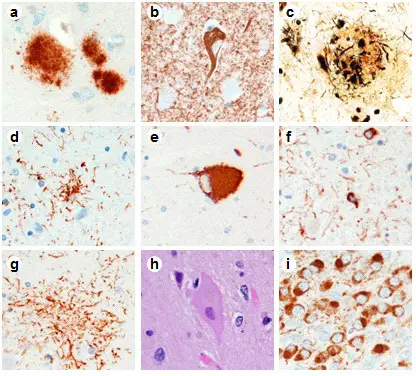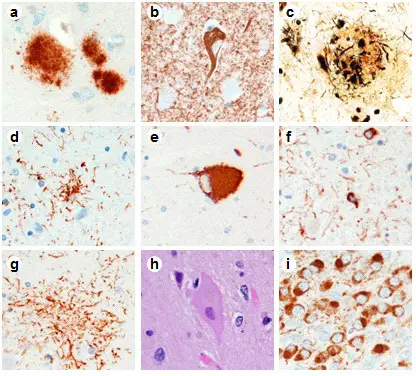
Neuropathologic inclusions seen in tauopathies range from intracellular to extracellular and from neuron to glia. Alzheimer’s disease neuropathologic inclusions used to classify severity based on an ABC scoring scheme include (a) extracellular amyloid-beta (Aβ) plaque (33.1.1 antibody), (b) neurofibrillary tangle (NFT) composed of abnormal tau fibrils (paired helical filament phosphorylated tau antibody), and (c) Aβ deposits surrounded by dystrophic neurites produce neuritic plaques (observed with Bielschowsky silver stain). Tau immunohistochemistry in progressive supranuclear palsy shows abnormal tau aggregates in (d) astrocytes called tufts or tufted astrocytes, (e) neurons called globose NFTs, and (f) oligodendrocytes termed coiled bodies. Tau-immunoreactivity in corticobasal degeneration (CBD) shows abnormal tau aggregates in (g) astrocytes called astrocytic plaques and tau-immunoreactive threads in the gray and white matter in neocortical and subcortical regions and (h) swollen, achromatic or ballooned neurons (hematoxylin and eosin). (i) Tau-immunoreactive, dense spherical neuronal cytoplasmic inclusions called Pick bodies are observed in granular neurons of the dentate fascia in Pick’s disease. (a), (b), (c) Medial temporal cortex. (d), (e), (f),(g), (i) Phospho-tau antibody CP13. (d), (f) Red nucleus at the level of the oculomotor nerve. (e) Substantia nigra. (g), (h)
Mid-frontal cortex.Clinicopathologic assessment and imaging of tauopathies in neurodegenerative dementias.
Murray ME, Kouri N, Lin WL, Jack CR, Dickson DW, Vemuri P - Alzheimer's research & therapy (2014). Not Altered. CC.
Corticobasal degeneration is a progressive neurological disorder characterized by nerve cell loss and atrophy of multiple areas of the brain including the cerebral cortex and the basal ganglia.
What is the Pathology of Corticobasal Degeneration?
Etiology: The exact, underlying cause of corticobasal degeneration is unknown.
Pathogenesis: Progressive deterioration of tissue in different parts of the brain.
Histology: The histology associated with corticobasal degeneration shows presence of neuronal cytoplasmic inclusions.
How does Corticobasal Degeneration Present?
Patients with corticobasal degeneration typically occurs in age range 50-70 years and affects more females than males. The symptoms, features, and clinical findings associated with Corticobasal degeneration include progressive asymmetric rigidity, pain, apraxia, bradykinesia, dystonia, and myoclonus.
How is Corticobasal Degeneration Diagnosed?
Corticobasal degeneration is diagnosed based on signs and symptoms.
How is Corticobasal Degeneration Treated?
There are no treatments that help slow the progression of corticobasal degeneration.
What is the Prognosis of Corticobasal Degeneration?
The prognosis of Corticobasal degeneration is poor, and the disease progresses over time.