Gastrointestinal pathology is the subspecialty of surgical pathology which deals with the diagnosis and characterization of neoplastic and non-neoplastic diseases of the digestive tract and accessory organs, such as the pancreas and liver.
What are Congenital Abnormalities of the Gastrointestinal Tract?
Congenital abnormalities of the gastrointestinal tract are abnormalities in the organs that prevent the digestive system from functioning. They could be further classified based on whether the defect is structural or functional.
Congenital abnormalities of the gastrointestinal tract include:
- Atresia
- Diaphragmatic hernia
- Duplications
- Ectopia
- Fistulae
- Gastroschisis
- Hirschsprung disease
- Meckel diverticulum
- Omphalocele
- Pyloric stenosis
| Abnormalities | Etiology | Diagnosis | Treatment | prognosis |
| Atresia | Not enough blood flow to the intestines | Blood tests, ultrasound, nuclear scan | Surgery, nasogastric tube | Excellent |
| Diaphragmatic Hernia | Genetic disorder | chest x-ray, echocardiogram, blood tests | Surgical repair of the hernia | Fair |
| Duplications | Abnormalities in recanalization, partial twinning | CT scan, Ultrasound, MRI | Excision, enemas | Bad |
| Ectopia | Genetic defect, intrauterine drug exposure and rupture of fetal membranes | Ultrasound, MRI | Emergency surgery after birth | Worst |
| Fistulae | Crohn’s disease, radiation therapy for cancer | CT scan, MRI | Fistulotomy, reconstructive surgery | Fair |
| Gastroschisis | Vascular accident in early embryonic life | Physical examination, Prenatal ultrasonography | Surgery, nutrients by IV and antibiotics to prevent infection | Good |
| Hirschsprung Disease | Mutations in the RET gene | Rectal biopsy, plain abdominal radiograph, Anal manometry | Surgery, IV antibiotics, nasogastric tube insertion and bowel decompression | Good |
| Meckel Diverticulum | Incomplete obliteration of the omphalomesenteric duct | Technetium scan, Colonoscopy, Wireless capsule endoscopy | Surgery, laparoscopic-assisted approach | Excellent |
| Omphalocele | Change in the genes or chromosomes | Prenatal ultrasounds, physical examination of the infant | Surgery | Good |
| Pyloric Stenosis | Unclear | Barium swallow / upper GI series, Abdominal ultrasound, Blood tests | Intravenously fluids, pyloromyotomy | Excellent |
What is Atresia?
Atresia is any congenital malformation of the structure of the intestine that causes bowel obstruction. These defects can either occur in the small or large intestine.
What is the Pathology of Atresia?
The pathology of atresia is:
-Etiology: The cause of atresia is when there is not enough blood flow to the intestines during development. Due to this, the affected intestine either scars or may be reabsorbed.
-Genes involved: CLMP, DHCR7, EFTUD2.
-Pathogenesis: The sequence of events that lead to atresia are: An intrauterine intestinal ischemia due to vascular pathology followed by resorption of the bowel is the possible explanation for the development of intestinal atresia.
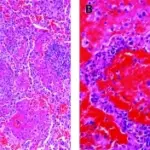
-Histology: The histology associated with atresia are: mucosal edema, congestion, ulceration, flattening of villi, submucosal oedema, prominent vascular proliferation, fibrosis, haemorrhage, gangrene, calcification.
How does Atresia Present?
Patients with atresia typically are both males and females with gestational age of 37 weeks or more. The symptoms, features, and clinical findings associated with atresia include jaundice, dark yellow or brown urine, pale or clay-colored stools, enlarged liver, and weight gain.
How is Atresia Diagnosed?
Atresia is diagnosed by blood tests, liver biopsy, ultrasound, and nuclear scan.
How is Atresia Treated?
Atresia is treated by surgery in the first days of life, giving fluids by placing an intravenous IV line into a vein, nasogastric tube to empty the stomach and keeps gas out.
What is the Prognosis of Atresia?
The prognosis of atresia is excellent when the condition is diagnosed and treated properly. The prognosis is also good for babies with more severe atresia or with associated anomalies, although they will require more advanced, long-term medical care.
What is Diaphragmatic Hernia?
Diaphragmatic hernia is a birth defect where there is a hole in the diaphragm. Organs in the abdomen such as intestines, stomach, and liver can move through the hole in the diaphragm and upwards into a baby’s chest.
What is the Pathology of Diaphragmatic Hernia?
The pathology of diaphragmatic hernia is:
-Etiology: The cause of diaphragmatic hernia is may be related to chromosomal or genetic disorders.
-Genes involved: GATA4 and SOX7.
-Pathogenesis: The sequence of events that lead to diaphragmatic hernia is incomplete formation of the posterolateral portion of the diaphragm. The hole in the diaphragm allows the abdominal viscera to invade the thoracic cavity, which blocks normal lung development.
-Histology: The histology associated with diaphragmatic hernia shows changes in alveolarization, and severely hypoplastic lungs.
How does Diaphragmatic Hernia Present?
Patients with diaphragmatic hernia typically in males with gestational age of 24-37 weeks. The symptoms, features, and clinical findings associated with diaphragmatic hernia include difficulty breathing, increaded heart beat, blue skin discoloration, and bowel sounds in the chest area.
How is Diaphragmatic Hernia Diagnosed?
Diaphragmatic hernia is diagnosed by physical exam, ultrasound, and x-ray.
How is Diaphragmatic Hernia Treated?
Diaphragmatic hernia is treated by surgical repair.
What is the Prognosis of Diaphragmatic Hernia?
The prognosis of diaphragmatic hernia is fair.
What are Duplications?
Gastrointestinal duplications are rare congenital lesions that can develop anywhere along the gastrintestinal tract. Gastrointestinal duplications may present in the newborn period as an abdominal mass. Gastrointestinal duplications may be differentiated from other intraabdominal cystic lesions by the presence of a normal gastrointestinal mucosal lining.
What is the Pathology of Gastrointestinal Duplications?
The pathology of gastrointestinal duplications is:
-Etiology: The cause of gastrointestinal duplications is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to gastrointestinal duplications are unknown.
-Histology: The histology associated with gastrointestinal duplications shows duplicated gastrointestinal tissue.
How does Gastrointestinal Duplications Present?
