Gallbladder pathology are diseases or disorders involving the gallbladder.
What are Congenital Anomalies of the Gallbladder?
Congenital anomalies of the gallbladder are rare, difficult to diagnose with imaging studies, and can be accompanied by other malformations of the biliary or vascular tree.
Examples of congenital anomalies of the gallbladder include:
- Absent gallbladder
- Duplication of the gallbladder
- Longitudinal septum of the gallbladder
- Transverse septum of the gallbladder
- Phrygian cap of the gallbladder
- True biliary atresia
What is Absent Gallbladder?
Absent gallbladder is the developmental abnormality of the gallbladder and it’s relatively rare.
What is the Pathology of Absent Gallbladder?
The pathology of the absent gallbladder is: a rare congenital anomaly characterized by the absence of the gallbladder in conjunction with a normal bile duct system. It’s often associated with other congenital abnormalities (12.8–30 %) and with gastrointestinal, cardiovascular, genitourinary, and skeletal malformations, such as duodenal atresia, malrotation of the gut, pancreas divisum, imperforate anus, hypoplasia of the right hepatic lobe, duplication cysts of the hepatic flexure, ventricular septal defect, renal agenesis, undescended testes, and syndactyly.
-Etiology: The cause of absent gallbladder is, most often, sporadic and there’s the possible existence of hereditary forms. It has been reported that it’s associated with congenital syndromes, trisomy 18, and with congenital malformations caused by thalidomide.
-Pathogenesis: The sequence of events that lead to an absent gallbladder is that it results from failure of the cystic bud to develop in utero.
-Morphology: The morphology associated with the absent gallbladder is an absence of the gallbladder. It’s almost always an incidental finding of the abdominal surgery or a finding at autopsy and it has a lower incidence in surgical cholecystectomy series (0.007–0.027 %) than in the autopsy reports (0.04–0.13 %). The prevalence range is 0.007–0.13 %.
How does Absent Gallbladder Present?
Patients with absent gallbladder typically are either male or female present at the age range of both children and adults, with a median age of 46 years. The symptoms, features, and clinical findings associated with absent gallbladder include that although often asymptomatic, the agenesis of the gallbladder can present symptoms, such as dyspepsia, abdominal pain, nausea, and vomiting, or intolerance to fatty foods, and it’s been reported to be associated with gastrointestinal, cardiovascular, genitourinary, and skeletal malformations. Clinically, three groups of presentation of gallbladder agenesis have been described: asymptomatic (an incidental finding at laparotomy for another reason- 35 %; symptomatic- 50 %; in children with multiple fetal anomalies (such as tetralogy of Fallot and agenesis of the lungs), and in children who die in the perinatal period (15–16 %). Common symptoms include: right upper quadrant abdominal pain (90 %), nausea and vomiting (66 %), fatty food intolerance (37 %), dyspepsia (30 %), and jaundice (35 %).
How is Absent Gallbladder Diagnosed?
Absent gallbladder is diagnosed during laparoscopic cholecystectomy. Combined with the rarity of the condition, the diagnosis is infrequently made preoperatively, and so the patient undergoes unnecessary operative intervention. Intraoperatively, the risk of iatrogenic injury is higher, and so the associated morbidity of the procedure is greater. The usual initial investigation for patients presenting right upper quadrant pain is an abdominal ultrasound. It has been suggested that the absence of the ultrasonographic features of the WES triad (visualization of the gallbladder wall, the echo of the stone, and the acoustic shadow) and the double-arc shadow should raise suspicion of gallbladder agenesis as the diagnosis. Pre-operative MRCP should be considered in cases in which ultrasound suggests non-visualization of the gallbladder, and surgeons should maintain a low threshold for further investigation before any decision to operate.
How is Absent Gallbladder Treated?
Absent gallbladder is treated with conservative surgery, medications, or making lifestyle changes to help manage the symptoms. Some of the lifestyle changes that can help ease digestive symptoms are: adopting a low-fat diet, avoiding eating fatty foods, such as fried foods, eating small, frequent meals, and avoiding eating a very large dinner after fasting all day.
What is the Prognosis of Absent Gallbladder?
The prognosis of the absent gallbladder is good. Patients without a gallbladder are usually operated, because of a “false” interpretation of ultrasound imaging.
What is Duplication of the Gallbladder?
Duplication of the gallbladder is a rare congenital malformation that occurs in about one in 4000 births.
What is the Pathology of Duplication of the Gallbladder?
The pathology of duplication of the gallbladder is:
-Etiology: The cause of duplication of the gallbladder is associated with an increased risk of complications after laparoscopic cholecystectomy. It can’t be accurately assessed, since the only cases which have been identified are those that became symptomatic or were encountered as incidental findings during surgery, imaging studies, or at autopsy.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to duplication of the gallbladder is that it occurs when either the cystic primordium splits during the fifth to sixth weeks of embryogenesis to give a duplicate gallbladder or when there’s extra budding of the biliary primordium to give rise to an accessory gallbladder.
-Morphology: The morphology associated with duplication of the gallbladder shows two chambers with a single cystic duct that communicate through a common ostium and there’re two cystic arteries as well.
How does Duplication of the Gallbladder Present?
Patients with duplication of the gallbladder typically are either male or female present at the age range of older than 65 years. The symptoms, features, and clinical findings associated with duplication of the gallbladder include acute or chronic cholecystitis, cholelithiasis, empyema, torsion, cholecystocolic fistula, and carcinoma. There are no specific symptoms attributable to it. Duplication of the gallbladder can be classified into 2 main types. The first is the bi-lobed gallbladder where a longitudinal septum or invaginating cleft separates the lumen into 2 chambers and both gallbladders share a common embryological origin (primordium). The second is the double gallbladder where there’re 2 separate gallbladders with their cystic ducts and a double embryological origin (dual primordium).
How is Duplication of the Gallbladder Diagnosed?
Duplication of the gallbladder is diagnosed by preoperative imaging. If the intraoperative anatomy isn’t clear then an intra-operative cholangiogram should be performed.
How is Duplication of the Gallbladder Treated?
