chronic ischemic heart disease presents as extreme chest pain and/or shortness of breath. Chronic ischemic heart disease is relieved by medication or rest, radiates to the back, arm or other areas occurring repeatedly. Symptoms usually occur during periods of physical exertion and last <5 minutes.
How is Chronic Ischemic Heart Disease Diagnosed?
Chronic ischemic heart disease is diagnosed with thorough history and physical exam, routine blood test, electrocardiogram and stress test.
How is Chronic Ischemic Heart Disease Treated?
Chronic ischemic heart disease is treated with ACE inhibitors, ARBs, antiplatelet drugs, beta blockers, calcium channel blockers, nitrates, and statins. Surgical procedures can also be performed such as angioplasty, and coronary artery bypass graft.
What is the Prognosis of Chronic Ischemic Heart Disease?
Chronic ischemic heart disease prognosis is dependent on disease progression. Good prognosis is achieved in patients with good control of risk factors and those who received appropriate treatment.
What is Myocardial Infarction?
Myocardial infarction is an irreversible heart muscle death caused by ischemia.
What is the Pathology of Myocardial Infarction?
Myocardial infarction pathology is characterized by death of heart muscle (necrosis) due to blocked arteries.
How does Myocardial Infarction Present?
Myocardial infarction affects millions of Americans annually. Individuals typically present with chest pain that is preceded by fatigue, chest discomfort and malaise. Chest pain is prolonged and continuous for 30-60 minutes with radiation to neck, shoulder, jaws and left arm.
How is Myocardial Infarction Diagnosed?
Myocardial infarction diagnosis include electrocardiogram, cardiac markers, CBC, metabolic panel, and lipid profile. Usual electrocardiogram findings are: ST-segment elevation, presence of new Q waves, ST-segment depression, T wave inversion. And nonspecific ST-T wave abnormalities.
How is Myocardial Infarction Treated?
Myocardial infarction treatment includes restoration of perfusion with percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG). Other pharmacologic management include: statins, aspirin, nitrates, and analgesia.
What is the Prognosis of Myocardial Infarction?
Myocardial infarction prognosis is poor with associated mortality of 30%; and 10% of survivors die after 1 year.
What is Sudden Cardiac Death?
Sudden cardiac death is an unexpected death due to loss of cardiac function within 1 hour of symptom onset.
What is the Pathology of Sudden Cardiac Death?
Sudden cardiac death pathology is associated with coronary artery occlusion, aneurysm, rupture, dissection, spasm, arteritis, and coronary anomalies of vessels.
How does Sudden Cardiac Death Present?
Sudden cardiac death has a prodrome of chest pain, fatigue, palpitations, and other nonspecific complaints.
How is Sudden Cardiac Death Diagnosed?
Sudden cardiac death diagnosis includes laboratory studies of cardiac enzymes, electrolytes, calcium, magnesium, BNP, and inflammation markers. For imaging, 2D echo, chest x-ray, and electrocardiogram are utilized.
How is Sudden Cardiac Death Treated?
Sudden cardiac death is treated with intensive monitoring; resuscitative efforts may be conducted. For drug therapy, beta blockers, and anti-arrhythmic drugs may be given. ICD placement may be used for prevention as well as temporary cardiac pacing, radiofrequency ablation, cardioverter defibrillator therapy and surgery.
What is the Prognosis of Sudden Cardiac Death?
Sudden cardiac death prognosis is poor with >40% unwitnessed deaths each year. Surviving patients have a recurrence rate of 20%.
What is Hypertensive Heart Disease?
Hypertensive heart disease is a heart condition brought about by high blood pressure.
Examples of hypertensive heart disease include:
- Pulmonary hypertensive heart disease
- Systemic hypertensive heart disease
What is Valvular Heart Disease?
Valvular heart disease is a condition wherein the valve of the heart is damaged or has a disease.
Examples of valvular heart disease include:
- Calcific valvular degeneration
- Infective endocarditis
- Mitral valve prolapse
- Rheumatic heart disease
What is Calcific Valvular Degeneration?
Calcific valvular degeneration is a slow and progressive condition that goes from mild valve thickening to severe calcification, impairing leaflet motion.
Examples of calcific valvular degeneration include:
Calcific aortic stenosis
Calcific stenosis of congenitally bicuspid aortic valve
Mitral annular calcification.
What is the Pathology of Calcific Valvular Degeneration?