Patients with gastrointestinal duplications typically in both males and females with before 3-years-old. The symptoms, features, and clinical findings associated with gastrointestinal duplications include nausea, vomiting, obstruction, and abdominal distension. Symptoms are often specific to the location of the lesion.
How is Gastrointestinal Duplications Diagnosed?
Gastrointestinal duplications is diagnosed by computed tomography, ultrasound and magnetic resonance imaging.
How is Gastrointestinal Duplications Treated?
Gastrointestinal duplications is treated by excision. Stool softeners and enemas may improve obstructive symptoms.
What is the Prognosis of Gastrointestinal Duplications?
The prognosis of disease in lower case is fair.
What is Ectopia?
Ectopia is an extremely rare condition in which babies are born with some organs partially or fully outside their bodies.
What is the Pathology of Ectopia?
The pathology of ectopia is:
-Etiology: The cause of ectopia is a rare genetic defect.
-Genes involved: FBN1 gene.
-Pathogenesis: The sequence of events that lead to ectopia are abnormal tissue fusion.
-Histology: The histology associated with ectopia are unknown.
How does Ectopia Present?
Patients with ectopia are typically in all genders. The symptoms, features, and clinical findings associated with ectopia include cranial cleft, cleft lip palate, lungs not developed, scoliosis abnormal hole in diaphragm.
How is Ectopia Diagnosed?
Ectopia is diagnosed by ultrasound in first trimester, and MRI.
How is Ectopia Treated?
Ectopia is treated by ectopia cordis treatment begins with emergency surgery after birth to place the heart inside the baby’s chest and close the thoracic cavity. Additional operations entail building a sternum to protect the heart and repairing any additional heart or abdominal wall defects.
What is the Prognosis of Ectopia?
The prognosis of ectopia is poor.
What is a Fistulae?
Fistulae is an abnormal connection between two body parts, such as an organ or blood vessel and another structure.
What is the Pathology of Fistulae?
The pathology of fistulae is:
-Etiology: The cause of fistulae is channel formation due to inflammation.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to fistulae is due to infection of anal crypts gland. The infection occurs in the ducts of the anal glands and the spreads resulting in an abscess. If the abscess is ruptured, a fistula may form.
-Histology: The histology associated with fistulae shows chronic inflammation, and giant cells.
How does Fistulae Present?
Patients with fistulae typically in all genders and at any age. The symptoms, features, and clinical findings associated with anal fistulae include frequent anal abscesses, pain, swelling, irritation, bleeding, and fever.
How is Fistulae Diagnosed?
Fistulae is diagnosed by CT scan, MRI, anorectal ultrasound.
How is Fistulae Treated?
Fistulae is treated by fistulotomy, filling the fistula with a special glue or plug, and reconstructive surgery.
What is the Prognosis of Fistulae?
The prognosis of fistulas is fair.
What is Gastroschisis?
Gastroschisis is a birth defect of the abdominal belly wall, in which the intestines are present outside the abdomen.
What is the Pathology of Gastroschisis?
The pathology of gastroschisis is:
-Etiology: The cause of gastroschisis is by vascular accident in early embryonic life.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to gastroschisis are due to an abdominal wall that does not form correctly.
-Histology: NA.
How does Gastroschisis Present?
Patients with gastroschisis typically in males and females both at between 18 and 20 weeks of pregnancy. The symptoms, features, and clinical findings associated with gastroschisis include intestines that are visible on the abdomen. Issues may arise due to absorption problems and intestinal irritation.
How is Gastroschisis Diagnosed?
Gastroschisis is diagnosed by physical examination, and prenatal ultrasonography.
How is Gastroschisis Treated?
Gastroschisis is treated by surgery to put the bowel back into the abdomen and close the defect. Other treatments for the baby include nutrients by IV and antibiotics to prevent infection.
What is the Prognosis of Gastroschisis?
The prognosis of gastroschisis is good.
What is Hirschsprung Disease?
Hirschsprung disease is a birth defect in which some nerve cells are missing in the large intestine, so a child’s intestine can’t move stool and becomes blocked.
What is the Pathology of Hirschsprung Disease?
The pathology of Hirschsprung disease is:
-Etiology: The cause of hirschsprung disease is a mutation in a single gene sometimes causes the condition, mutations in multiple genes may be required in some cases.
-Genes involved: Mutations in the RET gene.
-Pathogenesis: The sequence of events that lead to hirschsprung disease are: where ganglionic cells of the myenteric and submucosal plexuses in the bowel aren’t present proximally from the anus to a variable length along the large intestine. The enteric nervous system is derived from the vagal segment of neural crest cells which migrate along the vagus nerve to enter the foregut mesenchyme in a cranial to caudal direction.
-Histology: The histology associated with hirschsprung disease shows failure in peristalsis and bowel movements.
How does Hirschsprung Disease Present?
Patients with hirschsprung disease typically males as compared to female at six months of age. The symptoms, features, and clinical findings associated with hirschsprung disease include vomiting, swollen belly, and constipation.
How is Hirschsprung Disease Diagnosed?
Hirschsprung disease is diagnosed by rectal biopsy, plain abdominal radiograph, and anal manometry.
How is Hirschsprung Disease Treated?
Hirschsprung disease is treated by surgery. Initial management would involve IV antibiotics, nasogastric tube insertion and bowel decompression.
What is the Prognosis of Hirschsprung Disease?
The prognosis of hirschsprung disease is good. In general, more than 90% of patients with Hirschsprung disease report satisfactory outcomes; however, many patients experience disturbances of bowel function for several years before normal continence is established.
What is Meckel Diverticulum?
Meckel diverticulum is an outpouching or bulge in the lower part of the small intestine. The bulge is congenital present at birth and is a leftover of the umbilical cord.
What is the Pathology of Meckel Diverticulum?
The pathology of meckel diverticulum is:
-Etiology: The cause of meckel diverticulum is the incomplete obliteration of the omphalomesenteric duct in the developing embryo.
-Genes involved: BLOC1S1.
-Pathogenesis: The sequence of events that lead to meckel diverticulum is: In early fetal life, the vitelline or omphalomesenteric duct that connects the midgut to the yolk sac is normally obliterated by the 6th week. If the portion connecting to the ileum fails to atrophy, a Meckel diverticulum results.
