Cushing syndrome is due to an excessive amount of cortisol.
What is the Pathology of Cushing Syndrome?
The pathology of Cushing syndrome is:
-Etiology: The cause of Cushing syndrome is glucocorticoid overproduction. This may be due to an ACTH-producing pituitary adenoma or hyperplasia, adrenal adenoma, adrenal carcinoma, or bilateral adrenal hyperplasia, or ectopic ACTH production by non-adrenal neoplasm.
-Pathogenesis: The sequence of events that lead to Cushing syndrome involves ACTH stimulation of the adrenal gland that results in secretion of cortisol and other steroid hormones.
-Morphology: The morphology associated with Cushing syndrome shows that the enlarged adrenal glands.
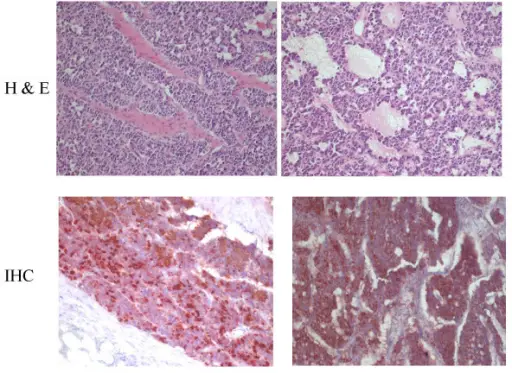
-Histology: The histology associated with zona glomerulosa is difficult to identify in adults, and fasciculata has lipid-depleted cells and reticularis cells are vacuolated.
How does Cushing Syndrome Present?
Patients with Cushing syndrome may be male or female, and they are usually middle aged. The symptoms, features, and clinical findings associated with Cushing syndrome include weight gain, truncal obesity, abdominal striae, hypertension, buffalo hump, and glucose intolerance.
How is Cushing Syndrome Diagnosed?
Cushing syndrome is diagnosed with a 24-hour urine collection with analysis for urinary-free cortisol excretion. Low-dose and high-dose dexamethasone suppression tests, corticotropin assays, corticotropin-releasing hormone stimulation tests, and inferior petrosal sinus catheterization may be required for a definitive diagnosis.
How is Cushing Syndrome Treated?
Cushing syndrome is treated with surgical resection or radiation of pituitary tumor, and surgical or medical (with mitotane) adrenalectomy for small ACTH-producing pituitary adenoma, or hyperplasia.
What is the Prognosis of Cushing Syndrome?
The prognosis of Cushing syndrome is fair. Patients who have been surgically treated for Cushing’s disease require careful long-term follow-up and monitoring for signs and symptoms of tumor recurrence. The pituitary-adrenal axis must be evaluated six to 12 months after surgery to determine the potential need for lifetime exogenous steroid replacement therapy.