Calcific valvular degeneration pathology is initiated by focal leaflet thickening with normal valve function, progressing to thickening of the valve leaflets, formation of calcium nodules, formation of new blood vessels, and formation of nodular calcified masses within aortic cusps, eventually interfering with its opening and function; commonly affecting aortic valve.
How does Calcific Valvular Degeneration Present?
Calcific valvular degeneration presents in 30% of elderly >65 years old. Hallmark features include early atherosclerosis, cell proliferation and osteoblast expression.
How is Calcific Valvular Degeneration Diagnosed?
Calcific valvular degeneration diagnosis is done through 2D echo.
How is Calcific Valvular Degeneration Treated?
Calcific valvular degeneration is treated with surgical replacement.
What is the Prognosis of Calcific Valvular Degeneration?
Calcific valvular degeneration prognosis is moderate with 50% risk of the disease to cause cardiovascular related events. And 80% mortality over 5 years from diagnosis.
What is Infective Endocarditis?
Infective endocarditis is an infection of the inner lining of the heart, valves, and great vessels.
What is the Pathology of Endocarditis?
Infective endocarditis pathology is characterized by the presence of aggregates made up of platelets, fibrin, microorganism, inflammatory cells and leaflet disruption. This is caused by bacteria, fungi and viruses.
How does Infective Endocarditis Present?
Infective endocarditis presents with nonspecific symptoms with mostly constitutional complaints such as fever and chills, anorexia, weight loss, malaise, headache, myalgias, night sweats, SOB, cough, and joint pains.
How is Infective Endocarditis Diagnosed?
Infective endocarditis diagnosis includes blood culture, blood work, 2D echo, ultrasound and chest x-ray.
How is Infective Endocarditis Treated?
Infective endocarditis is treated with IV antibiotics, anticoagulation therapy and surgery.
What is the Prognosis of Infective Endocarditis?
Infective endocarditis prognosis is moderate with cure rates ranging from 40%-99% depending on the offending organism involved.
What is Mitral Valve Prolapse?
Mitral valve prolapse is a condition wherein the flaps of the valve are not closing properly due to thickening of the leaflets forming an upward bulge into the left atrium.
What is the Pathology of Mitral Valve Prolapse?
Mitral valve prolapse pathology is due to thickened and myxomatous leaflets of the mitral valve with an elongated chordae tendineae.
How does Mitral Valve Prolapse Present?
Mitral valve prolapse affects 2-3% of the population and is usually benign that presents with fatigue, dyspnea, exercise intolerance, orthopnea, paroxysmal nocturnal dyspnea, progressive signs of CHF, and palpitations.
How is Mitral Valve Prolapse Diagnosed?
Mitral valve prolapse is diagnosed with 2D echo showing >2mm superior displacement of mitral leaflets into the left atrium during systole with thickness of less than or at least 5mm. Other findings include leaflet thickening, redundancy, annular dilatation, and chorda elongation.
How is Mitral Valve Prolapse Treated?
Mitral valve prolapse treatment is surgery for those with severe regurgitation. For the asymptomatic patients no treatment is required.
What is the Prognosis of Mitral Valve Prolapse?
Mitral valve prolapse prognosis is excellent with most of the patients being asymptomatic and only 5-10% progressing to severe regurgitation.
What is Rheumatic Heart Disease?
Rheumatic heart disease is an inflammatory disease that follows an S. pyogenes infection.
What is the Pathology of Rheumatic Heart Disease?
Rheumatic heart disease pathology involves the cardiac valves, commonly affecting the mitral valve causing leaflet thickening and fibrosis leading to stenosis or regurgitation. Thrombotic vegetation is seen in acute phases while in chronic, fused commissures, valve thickening and calcification is observed.
How does Rheumatic Heart Disease Present?
Rheumatic heart disease presentation involves the heart, joints, CNS, subcutaneous and skin. Fever, swollen joints, nodules, rashes, chest discomfort, and weakness may be noted.
How is Rheumatic Heart Disease Diagnosed?
Rheumatic heart disease is diagnosed with 2D echo, electrocardiogram, chest x-ray, MRI and blood tests.
How is Rheumatic Heart Disease Treated?
Rheumatic heart disease treatment includes preventing the disease by properly treating strep infections. Treatment of advanced damage is surgical repair/replacement of the affected valve.
What is the Prognosis of Rheumatic Heart Disease?
The prognosis of rheumatic heart disease is poor due to possible progression after repair.