-Histology: The histology associated with meckel diverticulum shows Ileitis, heterotopic gastric mucosa, pancreatic tissue, or a combination of both.
How does Meckel Diverticulum Present?
Patients with meckel diverticulum typically males present at age range of 2-8 years. The symptoms, features, and clinical findings associated with meckel diverticulum include gastrointestinal bleeding, abdominal pain, and cramping.
How is Meckel Diverticulum Diagnosed?
Meckel diverticulum is diagnosed by: Technetium scan, Colonoscopy, Wireless capsule endoscopy.
How is Meckel Diverticulum Treated?
Meckel diverticulum is treated by surgery.
What is the Prognosis of Meckel Diverticulum?
The prognosis of meckel diverticulum is excellent. Patients can expect a full recovery after treatment. In rare cases, excessive bleeding from Meckel’s diverticulum may occur and become life-threatening.
What is an Omphalocele?
Omphalocele is a birth defect of the abdominal belly wall. The infant’s intestines, liver, or other organs stick outside of the belly through the belly button. The organs are covered in a thin, nearly transparent sac that hardly ever is open or broken.
What is the Pathology of Omphalocele?
The pathology of omphalocele is:
-Etiology: The cause of omphalocele is a change in the genes or chromosomes. Omphalocele might also be caused by a combination of genes and other factors, such as the things the mother comes in contact with in the environment or what the mother eats or drinks, or certain medicines she uses during pregnancy.
-Genes involved: CDKN1C mutation.
-Pathogenesis: The sequence of events that lead to omphalocele are: at early fetal life much of midgut is temporarily herniated outside the abdomen at the umbilicus. The midgut later re-enters the abdomen and opening of abdominal wall is closed. Failure for midgut to return and re-enter the abdomen and omphalocele is formed.
-Histology: The histology associated with omphalocele shows herniated bowel and liver.
How does Omphalocele Present?
Patients with omphalocele typically in males present at age range of 6-10 weeks of pregnancy. The symptoms, features, and clinical findings associated with omphalocele include abdominal contents sticking out through the belly button area.
How is Omphalocele Diagnosed?
Omphalocele is diagnosed by by physical exam and ultrasound.
How is Omphalocele Treated?
Omphalocele is treated by surgery.
What is the Prognosis of Omphalocele?
The prognosis of omphalocele is good.
What is Pyloric Stenosis?
Pyloric stenosis is an uncommon condition in infants that blocks food from entering the small intestine. Normally, a muscular valve pylorus between the stomach and small intestine holds food in the stomach until it is ready for the next stage in the digestive process.
What is the Pathology of Pyloric Stenosis?
The pathology of pyloric stenosis is:
-Etiology: The cause of pyloric stenosis is: The cause of pyloric stenosis is unclear. Risk factors in babies include birth by cesarean section, preterm birth, bottle feeding, and being first born.
-Genes involved: NOS1 gene.
-Pathogenesis: The sequence of events that lead to pyloric stenosis are: hypertrophy and hyperplasia of both the circular and longitudinal muscular layers of the pylorus. This thickening leads to the narrowing of the lumen of the gastric antrum. The pyloric canal becomes lengthened. The muscles of the pylorus become thickened.
-Histology: The histology associated with pyloric stenosis shows muscles of the pylorus are abnormally thickened.
How does Pyloric Stenosis Present?
Patients with pyloric stenosis typically four times more common in males present at age range between 2 and 8 weeks of age, but can occur anytime from birth to 6 months. The symptoms, features, and clinical findings associated with pyloric stenosis include vomiting after feeding, lingering hunger, stomach contractions, dehydration, and lack in weight gain.
How is Pyloric Stenosis Diagnosed?
Pyloric stenosis is diagnosed by physical exam, ultrasound, and barium swallow. Blood tests for electrolytes may be helpful.
How is Pyloric Stenosis Treated?
Pyloric stenosis is treated by adequate hydration, electrolyte replacement, and pyloromyotomy.
What is the Prognosis of Pyloric Stenosis?
The prognosis of pyloric stenosis is excellent.
What is Esophagus Pathology?
Esophagus pathology is an abnormality with the esophagus. Examples include esophagus with reactive or reflux changes, Barrett’s esophagus, anatomic anomalies, and malignancies.
What is Esophageal Obstruction?
Esophageal obstruction is also known as ‘steakhouse syndrome’, is a type of medical emergency caused due to the obstruction of esophagus by ingested foreign body like pork or steak.
What is Achalasia?
Achalasia is a rare disorder that makes it difficult for food and liquid to pass from the swallowing tube connecting the mouth and stomach esophagus into stomach. Achalasia occurs when nerves in the esophagus become damaged.
What is the Pathology of Achalasia?
The pathology of achalasia is:
-Etiology: The cause of achalasia is when nerves in the esophagus become damaged. As a result, the esophagus becomes paralyzed and dilated over time and eventually loses the ability to squeeze food down into the stomach.
-Genes involved: HLA class II genes, CRLF1.
-Pathogenesis: The sequence of events that lead to achalasia are abnormalities in the myenteric plexus.
-Histology: The histology associated with achalasia shows decrease in the neurons of myenteric plexus.
How does Achalasia Present?
Patients with achalasia typically more in males and present at age range of 25 and 60 years. The symptoms, features, and clinical findings associated with achalasia include inability to swallow, dysphagia, and chest pain.
How is Achalasia Diagnosed?
Schalasia is diagnosed by endoscopy, X-ray, and esophageal manometry.
How is Achalasia Treated?
Achalasia is treated with oral medications, stretching of the lower esophageal sphincter dilation, and potentially surgery.
What is the Prognosis of Achalasia?
The prognosis of achalasia is excellent.
What is Esophagitis?
Esophagitis is inflammation that may damage tissues of the esophagus, the muscular tube that delivers food from your mouth to your stomach. Esophagitis can cause painful, difficult swallowing and chest pain.
Examples of esophagitis include:
- Chemical esophagitis
- Eosinophilic esophagitis
- Infectious esophagitis
- Reflux esophagitis
What is Chemical Esophagitis?
Chemical esophagitis is esophageal mucosal injury caused by the medications and usually refers to a direct toxic effect on esophageal mucosa by the culprit medication.
What is the Pathology of Esophagitis?