Duplication of the gallbladder is treated by laparoscopic cholecystectomy with intraoperative cholangiography in the symptomatic gallbladder and the removal of an asymptomatic double gallbladder remains controversial. Sometimes there’s the need for complete removal of both gallbladders during the initial surgery, as a failure of this may result in recurrence of symptoms, stones, and a need for re-exploration.
What is the Prognosis of Duplication of the Gallbladder?
The prognosis of duplication of the gallbladder is good and the simultaneous removal of both gallbladders at surgery is recommended to avoid cholecystitis and biliary colic in the remaining organ.
What is Longitudinal Septum of the Gallbladder?
Longitudinal septum of the gallbladder is the septum which is dividing the gallbladder longitudinally and it’s called the bilobed gallbladder.
What is the Pathology of Longitudinal Septum of the Gallbladder?
The pathology of the longitudinal septum of the gallbladder is:
-Etiology: The cause of the longitudinal septum of the gallbladder isn’t clear.
-Pathogenesis: The sequence of events that lead to the longitudinal septum of the gallbladder
-Morphology: The morphology associated with the longitudinal septum of the gallbladder shows the two distinct anatomical configurations of the bilobed gallbladder. The first is that in which the body of the organ is completely or partially separated into two lobes by a deep cleft, resulting in a Y- or T-shaped viscus and the second form has a single fundus, divided into paired mucosal compartments by a longitudinal septum. In either instance, the lobes may be of the same or unequal sizes.
How does Longitudinal Septum of the Gallbladder Present?
Patients with the longitudinal septum of the gallbladder typically are male present at the age range of all age groups. The symptoms, features, and clinical findings associated with the longitudinal septum of the gallbladder include that this malformation is represented by a structure having two separate fundic cavities, united at their bases and joined to the ductus choledochus by a single cystic duct. It’s differentiated from the double, or accessory gallbladder, called vesica fellea duplex, by the presence of independent cystic ducts, draining the individual fundic cavities of the latter type.
How is Longitudinal Septum of the Gallbladder Diagnosed?
Longitudinal septum of the gallbladder is diagnosed with a preoperative diagnosis which is important to avoid preoperative complications, however, it’s also a challenge as imaging reports are often confounding.
How is the Longitudinal Septum of the Gallbladder Treated?
Longitudinal septum of the gallbladder is treated with laparoscopic cholecystectomy which is minimally invasive surgery to remove the gallbladder. It helps people when gallstones cause inflammation, pain, or infection, the surgery involves a few small incisions, and most people go home the same day and soon return to normal activities.
What is the Prognosis of Longitudinal Septum of the Gallbladder?
The prognosis of the longitudinal septum of the gallbladder is good. The postoperative patient is treated with standard intravenous antibiotics. Usually, the postoperative day 1 diet is starting, and the patient is discharged on postoperative day 2 in stable condition.
What is Transverse Septum of the Gallbladder?
Transverse septum of the gallbladder is a stricture that divides the gallbladder into two cavities joined by a canal.
What is the Pathology of Transverse Septum of the Gallbladder?
The pathology of the transverse septum of the gallbladder is:
-Etiology: The cause of the transverse septum of the gallbladder is probably similar to a congenital septum.
-Pathogenesis: The sequence of events that lead to the transverse septum of the gallbladder is a result of adenomyomatosis of the gallbladder when it’s segmental in nature.
-Morphology: The morphology associated with the transverse septum of the gallbladder shows a thin septum covered by epithelium.
How does Transverse Septum of the Gallbladder Present?
Patients with the transverse septum of the gallbladder typically are male present at the age range of all age groups. The symptoms, features, and clinical findings associated with the transverse septum of the gallbladder include the occurrence of adenomyomatosis in the distal cavity, in most cases, and sometimes there’re strictures less than 12 mm in diameter and rarely it’s completely calculus-free. Rokitansky Aschoff sinuses are present in gallbladders with an acquired septum.
How is Transverse Septum of the Gallbladder Diagnosed?
Transverse septum of the gallbladder is diagnosed through X-ray and ultrasound. Where a case suggestive of cholelithiasis is encountered, the cholecystogram should be examined very carefully even if no stones are seen and repeat examinations should be performed if symptoms persist.
How is Transverse Septum of the Gallbladder Treated?
Transverse septum of the gallbladder is treated with laparotomy and cholecystectomy when symptoms are severe in association with the deformity. It’s possible that the use of cholecystokinin in reproducing symptoms can help to make a positive pre-operative diagnosis. The patients should undergo an exploratory laparotomy and cholecystectomy without stones being present only in a few cases in which the surgery is performed to relieve them of their symptoms.
What is the Prognosis of Transverse Septum of the Gallbladder?
The prognosis of the transverse septum of the gallbladder is good. It’s now possible to demonstrate the gallbladder septum through an ultrasonic examination which makes the diagnosis simpler.
What is Phrygian Cap of the Gallbladder?
Phrygian cap of the gallbladder is a triangular deformity of the gallbladder fundus and a fairly common anatomical variant.
What is Pathology of Phrygian Cap of the Gallbladder?
The pathology of the Phrygian cap of the gallbladder is:
-Etiology: The cause of the Phrygian cap of the gallbladder is a fold in the gallbladder where the gallbladder fundus joins the gallbladder body.
-Pathogenesis: The sequence of events that lead to a Phrygian cap of the gallbladder is that a gallbladder has shrunk in size, can’t be visible on an imaging test and this can prevent a gallbladder from properly functioning.
-Morphology: The morphology associated with the Phrygian cap of the gallbladder shows the folded portion of some gallbladders that resembles the Phrygian cap (a soft conical cap with the top pulled forward, associated in antiquity with the inhabitants of Phrygia, a region of central Anatolia).
How does Phrygian Cap of the Gallbladder Present?
