Chronic pancreatitis is a condition pancreas characterized by inflammation with irreversible destruction of exocrine parenchyma, and in the late stages, the destruction of endocrine parenchyma.
What is the Pathology of Chronic Pancreatitis?
The pathology of chronic pancreatitis is:
-Etiology: The cause of chronic pancreatitis is long-term alcohol abuse, long-standing obstruction, hereditary pancreatitis, and idiopathic chronic pancreatitis.
-Genes involved: PRSS1 gene.
-Pathogenesis: The sequence of events that lead to chronic pancreatitis is not well defined, and may involve ductal obstruction, toxins, oxidative stress, and necrosis. The inflammation of the pancreas, may present as repeated bouts of acute pancreatitis, the main distinction to acute pancreatitis is the irreversible impairment in the pancreatic function that is characteristic of chronic pancreatitis.
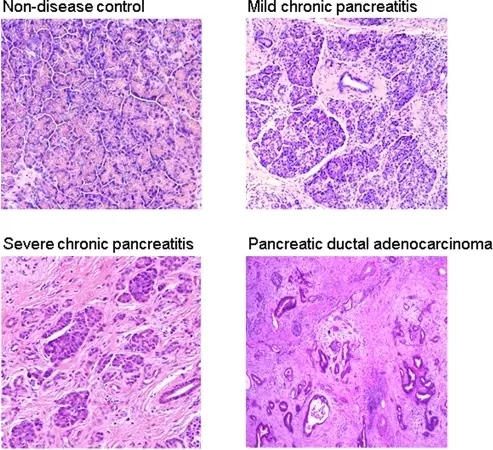
-Histology: The histology associated with chronic pancreatitis shows parenchymal fibrosis, reduced number, and size of acini. There may be relative sparing of the islets of Langerhans.
How does Chronic Pancreatitis Present?
Patients with chronic pancreatitis are typically common in males than females present at an age range of 35 to 45years. The symptoms, features, and clinical findings associated with chronic pancreatitis include moderately severe abdominal pain, back pain, jaundice.
How is Chronic Pancreatitis Diagnosed?
Chronic pancreatitis is diagnosed through the clinical presentation, ultrasonography, CT scan- evidence of calcifications.
How is Chronic Pancreatitis Treated?
Chronic pancreatitis is treated through medical care, analgesics, fluid management.
What is the Prognosis of Chronic Pancreatitis?
The prognosis of chronic pancreatitis is poor with a 20 to 25 year mortality rate of 50%.