What are Cardiomyopathies?
Cardiomyopathies are heart diseases affecting the cardiac musculature, affecting its pumping function.
Examples of cardiomyopathies include:
- Arrhythmogenic right ventricular cardiomyopathy
- Dilated cardiomyopathy
- Hypertrophic cardiomyopathy
- Restrictive cardiomyopathy
What is Arrhythmogenic Right Ventricular Cardiomyopathy?
Arrhythmogenic right ventricular cardiomyopathy is a hereditary disorder characterized by structural and functional abnormalities in the right ventricle causing ventricular arrhythmia.
What is the Pathology of Arrhythmogenic Right Ventricular Cardiomyopathy?
Arrhythmogenic right ventricular cardiomyopathy pathology consists of myocardial atrophy of the right ventricle with transmural fatty replacement resulting in electrical instability.
Arrhythmogenic Right Ventricular Cardiomyopathy?
Arrhythmogenic right ventricular cardiomyopathy is an important cause of sudden cardiac death in 11% of young adults. It presents as palpitation, syncope, sudden cardiac death, atypical chest pain, and dyspnea.
How is Arrhythmogenic Right Ventricular Cardiomyopathy Diagnosed?
Arrhythmogenic right ventricular cardiomyopathy diagnosis consists of electrocardiogram (inverted T-waves, epsilon waves), 2D echo, and 24-hr holter monitoring.
How is Arrhythmogenic Right Ventricular Cardiomyopathy Treated?
Arrhythmogenic right ventricular cardiomyopathy treatment consists of lifestyle changes, pharmacologic therapy, catheter-based ablation, placement of an implantable cardioverter-defibrillator (ICD), and heart transplantation.
What is the Prognosis of Arrhythmogenic Right Ventricular Cardiomyopathy?
Arrhythmogenic right ventricular cardiomyopathy prognosis is poor with mortality of 22% in young adult athletes. Poorer prognosis is seen in patients with left ventricular involvement.
What is Dilated Cardiomyopathy?
Dilated cardiomyopathy is a condition that involves the muscle in the left ventricle wherein it stretches and thins out, leading to inadequate pumping of the blood.
What is the Pathology of Dilated Cardiomyopathy?
Dilated cardiomyopathy pathology is an idiopathic process that characterizes an enlarged ventricle with normal wall thickness.
How does Dilated Cardiomyopathy Present?
Dilated cardiomyopathy has a prevalence of 1 in 2,500 and presents with fatigue, dyspnea on exertion, orthopnea, edema, weight or increasing abdominal girth. Tachypnea, tachycardia, and hyper/hypotension is noted, as well as jugular venous distension, pulmonary edema, and s3 gallop.
How is Dilated Cardiomyopathy Diagnosed?
Dilated cardiomyopathy diagnosis include CBC, thyroid function test, cardiac markers, chest x-ray, electrocardiogram, 2D echo, and cardiac catheterization.
How is Dilated Cardiomyopathy Treated?
Dilated cardiomyopathy treatment include use of ACE inhibitors, ARBs, beta blockers, diuretics, nitrates, vasodilators, left ventricular assist device, biventricular pacing, automatic cardioverter-defibrillator, and heart transplantation.
What is the Prognosis of Dilated Cardiomyopathy?
Dilated cardiomyopathy prognosis is poor with most of the patients progressing to heart failure.
What is Hypertrophic Cardiomyopathy?
Hypertrophic cardiomyopathy is a genetic disease characterized by an increase in the left ventricular wall thickness.
What is the Pathology of Hypertrophic Cardiomyopathy?
Hypertrophic cardiomyopathy pathology is due to mutation of cardiac sarcomere protein genes transmitted in an autosomal dominant trait.
How does Hypertrophic Cardiomyopathy Present?
Hypertrophic cardiomyopathy presents as dyspnea, syncope, presyncope, angina, palpitations, orthopnea, paroxysmal nocturnal dyspnea, congestive heart failure, dizziness, and sudden cardiac death.
How is Hypertrophic Cardiomyopathy Diagnosed?
Hypertrophic cardiomyopathy diagnosis include 2D echo, routine laboratory tests and genetic testing.
How is Hypertrophic Cardiomyopathy Treated?
Hypertrophic cardiomyopathy treatment includes beta blockers, calcium channel blockers, and antitussives. Surgery, alcohol ablation or pacing is also conducted.