Patients with Phrygian cap of the gallbladder typically are either male or female present at the age range of all age groups. The symptoms, features, and clinical findings associated with the Phrygian cap of the gallbladder include that it’s a benign anatomical abnormality and normally causes no symptoms. Sometimes patients complain of pain in the right upper quadrant of the abdomen. A Phrygian cap is a congenital abnormality of the gallbladder and it has an incidence of 4 %. Phrygian cap is the most common congenital anomaly of the gallbladder and it can simulate a mass in the liver during hepatobiliary imaging which may suggest a tumor. Also, it can simulate a duplication of the gallbladder. Apart from the chance of being mistaken for stones on a sonogram, it has no other medical implications nor does it predispose one to other diseases.
How is Phrygian Cap of the Gallbladder Diagnosed?
Phrygian cap of the gallbladder is diagnosed with ultrasonography, CT scan, oral cholecystography, cholescintigraphy, and multiphase MRI. CT and ultrasonography are not always conclusive and radiographic imaging can help narrow the differential diagnosis. The multiphase MRI or multiphase CT in case of MRI contraindication is nowadays the first choice of hepatobiliary imaging.
How is Phrygian Cap of the Gallbladder Treated?
Phrygian cap of the gallbladder is treated with prophylactic cholecystectomy only in case of symptoms or for other reasons, such as wedge resection of the liver. Due to a potential decrease in bile flow, it may warrant a preventive removal of the gallbladder.
What is the Prognosis of Phrygian Cap of the Gallbladder?
The prognosis of the Phrygian cap of the gallbladder is good.
What is True Biliary Atresia?
True biliary atresia is a blockage in the tubes (ducts) that carry bile from the liver to the gallbladder.
What is the Pathology of True Biliary Atresia?
The pathology of true biliary atresia is:
-Etiology: The cause of true biliary atresia is the bile ducts inside or outside the liver that aren’t developed normally. The biliary atresia can be caused by a defect in the normal remodeling process and the genetic predisposition has also been proposed as a factor for its development.
-Genes involved: INVS, ZIC3, AGXT, GPC1, XPNPEP1, ADD3, JAG1, MYO5B, ABCC2, ABCB11, UG1A1, MLL2, RFX6, ERCC4, and KCNH1.
-Pathogenesis: The sequence of events that lead to true biliary atresia is an obliterative fibrosing cholangiopathy of the intrahepatic and extrahepatic bile ducts. It’s the most common indication for liver transplantation during childhood. Viral infection initiates biliary epithelium destruction and release of antigens that trigger a Th1 immune response, which leads to further injury of the bile duct, resulting in inflammation and obstructive scarring of the biliary tree.
-Morphology: The morphology associated with true biliary atresia may show vauge abdominal symptoms.
-Histology: The histology associated with true biliary atresia shows the expansion of the portal tracts, with edematous fibroplasia and bile ductular proliferation, with bile plugs in duct lumen. Variable multinucleate giant cells, bilirubinostasis, and hemopoiesis may also be seen.
How does True Biliary Atresia Present?
Patients with true biliary atresia typically are female (slightly more frequent) at the age range of two to six weeks. The symptoms, features, and clinical findings associated with true biliary atresia include a yellowish coloration of the skin and whites of the eyes (jaundice), abnormally pale stools, swollen (distended) stomach, and abnormal enlargement of the liver (hepatomegaly). The clinical presentation is characterized by direct or conjugated hyperbilirubinemia, acholic stool, dark urine, variable levels of hepatosplenomegaly, and progressive hepatic failure. If untreated affected infants develop rapidly progressing fibrosis leading to portal hypertension and end-stage liver disease invariably resulting in death within the first 2 years of life. Therefore, early diagnosis is critical so that surgical intervention can remove the atretic extrahepatic biliary tree in an attempt to re-establish the biliary flow to the intestine by creating a Rouxen-Y intestinal conduit.
How is True Biliary Atresia Diagnosed?
True biliary atresia is diagnosed with ultrasonography, biochemical liver function tests, viral serology, and a percutaneous liver biopsy. Sometimes, duodenal intubation and measurement of intraluminal bile is the routine test for BA and the newer modalities, such as ERCP(37) and MRCP, have been used at times.
How is True Biliary Atresia Treated?
True biliary atresia is treated with Kasai portoenterostomy (KPE) in which a Roux-en-Y anastomosis is connected to the hepatic end of the divided extravascular portal structures, including the rudimentary bile ducts. Even after successful surgery, most patients are likely to show progressive liver dysfunction.
What is the Prognosis of True Biliary Atresia?
The prognosis of true biliary atresia is fair. Poor outcomes have been associated with late diagnosis and delayed KPE, presence of associated extrahepatic anomalies, portoenterostomy performed by laparoscopic method, failure to achieve jaundice clearance in 3 months post-KPE, and repeated cholangitis.
What is Cholelithiasis?
Cholelithiasis is caused by excessive amounts of cholesterol in the bile that’s stored in the gallbladder and this cholesterol hardens to form stone-like substances.
Examples of cholelithiasis are:
- Gallstones
- Cholesterol stones
- Pigment stones
What are Gallstones?
Gallstones are concretions that form in the biliary tract, usually in the gallbladder.
What is the Pathology of Gallstones?
The pathology of gallstones is:
-Etiology: The cause of gallstones isn’t completely understood, but it’s thought to have multiple risk factors. It’s the decreased degradation of mucin by lysosomal enzymes that are believed to promote the formation of cholesterol crystals. Also, loss of gallbladder muscular-wall motility and excessive sphincteric contraction are involved in gallstone formation.
-Pathogenesis: The sequence of events that lead to gallstones is that the gallbladder stores bile and releases it into the small intestine when it’s needed for digestion. Gallstones can develop if the bile contains too much cholesterol or too much bilirubin, or if the gallbladder is dysfunctional and can’t release the bile. The hypomotility leads to prolonged bile stasis (delayed gallbladder emptying), along with decreased reservoir function and the lack of bile flow causes an accumulation of bile and an increased predisposition for stone formation.
-Morphology: The morphology associated with gallstones shows a cholesterol stone that results from the presence of too much cholesterol in the bile and another type of stone, a pigment stone, is formed from excess bilirubin. The size and number of gallstones vary in cholelithiasis and the gallbladder can form many small stones or one large stone.