The pathology of esophagitisis:
-Etiology: The cause of esophagitisis may be due to stomach acids backing up into the esophagus, infection, oral medications and allergies.
-Genes involved: CAPN14.
-Pathogenesis: The sequence of events that lead to esophagitis are reflux of gastric contents are passively regurgitated into the esophagus. Gastric acid, pepsin, and bile irritate the squamous epithelium, leading to erosion and ulceration of esophageal mucosa. Eventually, a columnar epithelial lining may develop. This lining is a premalignant condition termed Barrett esophagus.
-Histology: The histology associated with esophagitis shows intraepithelial eosinophils in at least one high-power field HPF, and alterations in the epithelium and subepithelial connective tissue.
How does Esophagitis Present?
Patients with esophagitis typically more in males and present at age younger than 50 years. The symptoms, features, and clinical findings associated with esophagitis include difficult swallowing, painful swallowing, and chest pain.
How is Esophagitis Diagnosed?
Esophagitis is diagnosed by physical examination and several tests, endoscopy, and biopsy.
How is Esophagitis Treated?
Esophagitis is treated by medications that may include antiviral medications, antifungal medications, antacids, pain relievers, oral steroids, proton pump inhibitors.
What is the Prognosis of Esophagitis?
The prognosis of esophagitis is good.
What is Eosinophilic Esophagitis?
Eosinophilic esophagitis is a chronic immune system disease in which a type of white blood cell eosinophil builds up in the lining of the tube that connects your mouth to your stomach esophagus.
What is the Pathology of Eosinophilic Esophagitis?
The pathology of eosinophilic esophagitis is:
-Etiology: The cause of eosinophilic esophagitis by the presence of a large number of eosinophils in the esophagus. The production and accumulation of eosinophils may be caused by many factors such as immune hypersensitivity responses to particular foods or environmental proteins allergens in some affected individuals.
-Genes involved: TSLP, IL-33.
-Pathogenesis: The sequence of events that lead to eosinophilic esophagitis are incompletely understood but involves genetic, environmental, and host immune system factors. Molecular analysis has elucidated that eosinophilic esophagitis is caused by a primary defect in esophageal epithelial function, rather than an eosinophil defect.
-Histology: The histology associated with eosinophilic esophagitis shows a chronic relapsing antigen-driven disease, is associated with characteristic esophageal histopathology, including ≥15 intraepithelial eosinophils in at least one high-power field HPF, and alterations in the epithelium and subepithelial connective tissue.
How does Eosinophilic Esophagitis Present?
Patients with eosinophilic esophagitis typically 3–4 times more common in males than female present at age younger than 5 years old. The symptoms, features, and clinical findings associated with eosinophilic esophagitis include difficulty swallowing dysphagia, food getting stuck in the esophagus after swallowing, and chest pain.
How is Eosinophilic Esophagitis Diagnosed?
Eosinophilic esophagitis is diagnosed by Upper endoscopy, and biopsy.
How is Eosinophilic Esophagitis Treated?
Eosinophilic esophagitis is treated by dietary therapy, proton pump inhibitors.
What is the Prognosis of Eosinophilic Esophagitis?
The prognosis of eosinophilic esophagitis is good.
What is Infectious Esophagitis?
Infectious esophagitis is a bacterial, viral or fungal infection in tissues of the esophagus.
What is the Pathology of Infectious Esophagitis?
The pathology of infectious esophagitis is:
-Etiology: The cause of infectious esophagitis is fungal, viral, bacterial or even parasitic agents. Risk factors include antibiotics and steroids use, chemotherapy and/or radiation therapy, malignancies and immunodeficiency syndromes including acquired immunodeficiency syndrome.
-Genes involved: TSLP, LRRC32.
-Pathogenesis: The sequence of events that lead to infectious esophagitis colonization with mucosal adherence and proliferation.
-Histology: The histology associated with infectious esophagitis shows nuclear molding, margination, and multinucleation of infected cells. Eosinophilic intranuclear and cytoplasmic inclusion bodies within squamous cells, referred to as Cowdry type A inclusions, may be seen.
How does Infectious Esophagitis Present?
Patients with infectious esophagitis typically more in males and present at age range of 11 to 84 years. The symptoms, features, and clinical findings associated with infectious esophagitis include: pain when swallowing, difficulty swallowing, mouth pain, chest pain, nausea or vomiting.
How is Infectious Esophagitis Diagnosed?
Infectious esophagitis is diagnosed by endoscopy and esophageal biopsy.
How is Infectious Esophagitis Treated?
Infectious esophagitis is treated with antiviral medicines, such as acyclovir. Bacterial esophagitis may be treated with broad-spectrum antibiotics. These are medicines that work against many types of bacteria. Sometimes acid blockers are used along with other treatments.
What is the Prognosis of Infectious Esophagitis?
The prognosis of infectious esophagitis is poor. Severe esophagitis may lead to dysphagia, pain, odynophagia, and malnutrition. Rarely, life-threatening bleeding occurs and may lead to death. Outcomes and survival in these patients are related to the severity of their underlying systemic illness.
What is Reflux Esophagitis?
Reflux esophagitis is an esophageal mucosal injury that occurs secondary to retrograde flux of gastric contents into the esophagus. Clinically, this is referred to as gastroesophageal reflux disease or GERD.
What is the Pathology of Reflux Esophagitis?
The pathology of reflux esophagitis is:
-Etiology: The cause of reflux esophagitis is acid reflux also called gastroesophageal reflux disease or GERD. It is a backflow of digestive acid from the stomach, resulting in a chemical burn of the esophagus.
-Genes involved: FOXF1, MHC, CCND1.
-Pathogenesis: The sequence of events that lead to reflux esophagitis indicate that reflux esophagitis is the result of the failure of the lower esophageal sphincter to prevent the regurgitation of gastroduodenal secretions with subsequent esophageal mucosal injury.
-Histology: The histology associated with reflux esophagitis shows basal cell hyperplasia, elongation of vascular papillae, intercellular edema, presence of intraepithelial eosinophils, intraepithelial lymphocytosis, ballooning degeneration of squamous cells.
How does Reflux Esophagitis Present?
Patients with reflux esophagitis typically more in women and present at after 50s. The symptoms, features, and clinical findings associated with reflux esophagitis include heartburn, dysphagia, pain may be mistaken for myocardial infarction.
