Cystitis glandularis is a proliferative disorder of the urinary bladder in which there is glandular metaplasia of the transitional cells lining the urinary bladder.
What is the Pathology of Cystitis Glandularis?
The pathology of cystitis glandularis is:
-Etiology: The cause of cystitis glandularis is chronic bladder outlet obstruction, pelvic lipomatosis, benign prostatic hypertrophy, bladder transitional/urothelial cell carcinoma.
-Genes involved: CCND1, CCNA1, EGFR, AR, CX3CL1, CXCL6, and CXCL1.
-Pathogenesis: The sequence of events that lead to Cystitis glandularis result in metaplasia of the urothelium, which proliferates into buds, which grow down into the connective tissue beneath the epithelium in the lamina propria.
-Morphology: The morphology associated with cystitis glandularis shows lobulated outline of the urinary bladder with a nodular filling defect within.
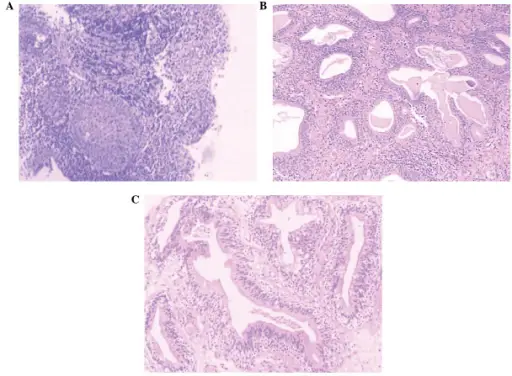
-Histology: The histology associated with cystitis glandularis shows abundant urothelial von Brunn nests.
How does Cystitis Glandularis Present?
Patients with cystitis glandularis typically affect both males and females at all years of age. The symptoms, features, and clinical findings associated with cystitis glandularis include renal colic and abdominal pain; a few patients with a shorter course of the disease also had nausea, vomiting, frequency, urgency, dysuria, hematuria, and fever.
How is Cystitis Glandularis Diagnosed?
Cystitis glandularis is diagnosed by cystoscopy in ureteroscopic surgery.
How is Cystitis Glandularis Treated?
Cystitis glandularis is treated by removing the source of irritation and surgical excision of the area of inflammation or cystectomy in rare severe cases.
What is the Prognosis of Cystitis Glandularis?
The prognosis of cystitis glandularis is variable.