-Histology: The histology associated with gallstones shows diverse histopathological changes in gallbladder mucosa, namely acute inflammation, chronic inflammation, granulomatous inflammation, hyperplasia, cholesterolosis, dysplasia, and carcinoma.
How do Gallstones Present?
Patients with gallstones typically are female present at the age range of 30-50 years. The symptoms, features, and clinical findings associated with gallstones include irritation and inflammation of the gallbladder (cholecystitis) that can result in several symptoms that can vary in intensity among individuals. The gallstones are generally asymptomatic and in the uncommon event that a patient develops symptomatic cholelithiasis presentation can range from mild nausea or abdominal discomfort to biliary colic and jaundice.
How are Gallstones Diagnosed?
Gallstones are diagnosed via several different imaging techniques and the CBC, liver-function testing, and serum amylase and lipase should be included in the laboratory tests to help discriminate between the various types of gallbladder disease and identify complications caused by gallbladder disease. Ultrasonography and cholescintigraphy are the imaging studies most commonly used to diagnose cholelithiasis and cholecystitis. The current techniques for diagnosing gallbladder disease are less invasive and allow patients to recover more quickly than was the case with earlier diagnostic procedures.
How are Gallstones Treated?
Gallstones are treated with laparoscopic cholecystectomy for symptomatic cholelithiasis and patients experiencing asymptomatic cholelithiasis don’t require treatment. In patients who are unable or unwilling to undergo surgery, endoscopic decompression by internal gallbladder stent can help prevent complications from developing and can serve as a palliative long-term treatment. Nonoperative therapy, which includes dissolution of gallstones using oral bile acids and shock wave lithotripsy can be another option in such patients.
What is the Prognosis of Gallstones?
The prognosis of gallstones is good.
What are Cholesterol Stones?
Cholesterol stones are formed when the bile is supersaturated with cholesterol, which may result from decreased bile acid production, increased cholesterol output in bile, or both.
What is the Pathology of Cholesterol Stones?
The pathology of cholesterol stones is:
-Etiology: The cause of cholesterol stones is often associated with inflammation (cholecystitis). Cholesterol stone formation is promoted by conditions that increase hepatic cholesterol excretion, such as oral contraceptives, pregnancy, anticholesterol medications, rapid weight loss, obesity, hypertriglyceridemia, and conditions that induce gallbladder stasis, or by conditions that deplete bile salts (e.g. Crohn disease).
-Pathogenesis: The sequence of events that lead to cholesterol stones is that they’re formed when the bile is supersaturated with cholesterol. Stone formation by cholesterol monohydrate crystals is enhanced by mucin hypersecretion and gallbladder hypomotility.
-Morphology: The morphology associated with cholesterol stones shows that they’re usually yellow-green and are made of mostly hardened cholesterol, usually < 2 cm, multiple, and round or faceted. Cholesterol stones form within the gallbladder and are frequently multiple, ranging in size from approximately 2 to 25 mm in diameter.
-Histology: The histology associated with cholesterol stones shows that they contain more than 50 % cholesterol. They frequently have a brownish core, with a variety of substances found there, including calcium salts and the glycoproteins and calcium salts (calcium bilirubinate, calcium hydroxyapatite, and calcium carbonate) form around the core, resulting in the layered appearance.
How do Cholesterol Stones Present?
Patients with cholesterol stones typically are female present at the age range of adult age groups. The symptoms, features, and clinical findings associated with cholesterol stones include that their incidence increases with age. They occur in two forms:
Pure cholesterol stones are typically large, solitary, spherical, and hard, with a yellow crystalline internal structure.
Mixed cholesterol stones, which are the majority of cholesterol stones found clinically, are composed predominantly of cholesterol, but also contain variable amounts of bilirubin and calcium salts, multiple.
How are Cholesterol Stones Diagnosed?
Cholesterol stones are diagnosed with abdominal ultrasound.
How are Cholesterol Stones Treated?
Cholesterol stones may be treated with medications, such as ursodiol works to break up small cholesterol stones. Cholecystectomy may also be useful.
What is the Prognosis of Cholesterol Stones?
The prognosis of cholesterol stones is good.
What are Pigment Stones?
Pigment stones are a type of gallbladder stone that is dark in color, made of bilirubin, and can be subclassified into brown and black types, which differ in morphology, pathogenesis, and clinical associations.
What is the Pathology of Pigment Stones?
The pathology of pigment stones is:
-Etiology: The cause of pigment stones is often associated with inflammation (cholecystitis). Black pigment stones can occur in persons with no predisposing conditions, but important risk factors associated with it include chronic hemolysis (e.g., sickle cell disease), thalassemia, prosthetic cardiac valves, advancing age, and cirrhosis.
-Pathogenesis: The sequence of events that lead to pigment stones has to do with after glucuronidation in the liver bilirubin is secreted into bile. Because mixed cholesterol and pigment stones contain salts of calcium and bilirubin, deconjugation and precipitation of bilirubin are essential in pathogenesis. Also, the gallbladder stasis must be present for precipitates of calcium bilirubinate to form.
-Morphology: The morphology associated with pigment stones shows that black pigment stones are 2-5 mm, shiny, irregular, and multifaceted and the brown pigment stones have a softer texture and flaky appearance, often larger than black stones
-Histology: The histology associated with pigment stones shows proliferation of connective tissue and loss of elastic fibers, cellular infiltration of lymphocytes and polymorphonuclear leukocytes, and atrophic dilatation or hyperplasic glandular changes.
How does Pigment Stones Present?
Patients with pigment stones typically are female present at the age range of reproductive years. The symptoms, features, and clinical findings associated with pigment stones include that black pigment stones seldom coexist with cholesterol stones in the same gallbladder. Symptoms include right upper quadrant pain that may be constant, and intense. Other symptoms include fever, yellowing of skin and whites of the eyes (jaundice), loss of appetite, nausea, clay colored stools, and vomiting.
How are Pigment Stones Diagnosed?