How is Reflux Esophagitis Diagnosed?
Reflux esophagitis is diagnosed by clinical heartburn, regurgitation, and intraesophageal pH monitoring to detect acid.
How is Reflux Esophagitis Treated?
Reflux esophagitis is treated by proton pump inhibitor therpay.
What is the Prognosis of Reflux Esophagitis?
The prognosis of reflux esophagitis is good. Chronic cases often respond to prescription drugs, and severe cases may require surgery to avoid serious complications.
What are Esophageal Lacerations?
Esophageal Lacerations is a disorder characterized by upper gastrointestinal tract bleeding caused by longitudinal mucosa a tear that does not penetrate the wall of the esophagus. The tear can be caused by forceful vomiting.
What is the Pathology of Esophageal Lacerations
The pathology of esophageal lacerations is:
-Etiology: The cause of esophageal lacerations is violent coughing or vomiting.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to esophageal lacerations occurs when intraabdominal pressure suddenly and severely increases as in cases of forceful retching and vomiting, the gastric contents rush proximally under pressure into the esophagus. This excess pressure from the gastric contents results in longitudinal mucosal tears which may reach deep into the submucosal arteries and veins, resulting in upper GI bleeding.
-Histology: The histology associated with esophageal lacerations shows rupturing of blood vessels.
How does Esophageal Lacerations Present?
Patients with esophageal lacerations typically in male present at age range of 50 to 70 years. The symptoms, features, and clinical findings associated with esophageal lacerations include: bright-red blood in vomit, and pain or stiffness in the neck.
How is Esophageal Lacerations Diagnosed?
Esophageal lacerations is diagnosed by endoscopy, angiography.
How is Esophageal Lacerations Treated?
Esophageal lacerations is treated by using heat to cauterize the bleeding blood vessel, clipping it closed, or injecting a drug into it.
What is the Prognosis of Esophageal Lacerations?
The prognosis of esophageal lacerations is good.
What is Barrett Esophagus?
Barrett esophagus is a condition in which the flat pink lining of the swallowing tube that connects the mouth to the stomach esophagus becomes damaged by acid reflux, which causes the lining to thicken and become red.
What is the Pathology of Barrett Esophagus?
The pathology of barrett esophagus is:
-Etiology: The cause of barrett esophagus is not yet known. However, the condition is most often seen in people with GERD.
-Genes involved: MSR1, CTHRC1, and ASCC1.
-Pathogenesis: The sequence of events that lead to barrett esophagus are metaplastic columnar mucosa containing epithelial cells with gastric and intestinal features replaces esophageal squamous mucosa damaged by gastroesophageal reflux disease.
-Histology: The histology associated with barrett esophagus shows an acquired condition that results from chronic gastro-esophageal reflux. It is characterized by the metaplastic replacement of the normal squamous epithelium of the lower oesophagus by columnar epithelium.
How does Barrett Esophagus Present?
Patients with barrett esophagus typically in male and present at age range of over 50-years-old. The symptoms, features, and clinical findings associated with barrett esophagus include heartburn, regurgitation of stomach contents, and difficulty swallowing.
How is Barrett Esophagus Diagnosed?
Barrett esophagus is diagnosed by endoscopy.
How is Barrett Esophagus Treated?
Barrett esophagus is treated by proton pump inhibitors, and photodynamic therapy.
What is the Prognosis of Barrett Esophagus?
The prognosis of Barrett esophagus is good. In many cases, treatment improves acid reflux symptoms and keeps Barrett esophagus from getting worse. People with Barrett esophagus do have a greater risk than the general population of developing esophageal cancer.
What are Esophageal Varices?
Esophageal varices are enlarged veins in the esophagus.
What is the Pathology of Esophageal Varices?
The pathology of esophageal varices is:
-Etiology: The cause of esophageal varices is related to severe liver scarring cirrhosis, blood clot thrombosis, or parasitic infections.
-Genes involved: SST.
-Pathogenesis: The sequence of events that lead to esophageal varices are: increases portal pressures such as with cirrhosis, there is dilation of veins in the anastomosis, leading to esophageal varices. Splenic vein thrombosis is a rare condition that causes esophageal varices without a raised portal pressure.
-Histology: The histology associated with esophageal varices shows expansion of the submucosa leads to elevation of the mucosa above the surrounding tissue, which is apparent during endoscopy and is a key diagnostic feature. Evidence of recent variceal hemorrhage includes necrosis and ulceration of the mucosa.
How does Esophageal Varices Present?
Patients with esophageal varices typically more in males and present at age range of 48-years-old. The symptoms, features, and clinical findings associated with esophageal varices include vomiting large amounts of blood, black, tarry or bloody stools, lightheadedness, loss of consciousness in severe cases.
How are Esophageal Varices Diagnosed?
Esophageal varices are diagnosed by endoscopic exam, imaging tests, or capsule endoscopy.
How are Esophageal Varices Treated?
Esophageal varices is are treated by using elastic bands to tie off bleeding veins, medications to slow blood flow into the portal vein, diverting blood flow away from the portal vein, or placing pressure on varices to stop bleeding.
What is the Prognosis of Esophageal Varices?
The prognosis of esophageal varices is poor. Bleeding esophageal varices is life-threatening condition and can be fatal in up to 50% of patients. People who have had an episode of bleeding esophageal varices are at risk for bleeding again.
What are Esophageal Tumors?
Esophageal Tumors are malignant cancer cells form in the tissues of the esophagus, a tube-like structure that runs from your throat to your stomach. Food goes from the mouth to the stomach through the esophagus. The cancer starts at the inner layer of the esophagus and can spread throughout the other layers of the esophagus and to other parts of the body metastasis.
What is an Adenocarcinoma?
An adenocarcinoma is a type of cancer that starts in mucus-producing glandular cells. Many organs have these types of cells and adenocarcinoma can develop in any of these organs.
What is the Pathology of Adenocarcinoma?
The pathology of adenocarcinoma is:
-Etiology: The cause of adenocarcinoma is smoking, toxin exposure, previous radiation therapy.
-Genes involved: p53 or TP53.
-Pathogenesis: The sequence of events that lead to adenocarcinoma are glandular cells which secrete mucous, digestive juices or other liquids and begin to grow in the glands that line your organs, they can eventually spread to other parts of your body. This may include the brain, liver, lungs, lymph nodes, or bone.