What is the Prognosis of Hypertrophic Cardiomyopathy?
Hypertrophic cardiomyopathy prognosis is good with an annual mortality of only <1%-6%.
What is Restrictive Cardiomyopathy?
Restrictive cardiomyopathy is a rare condition characterized by restrictive ventricular function, diastolic dysfunction but with normal systolic activity.
What is the Pathology of Restrictive Cardiomyopathy?
Restrictive cardiomyopathy pathology is characterized by mutation in the sarcomeric proteins which increases cardiac myofilaments sensitivity to calcium leading to diastolic dysfunction. Biatrial dilatation, abnormal ventricular wall with rubbery texture, and thickening of the endocardium are observed.
How does Restrictive Cardiomyopathy Present?
Restrictive cardiomyopathy presents as worsening shortness of breath, exercise intolerance, orthopnea, fatigue, and paroxysmal dyspnea. It is rare and accounts for only 5% of all cardiomyopathies.
How is Restrictive Cardiomyopathy Diagnosed?
Restrictive cardiomyopathy diagnosis includes chest x-ray (atrial dilatation), 2D echo (non-dilated ventricles with dilation of both atria), catheterization, cardiac biopsy (abnormal myocardium).
How is Restrictive Cardiomyopathy Treated?
Restrictive cardiomyopathy treatment is non-specific and highly based on causation. Corticosteroids, endocardectomy, phlebotomy and chelation, and chemotherapy may be utilized. Pharmacologic treatment is symptomatic.
What is the Prognosis of Restrictive Cardiomyopathy?
Restrictive cardiomyopathy prognosis is poor with 2-year mortality of 50% and 5-year mortality of 70% after diagnosis.
What is Pericardial Disease?
Pericardial disease is inflammation in the layers of the pericardium.
Examples of pericardial disease include:
- Pericarditis
- Pericardial effusion
- Hemopericardium
What is Pericarditis?
Pericarditis is inflammation of the pericardium.
What is the Pathology of Pericarditis?
Pericarditis pathology is characterized by infiltration of polymorphonuclear leukocytes and pericardial vascularization. Manifestation of fibrinous reaction with exudates and adhesion is frequently noted.
How does Pericarditis Present?
Pericarditis presents as chest pain that is precordial/retrosternal that radiates to trapezius ridge, neck, shoulder, or arm. It is a pleuritic pain that is worse on inspiration, when lying flat, or with movement and relieved when leaning forward or with sitting. Associated features include fever, dyspnea, cough, dysphagia and weight loss.
How is Pericarditis Diagnosed?
Pericarditis diagnosis include electrocardiogram, echocardiography and chest x-ray, as well as inflammation and cardiac markers.
How is Pericarditis Treated?
Pericarditis treatment is symptomatic and based on causation. Pain relievers, colchicine, corticosteroids are used. For bacterial infection, antibiotics and drainage is used. Surgery may also be performed such as pericardiocentesis and pericardiectomy.
What is the Prognosis of Pericarditis?
Pericarditis prognosis is good with most post-myocardial infarction cases having a benign course.
What is Pericardial Effusion?
Pericardial effusion is an abnormal fluid accumulation in the pericardial space.
What is the Pathology of Pericardial Effusion?
Pericardial effusion pathology is characterized by fluid buildup in the pericardial space that may be serious with fibrin strands, serosanguineous fluid, blood, pus, or chyle, that may eventually lead to cardiac tamponade.
How does Pericardial Effusion Present?
Pericardial effusion presents as chest discomfort, light-headedness, palpitations, cough, dyspnea, hoarseness and hiccups.
How is Pericardial Effusion Diagnosed?
Pericardial effusion diagnosis includes echocardiography and electrocardiogram.
How is Pericardial Effusion Treated?
Pericardial effusion treatment includes pericardiocentesis, pericardiostomy, and use of aspirin, colchicine, steroids, and antibiotics.
What is the Prognosis of Pericardial Effusion?
Pericardial effusion prognosis is good, however poor prognosis is attributed to fever >38C, traumatic cause, unresponsive to NSAIDs, and in patients on anticoagulants.
What is Hemopericardium?
Hemopericardium is the presence of blood in the pericardial space.
What is the Pathology of Hemopericardium?
Hemopericardium pathology is due to ruptured secondary to myocardial infarction or left ventricular aneurysm, aortic dissection, pericarditis, trauma, ruptured coronary aneurysm, and post-thrombolysis.