Pigment stones are diagnosed with abdominal ultrasound. Other imaging tests that may help diagnose pigment stones include oral cholecystography, a hepatobiliary iminodiacetic acid (HIDA) scan, computerized tomography (CT), magnetic resonance cholangiopancreatography (MRCP), or endoscopic retrograde cholangiopancreatography (ERCP). Blood tests can reveal infection, jaundice, pancreatitis, or other complications caused by gallstones.
How are Pigment Stones Treated?
Pigment stones are treated with surgery to remove the gallbladder, or medications to dissolve the stones.
What is the Prognosis of Pigment Stones?
The prognosis of pigment stones is good.
What is Cholecystitis?
Cholecystitis is inflammation of the gallbladder wall.
Examples of cholecystitis include:
- Acute cholecystitis
- Chronic cholecystitis
What is Acute Cholecystitis?
Acute Cholecystitis is the abrupt destructive process of the gallbladder.
What is the Pathology of Acute Cholecystitis?
The pathology of acute cholecystitis is:
-Etiology: The cause of acute cholecystitis are stones are physically blocking of the cystic duct. Acute cholecystitis also has other causes, such as ischemia, chemicals that enter biliary secretions, motility disorders associated with drugs, infections with microorganisms, protozoa, parasites, collagen disease, and allergic reactions. Acute acalculous cholecystitis can also be associated with a recent operation, trauma, burns, multisystem organ failure, and parenteral nutrition.
-Pathogenesis: The sequence of events that lead to acute calculous cholecystitis is the blockage of the neck or cystic duct typically by gallstones or biliary sludge, increased pressure within the gallbladder, venous stasis, arterial stasis, gallbladder ischemia, and necrosis. The sequence of events that lead to acute acalculous cholecystitis is the bile stasis and ischemia that isn’t provoked by a physical blockade of cystic duct or ischemia due to activated factor XII, no collateral blood supply, and complete reliance on the cystic artery.
-Morphology: The morphology associated with acute cholecystitis shows gallbladder wall thickening and pericholecystic fluid seen on transabdominal ultrasound and complications, such as perforation, that is seen most often in acalculous cholecystitis.
-Histology: The histology associated with acute cholecystitis shows the erosion of mucosa, edema, myofibroblasts, lymphocytes, plasma cells, eosinophils, pigment-laden macrophages, and fibrin. Acute inflammatory cells can’t be seen unless there’s a secondary bacterial infection or choledocholithiasis.
How does Acute Cholecystitis Present?
Patients with acute cholecystitis typically are female present at the age range of over 30 years old. The symptoms, features, and clinical findings associated with acute cholecystitis include classic symptoms, such as right upper quadrant pain, nausea, vomiting, anorexia, and fever. There’s the distention or edema of the gallbladder, the serosa is hemorrhagic, there’s an exudate and color alteration. The wall is thickened up to 2 cm, edematous, and hemorrhagic. In the mucosa, ulcers can be seen and there’re choleliths in the neck or cystic duct. In the lumen bile, hemorrhage, the fluid mixture of cholesterol, and calcium carbonate can be seen.
How is Acute Cholecystitis Diagnosed?
Acute cholecystitis is diagnosed with a combination of history, physical, laboratory, and imaging findings. The imaging findings include transabdominal ultrasound and cholescintigraphy.
How is Acute Cholecystitis Treated?
Acute cholecystitis is treated with antibiotics, and cholecystectomy.
What is the Prognosis of Acute Cholecystitis?
The prognosis of acute cholecystitis is fair.
What is Chronic Cholecystitis?
Chronic cholecystitis is the chronic inflammation of the gallbladder, typically secondary to gallstones and cholelithiasis. The two forms of chronic cholecystitis are calculous (occurring in the setting of cholelithiasis), and acalculous (without gallstones), however, most cases of chronic cholecystitis are commonly associated with cholelithiasis.
What is the Pathology of Chronic Cholecystitis?
The pathology of chronic cholecystitis is:
-Etiology: The cause of chronic cholecystitis is cholelithiasis, though the severity of the disease poorly correlates with stone burden and the risk factors correspond to those that increase the risk of cholelithiasis: female sex, obesity, rapid weight loss, pregnancy, and advanced age.
-Pathogenesis: The sequence of events that lead to chronic cholecystitis may be due to recurrent acute cholecystitis, cholelithiasis, either through direct mucosal irritation or via intermittent mechanical obstruction with associated alteration of bile chemistry.
-Morphology: The morphology associated with chronic cholecystitis shows gallbladder wall thickening and a gallbladder can appear contracted or distended.
-Histology: The histology associated with chronic cholecystitis shows variable amounts of predominantly mononuclear inflammatory infiltrate in lamina propria, which may extend into the muscular and pericholecystic tissues, hypertrophy of muscularis, variable degrees of mural fibrosis, elastosis, and neural hyperplasia, and accentuation of Rokitansky-Aschoff sinuses (pseudodiverticula).
How does Chronic Cholecystitis Present?
Patients with chronic cholecystitis typically are female present at the age range of from 18 to 50 years-old. The symptoms, features, and clinical findings associated with chronic cholecystitis include Murphy sign or the right upper abdominal pain with deep palpation, abdominal discomfort often related to fatty food ingestion, nausea, vomiting, bloating, and flatulence. Chronic cholecystitis presents as a smoldering course that can be accompanied by acute exacerbations of increased pain (acute biliary colic), or it can progress to a more severe form of cholecystitis requiring urgent intervention (acute cholecystitis). It doesn’t always cause clinical symptoms and can present with dull right upper quadrant pain that radiates to the mid-back or right scapula.
How is Chronic Cholecystitis Diagnosed?
Chronic cholecystitis is diagnosed with abdominal ultrasound, abdominal CT with contrast, or HIDA (hepatobiliary iminodiacetic acid) scan demonstrating a reduced ejection fraction (< 35%).
How is Chronic Cholecystitis Treated?
Chronic cholecystitis is treated with elective cholecystectomy.
What is the Prognosis of Chronic Cholecystitis?
The prognosis of chronic cholecystitis is good and the majority of uncomplicated cases have an excellent outcome. With elective cholecystectomy, bile duct injuries do occur with regular frequency, biliary leakage is reported in up to 3 % of cases, and, generally, there’s a very low risk (< 0.5%) of associated incidental carcinoma.