-Histology: The histology associated with adenocarcinoma shows malignant glands.
How does Adenocarcinoma Present?
Patients with adenocarcinoma are middle aged. The symptoms, features, and clinical findings associated with adenocarcinoma include abdominal pain, nausea, and vomiting.
How is Adenocarcinoma Diagnosed?
Adenocarcinoma is diagnosed by blood tests, CT scan, MRI, and biopsy.
How is Adenocarcinoma Treated?
Adenocarcinoma is treated by surgery, chemotherapy, and radiation therapy.
What is the Prognosis of Adenocarcinoma?
The prognosis of adenocarcinoma is poor.
What is Squamous Cell Carcinoma?
Squamous cell carcinoma is a common form of skin cancer that develops in the squamous cells that make up the middle and outer layers of the skin. Squamous cell carcinoma of the skin is usually not life-threatening, though it can be aggressive.
What is the Pathology of Squamous Cell Carcinoma?
The pathology of squamous cell carcinoma is:
-Etiology: The cause of squamous cell carcinoma is prolonged exposure to ultraviolet UV radiation, either from sunlight or from tanning beds or lamps.
-Genes involved: TP53, GRM8, BAI3, ERBB4, RUNX1T1, KEAP1, FBXW7, KRAS,
-Pathogenesis: The sequence of events that lead to squamous cell carcinoma is multifactorial and includes many extrinsic and intrinsic factors. The most important extrinsic factor is generally recognized as UV sunlight exposure. As lifetime UV exposure increases, so does the incidence of squamous cell carcinoma.
-Histology: The histology associated with squamous cell carcinoma shows nests of squamous epithelial cells arising from the epidermis and extending into the dermis. The malignant cells are often large with abundant eosinophilic cytoplasm and a large, often vesicular, nucleus. Variable keratinisation and keratin pearls may be present.
How does Squamous Cell Carcinoma Present?
Patients with squamous cell carcinoma typically more in male at age between 50 and 70 years. The symptoms, features, and clinical findings associated with squamous cell carcinoma include: a firm, red nodule, a flat sore with a scaly crust, a new sore or raised area on an old scar or ulcer, a rough, scaly patch on your lip that may evolve to an open sore, a red sore or rough patch inside your mouth.
How is Squamous Cell Carcinoma Diagnosed?
Squamous cell carcinoma is diagnosed by: skin diagnosis, biopsy of skin lesions, lymph node biopsy, x-ray, and CT scan.
How is Squamous Cell Carcinoma Treated?
Squamous cell carcinoma is treated by surgical excision, cryotherapy, curettage or topical 5-fluorouracil.
What is the Prognosis of Squamous Cell Carcinoma?
The prognosis of squamous cell carcinoma is good. Squamous cell carcinoma (SCC) generally has a high survival rate.
What is Stomach Pathology?
Stomach pathology is a congenital anomaly pyloric stenosis with inflammatory conditions such as gastritis, peptic ulcers and tumors.
What is Gastropathy?
Gastropathy is a condition that affects the stomach lining, also known as the mucosa. In gastritis, the stomach lining is inflamed. In gastropathy, the stomach lining is damaged, but little or no inflammation is present.
What is Acute Gastritis?
Acute gastritis is an inflammation or irritation of the stomach lining. The condition tends to last for a short period of time only. If the inflammation persists, however, the condition is referred to as chronic gastritis. Acute gastritis can affect people of all ages, though it’s more common in adulthood and old age.
What is the Pathology of Acute Gastritis?
The pathology of acute gastritis is:
-Etiology: The cause of acute gastritis is injury, bacteria, viruses, stress, or ingesting irritants such as alcohol, NSAIDs, steroids, or spicy food.
-Genes involved: IL1B-31.
-Pathogenesis: The sequence of events that lead to acute gastritis are: as a result of the trigger by factors such as NSAIDs, stress, bile reflux, radiation, alcohol abuse, cocaine addiction, and ischemic damage. The outcome of these triggers may result in ulcers, hemorrhage and erosion of the gastric mucosa.
-Histology: The histology associated with acute gastritis shows hyperemia, acute inflammation, increased polymorphonuclear neutrophil in the superficial lamina propria, erosion of the surface epithelium, sloughing, mucosal necrosis to a greater extent, scarring.
How does Acute Gastritis Present?
Patients with acute gastritis are typically both genders of all ages. The symptoms, features, and clinical findings associated with acute gastritis include a burning ache or pain, indigestion in your upper abdomen that may become either worse or better with eating, nausea, vomiting, a feeling of fullness in your upper abdomen after eating.
How is Acute Gastritis Diagnosed?
Acute gastritis is diagnosed by a blood, breath, or saliva test to check for H. pylori.
How is Acute Gastritis Treated?
Acute gastritis is treated by antacids and other drugs such as proton pump inhibitors or H-2 blockers to reduce stomach acid, avoiding hot and spicy foods.
What is the Prognosis of Acute Gastritis?
The prognosis of acute gastritis is good.
What is Stress-Related Mucosal Disease?
Stress related mucosal disease is a stress-related injury superficial mucosal damage and stress ulcers focal deep mucosal damage. Both types are caused by mucosal ischemia, and both show a propensity for the acid-producing corpus and fundus.
What is the Pathology of Stress-Related Mucosal Disease?
The pathology of stress-related mucosal disease is:
-Etiology: The cause of stress-related mucosal disease is mucosal erosions and superficial hemorrhages in patients who are critically ill or in those who are under extreme physiologic stress, resulting in minimal-to-severe.
-Genes involved: HSP-70.
-Pathogenesis: The sequence of events that lead to stress-related mucosal disease are gastric mucosal injury which is most often due to local ischemia. Upregulation and increased release of the vasoconstrictor endothelin-1 also contributes to ischemic gastric mucosal injury while increased COX-2 expression appears to be protective. Systemic acidosis may also contribute to mucosal injury by lowering the intracellular pH of mucosal cells.
-Histology: The histology associated with stress-related mucosal disease are: shallow erosions to deeper lesions that involve the entire mucosal thickness true ulceration.
How does Stress-Related Mucosal Disease Present?