How does Hemopericardium Present?
Hemopericardium presents as difficulty breathing, fatigue, rapid breathing, chest pressure, and elevated heart rate.
How is Hemopericardium Diagnosed?
Hemopericardium diagnosis include echocardiography, chest x-ray, jugular vein distention and pulsus paradoxus.
How is Hemopericardium Treated?
Hemopericardium treatment is pericardiocentesis
What is the Prognosis of Hemopericardium?
Hemopericardium prognosis is poor with 13.3% leading to mortality without prompt treatment.
What Heart Diseases are Associated with Rheumatologic Disorders?
Heart diseases associated with rheumatologic disorders are manifestations of rheumatologic disease that can range from subclinical to severe manifestations. These are due to autoimmune inflammatory conditions that can cause morbidity and mortality in patients causing manifestations such as myocardial, valvular, pericardial, and conduction system abnormalities.
Examples of heart diseases associated with rheumatologic disorders include:
- Ankylosing spondylitis
- Psoriatic arthritis
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Systemic sclerosis
What are Tumors of the Heart?
Tumors of the heart are growth of abnormal tissues in the heart that are classified as either primary or secondary, and malignant or benign.
Primary tumors of the heart include:
- Cardiac lipoma
- Cardiac myxoma
- Cardiac papillary fibroelastoma
- Cardiac sarcoma
What is a Cardiac Lipoma?
Cardiac lipoma is an encapsulated, benign, primary cardiac tumor considered to be the most common non-myxomatous cardiac tumor.
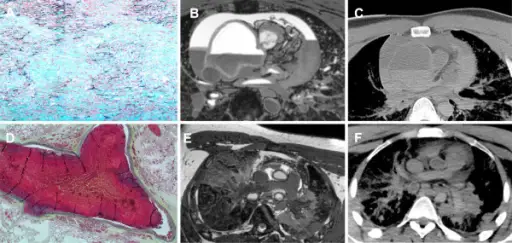
What is the Pathology of Cardiac Lipoma?
The pathology of cardiac lipoma is:
-Etiology: The cause of cardiac lipoma is unknown, however, association with gene rearrangement is seen.
-Genes involved: chromosome 12 gene rearrangement, HMGA2-LPP fusion.
-Pathogenesis: The sequence of events that lead to cardiac lipoma is not understood but to progression of the tumor may be silent for a long period of time and may grow in size without infiltrating the myocardium. It may result in myocardium resorption and cavitation that may involve the cardiac chambers.
-Histology: The histology associated with cardiac lipoma shows mature fat cells within the collagenous capsule.
How does Cardiac Lipoma Present?
Patients with cardiac lipoma have no sex or age predilection. The symptoms, features, and clinical findings associated with cardiac lipoma include dyspnea, syncope, arrhythmia, palpitations, and angina.
How is Cardiac Lipoma Diagnosed?
Cardiac lipoma is diagnosed in echocardiography showing a cardiac mass. CT and MRI are good modalities to show tissue characteristics; coronary arteriography can aid the operating surgeon in outlining blood supply and coronary anatomy.
How is Cardiac Lipoma Treated?
Cardiac lipoma is treated through surgical excision of the tumor. However, treatment is not warranted in asymptomatic individuals.
What is the Prognosis of Cardiac Lipoma?
The prognosis of cardiac lipoma is good with patients not usually needing treatment or surgical intervention, but if needed, resection can be done easily followed with excellent patient recovery.
What is a Cardiac Myxoma?
Cardiac myxoma is the most common primary heart tumor.
What is the Pathology of Cardiac Myxoma?
The pathology of cardiac myxoma is:
-Etiology: The cause of cardiac myxoma is sporadic with unknown exact cause.
-Genes involved: Abnormality with the short arm of chromosome 2 and chromosome are associated with 7% of all cardiac myxoma cases.
-Pathogenesis: The sequence of events that lead to cardiac myxoma are attributed to a mixture of environmental and genetic factors. It can occur spontaneously with no definite underlying cause.
-Histology: The histology associated with cardiac myxoma shows lepidic cells within the myxoid stroma with structures resembling cords or rings around the blood vessels accompanied by presence of inflammatory cells and hemorrhage with hemosiderin deposits.
How does Cardiac Myxoma Present?