What is Carcinoma of the Gallbladder?
Carcinoma of the gallbladder is an abnormal growth of cells that begins in the gallbladder. It’s often an incidental finding after cholecystectomy for cholecystitis or cholelithiasis and it isn’t associated with tumor-related death.
Examples of carcinoma of the gallbladder include:
- Adenocarcinoma of the gallbladder
- Squamous cell carcinoma of the gallbladder
- Adenosquamous carcinoma of the gallbladder
- Small cell carcinoma of the gallbladder
- Sarcoma of the gallbladder
- Neuroendocrine tumor of the gallbladder
- Lymphoma of the gallbladder
- Melanoma of the gallbladder
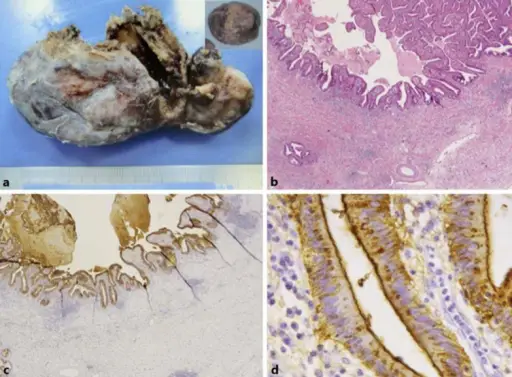
What is Adenocarcinoma of the Gallbladder?
Adenocarcinoma of the Gallbladder is cancer that begins in the glandular cells that line the inner surface of the gallbladder.
What is the Pathology of Adenocarcinoma of the Gallbladder?
The pathology of adenocarcinoma of the gallbladder is:
-Etiology: The cause of adenocarcinoma of the gallbladder isn’t clear. Factors that can increase the risk of gallbladder cancer include a history of gallstones, alcohol use, and gallbladder inflammation.
-Genes involved: K-ras mutations, cancers without expression of p21 but with expression for p27 have a better prognosis, whereas those that express c-erb-B2 have a worse one.
-Pathogenesis: The sequence of events that lead to adenocarcinoma of the gallbladder is that healthy gallbladder cells develop mutations in their DNA. The cells start to grow out of control and to continue living when other cells would normally die and the accumulating cells form a tumor that can grow beyond the gallbladder and spread to other areas of the body. It can arise from either a pathway involving metaplasia or dysplasia or one in which there is a pre-existing adenoma.
-Morphology: The morphology associated with adenocarcinoma of the gallbladder shows thickened and indurated gallbladder wall, exophytic or polypoid friable mucosal lesions.
-Histology: The histology associated with adenocarcinoma of the gallbladder shows malignant glandular proliferation.
How does Adenocarcinoma of the Gallbladder Present?
Patients with adenocarcinoma of the gallbladder typically are female (F: M = 3:1) present at the age range of the sixth and seventh decades. The symptoms, features, and clinical findings associated with adenocarcinoma of the gallbladder include abdominal pain, particularly in the upper right portion of the abdomen, abdominal bloating, weight loss, and jaundice.
How is Adenocarcinoma of the Gallbladder Diagnosed?
Adenocarcinoma of the gallbladder is diagnosed with a physical exam, but gallbladder cancer may not be detectable through a physical exam in the early stages and since the gallbladder is buried deep within the abdomen. Tests that are needed to make the diagnosis are lab tests to determine the level of bilirubin, albumin, alkaline phosphatase, AST, ALT, and GGT, and tumor markers. Other procedures for diagnosis include the CT scan, ultrasound, MRI, X-ray, cholangiography, and biopsy.
How is Adenocarcinoma of the Gallbladder Treated?
Adenocarcinoma of the gallbladder is treated with 1 or more treatments, including surgery, chemotherapy, or radiation therapy.
What is the Prognosis of Adenocarcinoma of the Gallbladder?
The prognosis of adenocarcinoma of the gallbladder is poor and the overall 5-year survival rate is less than 5 %.
What is Squamous Cell Carcinoma of the Gallbladder?
Squamous cell carcinoma of the gallbladder is a rare histopathologic subtype of gallbladder carcinomas.
What is the Pathology of Squamous Cell Carcinoma of the Gallbladder?
The pathology of squamous cell carcinoma of the gallbladder is:
-Etiology: The cause of squamous cell carcinoma of the gallbladder isn’t clear, but there are some known risk factors which include which include age and sex, gallstones and inflammation, family history of gallbladder cancer, smoking, porcelain gallbladder, primary sclerosing cholangitis, and obesity.
-Pathogenesis: The sequence of events that lead to squamous cell carcinoma of the gallbladder is uncertain and usually is thought to develop in response to the irritation resulting in squamous metaplasia.
-Morphology: The morphology associated with squamous cell carcinoma of the gallbladder shows vauge abdminal symptoms.
-Histology: The histology associated with squamous cell carcinoma of the gallbladder shows squamous differentiation without any recognizable invasive glandular component. Squamous cell carcinomas exhibit abundant keratinization with pearl formation, prominent intercellular bridges, and the presence of keratohyaline granules with numerous dyskeratotic cells.
How does Squamous Cell Carcinoma of the Gallbladder Present?
Patients with squamous cell carcinoma of the gallbladder typically are female present at the age range of 50–71 years-old. The symptoms, features, and clinical findings associated with squamous cell carcinoma of the gallbladder include abdominal pain, nausea, vomiting, fever with raised total leucocyte count (TLC), preoperative diagnosis of empyema gall bladder/acute calculous cholecystitis can be made, and gallstones may be seen. Although the patients present at an advanced stage the nodal metastases aren’t common.
How is Squamous Cell Carcinoma of the Gallbladder Diagnosed?
Squamous cell carcinoma of the gallbladder is diagnosed with immunostains, endoscopic retrograde cholangiopancreatography (ERCP), percutaneous cholangiography, laparoscopy, blood tests, computed tomography (CT or CAT) scan, magnetic resonance imaging (MRI), ultrasound, endoscopic ultrasonography, and biopsy.
How is Squamous Cell Carcinoma of the Gallbladder Treated?