Patients with stress-related mucosal disease typically all genders of any age but more in people with age >50years. The symptoms, features, and clinical findings associated with stress-related mucosal disease include: Acute gastroduodenal lesions related to severe sepsis. Respiratory failure, hypotension, sepsis, and jaundice. Sepsis and gastrointestinal bleeding.
How is Stress-Related Mucosal Disease Diagnosed?
Stress-related mucosal disease is diagnosed by endoscopy.
How is Stress-Related Mucosal Disease Treated?
Stress-related mucosal disease is treated by antacids, cimetidine, and other histamine H2-receptor antagonists, and vigorous acid suppression.
What is the Prognosis of Stress-Related Mucosal Disease?
The prognosis of disease in lower case is good. Mortality is increased in people with clinically significant bleeding compared to those patients who do not bleed. Institution of prophylaxis is recommended in high-risk patients.
What is Chronic Gastritis?
Chronic gastritis is a long-term condition in which the mucus lined layer of the stomach, also known as the gastric mucosa, is inflamed or irritated over a longer period of time. Symptoms tend to appear slowly, over time.
What is the Pathology of Chronic Gastritis?
The pathology of chronic gastritis is:
-Etiology: The cause of chronic gastritis is: the presence of bacteria H. pylori, long-term use of certain medications aspirin and ibuprofen,excessive alcohol consumption, certain illnesses diabetes or kidney failure, a weakened immune system.
-Genes involved: c-Myc and p53.
-Pathogenesis: The sequence of events that lead to chronic gastritis are the continuous mucosal injury due to long-standing H. pylori infection, leads to atrophy of stomach. This continuous pathological process results in erosion or ulceration of the mucosa leading to the destruction of the glandular layer and followed by fibrous replacement.
-Histology: The histology associated with chronic gastritis shows inflammatory infiltrates of neutrophils localized on the foveolar layer stroma of gastric mucous membrane in the case of acute gastritis. Chronic gastritis is characterized by an infiltrate of lymphoid cells, plasmatic cells and acidophilic granulocytes.
How does Chronic Gastritis Present?
Patients with chronic gastritis typically all sexes at older age. The symptoms, features, and clinical findings associated with chronic gastritis include: upper abdominal pain, Indigestion, bloating, nausea, vomiting, belching, loss of appetite, weight loss.
How is Chronic Gastritis Diagnosed?
Chronic gastritis is diagnosed by an endoscopy, in which a camera attached to a long tube is inserted into your mouth and down into your digestive tract, a test for the bacteria that cause stomach ulcers, a stool test to look for stomach bleeding, a blood count and an anemia test.
How is Chronic Gastritis Treated?
Chronic gastritis is treated by: medications antacids, including calcium carbonate Rolaids and Tums, proton pump inhibitors, and diet.
What is the Prognosis of Chronic Gastritis?
The prognosis of chronic gastritis is good. The prognosis of chronic gastritis is strongly related to the underlying cause.
What is Autoimmune Gastritis?
Autoimmune gastritis is an increasingly prevalent, organ-specific, immune-mediated disorder characterized by the destruction of gastric parietal cells, leading to the loss of intrinsic factor and reduced acid output.
What is the Pathology of Autoimmune Gastritis?
The pathology of autoimmune gastritis is:
-Etiology: The cause of autoimmune gastritis is unknown but affected people are likely to have other autoimmune disorders including autoimmune thyroiditis, diabetes type I, Addison’s disease, and vitiligo.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to autoimmune gastritis are restricted to oxyntic acid-producing mucosa in the corpus anatomic body and fundus of the stomach. Normally, the parietal cells in the oxyntic mucosa produce hydrochloric acid and intrinsic factor.
-Histology: The histology associated with autoimmune gastritis shows diffuse mononuclear infiltrates within the lamina propria that are heavier in the deeper, glandular portions. Patchy lymphocytic infiltrates and damage to oxyntic glands.
How does Autoimmune Gastritis Present?
Patients with autoimmune gastritis typically are all sexes at any age. The symptoms, features, and clinical findings associated with autoimmune gastritis include nausea, vomiting, a feeling of fullness in the upper abdomen after eating, or abdominal pain.
How is Autoimmune Gastritis Diagnosed?
Autoimmune gastritis is diagnosed by certain blood test, biopsy of stomach lining.
How is Autoimmune Gastritis Treated?
Autoimmune gastritis is treated by treating vitamin B12 and iron deficiencies, antibiotics for bacterial infections.
What is the Prognosis of Autoimmune Gastritis?
The prognosis of autoimmune gastritis is good. In some cases, acute gastritis can lead to serious or life-threatening complications, such as gastrointestinal hemorrhage.
What is Helicobacter Pylori Gastritis?
Helicobacter pylori gastritis is bacteria that can cause an infection in the stomach or duodenum first part of the small intestine. It’s the most common cause of peptic ulcer disease. H. pylori can also inflame and irritate the stomach lining gastritis.
What is the Pathology of Helicobacter Pylori Gastritis?
The pathology of helicobacter pylori gastritis is:
-Etiology: The cause of helicobacter pylori gastritis is: bacteria that infect and inflame the stomach lining. The term gastritis refers specifically to abnormal inflammation in the stomach lining.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to helicobacter pylori gastritisare infection in humans can be described in three steps: entry to adherence to and colonization of the human gastric mucosa, exploitation of the human immune system and transmission to a new susceptible host.
-Histology: The histology associated with pylori gastritis are: irregular surface epithelium, loss of apical mucin, cell dropout, formation of pits and microerosions.
How does Helicobacter Pylori Gastritis Present?
Patients with helicobacter pylori gastritis typically more in males present under age of 5 years. The symptoms, features, and clinical findings associated with helicobacter pylori gastritis include: dull or burning pain in your stomach more often a few hours after eating and at night, unplanned weight loss, bloating, nausea and vomiting bloody vomit, indigestion dyspepsia, burping, loss of appetite.
How is Helicobacter Pylori Gastritis Diagnosed?
Helicobacter pylori gastritis is diagnosed by urea breath test, stool antigen test, and testing of endoscopic biopsy samples.
How is Helicobacter Pylori Gastritis Treated?
Helicobacter pylori gastritis is treated by antibiotics, and a proton pump inhibitor.
What is the Prognosis of Helicobacter Pylori Gastritis?