Patients with cardiac myxoma typically affect females more than males and present at the age range of 3-83 years old. The symptoms, features, and clinical findings associated with cardiac myxoma include dyspnea on exertion, fatigue peripheral edema, dizziness/ syncope, and pulmonary edema.
How is Cardiac Myxoma Diagnosed?
Cardiac myxoma is diagnosed depending on its location and size. Generally, a thorough history and physical exam is essential. Blood test, electrocardiogram, chest x-ray, CT scan/ MRI, Echocardiography can be utilized.
How is Cardiac Myxoma Treated?
Cardiac myxoma is treated by removing the tumor.
What is the Prognosis of Cardiac Myxoma?
The prognosis of cardiac myxoma is good due to its benign process, however, 15% of patients with the disease died due to sudden cardiac death.
What is a Cardiac Papillary Fibroelastoma?
Cardiac papillary fibroelastoma is the second most common cardiac tumor.
What is the Pathology of Cardiac Papillary Fibroelastoma?
The pathology of cardiac papillary fibroelastoma is:
-Etiology: The cause of cardiac papillary fibroelastoma is unknown, due to its rare occurrence.
-Pathogenesis: The sequence of events that lead to cardiac papillary fibroelastoma is hypothesized to be acquired and begin as a microthrombi which aggregates at minor endothelial damages on the valvular surface. The microthrombi becomes excrescences and then papillary fibroelastoma that can potentially lead to sudden death, stroke, and myocardial infarction.
-Histology: The histology associated with cardiac papillary fibroelastoma shows a sea-anemone like structure with a central stalk and arms projecting outward composed of collagen, elastin, and reticulin.
How does Cardiac Papillary Fibroelastoma Present?
Patients with cardiac papillary fibroelastoma typically affect male with <1% prevalence and present at a mean age of 60 years old. The symptoms, features, and clinical findings associated with cardiac papillary fibroelastoma is generally asymptomatic but can include stroke, myocardial infarction, features of heart failure, syncope or sudden death.
How is Cardiac Papillary Fibroelastoma Diagnosed?
Cardiac papillary fibroelastoma is diagnosed with an incidental finding; initial approach is with transthoracic echocardiography, transesophageal echocardiogram or during cardiac surgery and autopsy.
How is Cardiac Papillary Fibroelastoma Treated?
Cardiac papillary fibroelastoma treatment includes surgery and close monitoring.
What is the Prognosis of Cardiac Papillary Fibroelastoma?
The prognosis of cardiac papillary fibroelastoma is good following surgical procedure due to its benign process.
What is a Cardiac Sarcoma?
Cardiac sarcoma is a malignant cardiac tumor that is also the most common malignant tumor of the heart.
What is the Pathology of Cardiac Sarcoma?
The pathology of cardiac sarcoma is:
-Etiology: The cause of cardiac sarcoma is an abnormal cell division regulation that is caused by immune system irregularities that is associated with previous radiotherapy treatment.
-Genes involved: p53 gene.
-Pathogenesis: The sequence of events that lead to cardiac sarcoma is ana;yzed to be due to numerical and structural chromosomal changes that arise as a mural mass in the right atrium, eventually affecting adjacent structures.
-Histology: The histology associated with cardiac sarcoma shows collapsed, complex anastomosing vascular channels lined with flat/tufted bland endothelial cells.
How does Cardiac Sarcoma Present?
Patients with cardiac sarcoma typically affect male with a prevalence of 0.2% and present at any age. The symptoms, features, and clinical findings associated with cardiac sarcoma include dyspnea, chest pain, hemoptysis, diminished cardiac sounds, friction rub, rales, arrhythmia, heart block and heart failure.
How is Cardiac Sarcoma Diagnosed?
Cardiac sarcoma is diagnosed with echocardiography, CT scan/MRI, and angiography for assessment of arteries. Chest x-ray may show cardiomegaly, pulmonary congestion/ effusion, and hilar adenopathy.
How is Cardiac Sarcoma Treated?
Cardiac sarcoma is treated with surgical excision and radiotherapy with/without chemotherapy. .
What is the Prognosis of Cardiac Sarcoma?
The prognosis of cardiac sarcoma is poor with postoperative survival of 17 months and 6 months for those without treatment.
What are Metastatic Cancers to the Heart?
Metastatic cancers to the heart are malignancies that originate from other organs, but travel to the heart and develop there. Note that cardiac and noncardiac neoplasms may affect the heart by altering conduction leading to conduction abnormalities, causing emboli, or causing obstruction.