Squamous cell carcinoma of the gallbladder is treated with radical resection or with primary tumor resection alone.
What is the Prognosis of Squamous Cell Carcinoma of the Gallbladder?
The prognosis of squamous cell carcinoma of the gallbladder is fair because although it presents at an advanced stage, curative surgical resection of squamous cell carcinoma of the gallbladder might result in disease-free survival rates.
What is Adenosquamous Carcinoma of the Gallbladder?
Adenosquamous carcinoma of the gallbladder is a rare histopathologic subtype that accounts for 1 to 12 % of all gallbladder carcinomas.
What is the Pathology of Adenosquamous Carcinoma of the Gallbladder?
The pathology of adenosquamous carcinoma of the gallbladder is:
-Etiology: The cause of adenosquamous carcinoma of the gallbladder isn’t clear, but there are some known risk factors which include: age and sex, gallstones and inflammation, family history of gallbladder cancer, porcelain gallbladder, primary sclerosing cholangitis, smoking, and obesity.
-Pathogenesis: The sequence of events that lead to adenosquamous carcinoma of the gallbladder is uncertain and usually is thought to originate from preexisting adenocarcinoma by a stepwise molecular progression.
-Morphology: The morphology associated with adenosquamous carcinoma of the gallbladder shows vauge abdominal signs.
-Histology: The histology associated with adenosquamous carcinoma of the gallbladder shows squamous and glandular malignant cells. A significant amount of keratin is observed that is poorly or moderately differentiated. There may be foci of spindle cells, and neuroendocrine and gastric foveolar type of differentiation.
How does Adenosquamous Carcinoma of the Gallbladder Present?
Patients with adenosquamous carcinoma of the gallbladder typically are female. The symptoms, features, and clinical findings associated with adenosquamous carcinoma of the gallbladder include abdominal pain, nausea, vomiting, fever with raised total leucocyte count (TLC).
How is Adenosquamous Carcinoma of the Gallbladder Diagnosed?
Adenosquamous carcinoma of the gallbladder is diagnosed with biopsy, and histologic examination.
How is Adenosquamous Carcinoma of the Gallbladder Treated?
Adenosquamous carcinoma of the gallbladder is treated with surgical resection.
What is the Prognosis of Adenosquamous Carcinoma of the Gallbladder?
The prognosis of adenosquamous carcinoma of the gallbladder is fair because although it presents at an advanced stage, curative surgical resection of adenosquamous carcinoma of the gallbladder may result in disease-free survival rates that are comparable with those of conventional GBC.
What is Small Cell Carcinoma of the Gallbladder?
Small cell carcinoma of the gallbladder is a malignant tumor of the gallbladder.
What is the Pathology of Small Cell Carcinoma of the Gallbladder?
The pathology of small cell carcinoma of the gallbladder is:
-Etiology: The cause of small cell carcinoma of the gallbladder isn’t clear, but there are some known risk factors which include smoking, alcohol use, porcelain gallbladder, primary sclerosing cholangitis, and obesity.
-Pathogenesis: The sequence of events that lead to small cell carcinoma of the gallbladder is that it arises in the setting of chronic inflammation.
-Morphology: The morphology associated with small cell carcinoma of the gallbladder shows a mass lesion with an enlarged lymph node at the hepatic hilum.
-Histology: The histology associated with small cell carcinoma of the gallbladder shows more as pure small round blue cells.
How does Small Cell Carcinoma of the Gallbladder Present?
Patients with small cell carcinoma of the gallbladder typically are female (66 %) present at the age range of 25–86 years (median age: 67 years). The symptoms, features, and clinical findings associated with small cell carcinoma of the gallbladder include abdominal symptoms.
How is Small Cell Carcinoma of the Gallbladder Diagnosed?
Small cell carcinoma of the gallbladder is diagnosed with biopsy.
How is Small Cell Carcinoma of the Gallbladder Treated?
Small cell carcinoma of the gallbladder is treated with chemoradiation and surgical resection.
What is the Prognosis of Small Cell Carcinoma of the Gallbladder?
The prognosis of small cell carcinoma of the gallbladder is poor, the median survival period is nine months.
What is Sarcoma of the Gallbladder?
Sarcoma of the gallbladder is a rare type of gallbladder cancer.
What is the Pathology of Sarcoma of the Gallbladder?
The pathology of sarcoma of the gallbladder is:
-Etiology: The cause of sarcoma of the gallbladder isn’t clear.
-Pathogenesis: The sequence of events that lead to sarcoma of the gallbladder is that it arises in the setting of chronic inflammation.
-Morphology: The morphology associated with sarcoma of the gallbladder shows vauge abdominal symptoms. the mass lesion that is attached to the small bowel and abdominal wall. Leiomyosarcoma typically forms a fleshy mass, with colors varying from grey to white to tan and large examples often display hemorrhage, necrosis, or a cystic change.
-Histology: The histology associated with sarcoma of the gallbladder shows a malignant spindle cell tumor consisting of leiomyosarcoma with marked nuclear atypia and mitosis. The neoplastic cells infiltrate the muscularis propia layers of the small bowel and the soft tissue of the abdominal wall. Intersecting, sharply marginated groups of spindle cells are the typical histopathologic pattern of leiomyosarcoma.
How does Sarcoma of the Gallbladder Present?
Patients with sarcoma of the gallbladder typically are female present at the age range of 50 and 75 years. The symptoms, features, and clinical findings associated with sarcoma of the gallbladder include that it has a very aggressive behavior and is usually diagnosed at advanced stages, therefore, curative surgical management may not be possible. The presence of gallstones is invariable, the symptoms presented are those of chronic cholecystitis and, histopathologically, the majority of these tumors are-high grade and display an epithelioid morphology, but cases with features of well-differentiated leiomyosarcoma have been described.
How is Sarcoma of the Gallbladder Diagnosed?
Sarcoma of the gallbladder is diagnosed on the immunostains, but a diagnosis should be also made on the appropriate morphologic features. In addition to a physical examination, the following tests include biopsy, and endoscopic retrograde cholangiopancreatography (ERCP).
How is Sarcoma of the Gallbladder Treated?
Sarcoma of the gallbladder is treated with a radical cholecystectomy. Chemotherapy may also be needed.
What is the Prognosis of Sarcoma of the Gallbladder?
The prognosis of sarcoma of the gallbladder is poor, the five-year survival rate is less than 5 % and this is because at the time of the diagnosis or surgery almost 75 % of cases involve the liver.
What is Neuroendocrine Tumor of the Gallbladder?
Neuroendocrine tumor of the gallbladder is a unique heterogeneous neoplasm originating from neuroendocrine cells and able to secrete peptides as its neurotransmitter.
What is the Pathology of Neuroendocrine Tumor of the Gallbladder?
The pathology of neuroendocrine tumor of the gallbladder is:
-Etiology: The cause of neuroendocrine tumor of the gallbladder is due to overproduction of neoplastic neuroendocrine cells.
-Genes involved: Epidermal growth factor receptor (EGFR), vascular endothelial growth factor (VEGF), growth factor receptor-bound protein 2 (GRB2).
-Pathogenesis: The sequence of events that lead to a neuroendocrine tumor of the gallbladder is the inflammation that produces neuroendocrine cells at the lesion site eventually leading to its development.
-Morphology: The morphology associated with a neuroendocrine tumor of the gallbladder may show vague abdominal symptoms.
-Histology: The histology associated with a neuroendocrine tumor of the gallbladder shows shows cells that are small, cone-shaped, and polygonal, with no clear cell boundaries. Its cells have small nucleoli, granular chromatin, relatively consistent tumor cell morphology, and are rich in interstitial blood vessels.
How does Neuroendocrine Tumor of the Gallbladder Present?
Patients with neuroendocrine tumor of the gallbladder typically are female. The symptoms, features, and clinical findings associated with a neuroendocrine tumor of the gallbladder include nausea, abdominal distension, and abdominal pain.
How is Neuroendocrine Tumor of the Gallbladder Diagnosed?
Neuroendocrine tumor of the gallbladder is diagnosed with tumor markers and imaging examinations, such as ultrasound, computed tomography (CT). and magnetic resonance imaging (MRI), and biopsy.
How is Neuroendocrine Tumor of the Gallbladder Treated?
Neuroendocrine tumor of the gallbladder is treated with surgery.
What is the Prognosis of Neuroendocrine Tumor of the Gallbladder?
The prognosis of a neuroendocrine tumor of the gallbladder is fair.
What is Lymphoma of the Gallbladder?
Lymphoma of the gallbladder is a rare malignant neoplasm that can mimic carcinoma of the extrahepatic biliary tree.
What is the Pathology of Lymphoma of the Gallbladder?
The pathology of lymphoma of the gallbladder is:
-Etiology: The cause of lymphoma of the gallbladder are low-grade lymphomas of mucosa-associated lymphoid tissue (MALT) which have the propensity to spread.
-Pathogenesis: The sequence of events that lead to a lymphoma of the gallbladder is a diffuse, infiltrating, high-grade malignancy, arising from large B cells, with mainly immunoblastic characteristics.
-Morphology: The morphology associated with lymphoma of the gallbladder a high biliary stricture to involve the confluence of the hepatic ducts with dilatation of the biliary tree.
-Histology: The histology associated with lymphoma of the gallbladder shows a large compact and nodular mass, involving the gallbladder and lymph nodes of the hepatoduodenal ligament en bloc. A gallbladder mass with thickening of the wall, enlarged lymph nodes at the porta hepatis and along the hepatoduodenal ligament, causing extrinsic compression of the common bile duct (CBD), and dilated intrahepatic bile ducts.
How does Lymphoma of the Gallbladder Present?
Patients with lymphoma of the gallbladder typically are female present at the age range of older years. The symptoms, features, and clinical findings associated with lymphoma of the gallbladder include the symptoms of gallstones, or other benign gallbladder diseases, abdominal colic, and dyspepsia.
How is Lymphoma of the Gallbladder Diagnosed?
Lymphoma of the gallbladder is diagnosed by US, CT and magnetic resonance imaging (MRI) scans, ERCP and PTC, laparoscopy, bone-marrow biopsy, gallbladder biopsy, and peripheral blood smear.
How is Lymphoma of the Gallbladder Treated?
Lymphoma of the gallbladder is treated with chemotherapy, with or without radiation therapy.
What is the Prognosis of Lymphoma of the Gallbladder?
The prognosis of lymphoma of the gallbladder is poor and the overall 5-year relative survival rate is 75%.
What is Melanoma of the Gallbladder?
Melanoma of the gallbladder is a rare malignancy of the gallbladder.
What is the Pathology of Melanoma of the Gallbladder?
The pathology of melanoma of the gallbladder is:
-Etiology: The cause of melanoma of the gallbladder are malignant melanocytes impacting the gallbladder.
-Pathogenesis: The sequence of events that lead to melanoma of the gallbladder is a patient with a history of cutaneous malignant melanoma who presents with hepatobiliary symptoms which suggest the diagnosis of a metastatic lesion.
-Morphology: The morphology associated with melanoma of the gallbladder shows the intracholecystic lesions greater than 1 cm without acoustic shadow and distinguish between stones and probable benign small polyps, and gallbladder wall thickening.
-Histology: The histology associated with melanoma of the gallbladder shows malignant melanocytes and pigment.
How does Melanoma of the Gallbladder Present?
Patients with melanoma of the gallbladder typically are male present at the age range of middle-age groups. The symptoms, features, and clinical findings associated with melanoma of the gallbladder include vague abdominal symptoms.
How is Melanoma of the Gallbladder Diagnosed?
Melanoma of the gallbladder is diagnosed with an ultrasound scan of the abdomen and CT, MRI, and Posistron Emission Tomography (PET) scans, and biopsy.
How is Melanoma of the Gallbladder Treated?
Melanoma of the gallbladder is treated with open surgical resection, and potentially chemotherapy.
What is the Prognosis of Melanoma of the Gallbladder?
The prognosis of melanoma of the gallbladder is poor.