The prognosis of helicobacter pylori gastritis is fair. H. pylori infection is not easily cured, and research has shown that multidrug therapy is required. As with any bacterial infection, therapy must include antimicrobial agents to which the bacterium is sensitive.
What is Peptic Ulcer Disease?
Peptic ulcer disease are open sores that develop on the inside lining of your stomach and the upper portion of your small intestine. The most common symptom of a peptic ulcer is stomach pain. Peptic ulcers include gastric ulcers that occur on the inside of the stomach.
What is the Pathology of Peptic Ulcer Disease?
The pathology of peptic ulcer disease is:
-Etiology: The cause of peptic ulcer disease are Helicobacter pylori and NSAID medications.
-Genes involved: NA.
-Pathogenesis: The sequence of events that lead to peptic ulcer disease are defects in the gastric or duodenal mucosa that extend through the muscularis mucosa. The epithelial cells of the stomach and duodenum secrete mucus in response to irritation of the epithelial lining and as a result of cholinergic stimulation. The superficial portion of the gastric and duodenal mucosa exists in the form of a gel layer, which is impermeable to acid and pepsin.
-Histology: The histology associated with peptic ulcer disease shows Lesions. The surface is covered with slough and inflammatory debris.
How does Peptic Ulcer Disease Present?
Patients with peptic ulcer disease typically both in male or female and present at any age. The symptoms, features, and clinical findings associated with peptic ulcer disease include: burning stomach pain, feeling of fullnessbloating or belching, intolerance to fatty foods, heartburn, and nausea.
How is Peptic Ulcer Disease Diagnosed?
Peptic ulcer disease is diagnosed by endoscopy and biopsy.
How is Peptic Ulcer Disease Treated?
Peptic ulcer disease is treated by proton pump inhibitors PPI, histamine receptor blockers H2 blockers, antibiotics, and protective medications.
What is the Prognosis of Peptic Ulcer Disease?
The prognosis of peptic ulcer disease is good. The prognosis of peptic ulcer disease PUD is excellent after the underlying cause is successfully treated. Recurrence of the ulcer may be prevented by maintaining good hygiene and avoiding alcohol, smoking, and NSAIDs. Unfortunately, recurrence is common with rates exceeding 60% in most series.
What is Mucosal Atrophy?
Mucosal atrophy is the loss of appropriate glands, which occurs when glands damaged by inflammation are replaced either by connective tissue scarring or by glandular structures inappropriate for location metaplasia.
What is the Pathology of Mucosal Atrophy?
The pathology of mucosal atrophy is:
-Etiology: The causes of mucosal atrophy are autoimmune due to pernicious anemia or chronic Helicobacter pylori infection.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to mucosal atrophy are low gastric acid output and hypergastrinemia, which may lead to enterochromaffin-like ECL cell hyperplasia and carcinoid tumors.
-Histology: The histology associated with mucosal atrophy shows severe mucosal damage, erosions and hemorrhage.
How does Mucosal Atrophy Present?
Patients with mucosal atrophy typically more severe in men and present at any age range. The symptoms, features, and clinical findings associated with mucosal atrophy include: stomach pain, nausea and vomiting, loss of appetite, unexpected weight loss, stomach ulcers.
How is Mucosal Atrophy Diagnosed?
Mucosal atrophy is diagnosed by endoscopy and biopsy.
How is Mucosal Atrophy Treated?
Mucosal atrophy is treated antibiotics and vitamin B12 injections.
What is the Prognosis of Mucosal Atrophy?
The prognosis of mucosal atrophy is not good. It will finally end up in a permanently acid-free stomach in the most extreme cases. Severe atrophic gastritis and acid-free stomach are the highest independent risk conditions for gastric cancer.
What is Intestinal Metaplasia?
Intestinal metaplasia is a precancerous change of the mucosa of the stomach with intestinal epithelium and is associated with an increased risk of dysplasia and cancer.
What is the Pathology of Intestinal Metaplasia?
The pathology of intestinal metaplasia is:
-Etiology: The cause of intestinal metaplasia are smoking, H. pylori infection, genetics having a close, first-degree relative with gastric cancer, environmental factors.
-Genes involved: SOX2, CDX.
-Pathogenesis: The sequence of events that lead to intestinal metaplasia are the replacement of one differentiated somatic cell type with another differentiated somatic cell type in the same tissue. Typically, metaplasia is triggered by environmental stimuli, which may act in concert with the deleterious effects of microorganisms and inflammation.
-Histology: The histology associated with intestinal metaplasia shows chronic inflammation due to Helicobacter pylori infection.
How does Intestinal Metaplasia Present?
Patients with intestinal metaplasia typically are both male or female at any age. The symptoms, features, and clinical findings associated with intestinal metaplasia include: acid reflux, ulcers, gastritis, or gastroesophageal reflux disease.
How is Intestinal Metaplasia Diagnosed?
Intestinal metaplasia is diagnosed by upper endoscopy with biopsy.
How is Intestinal Metaplasia Treated?
Intestinal metaplasia is treated by removing the H. pylori infection completely by antibiotics.
What is the Prognosis of Intestinal Metaplasia?
The prognosis of intestinal metaplasia is poor. Intestinal metaplasia is believed to be a precancerous lesion that may lead to gastric cancer. If you have intestinal metaplasia, then your risk of getting gastric cancer is increased six times.
What is Stomach Metaplasia?
Stomach Metaplasia is a precancerous change of the mucosa of the stomach and is associated with an increased risk of dysplasia and cancer.
What is the Pathology of Stomach Metaplasia?
The pathology of stomach metaplasia is:
-Etiology: The cause of stomach metaplasia is helicobacter pylori infection, high salt intake, smoking, alcohol consumption, and chronic bile reflux.
-Genes involved: RUNX3.
-Pathogenesis: The sequence of events that lead to stomach metaplasia are a pre-neoplastic lesion that usually follows Helicobacter pylori infection and that confers increased risk for gastric cancer development. After setting the role played by CDX2 Caudal-type homeobox 2 in the establishment of gastric IM, it became of foremost importance to unravel the regulatory mechanisms behind its de novo expression in the stomach.
-Histology: The histology associated with stomach metaplasia shows differentiated epithelium.
How does Stomach Metaplasia Present?
Patients with stomach metaplasia typically are both male or female at any age. The symptoms, features, and clinical findings associated with stomach metaplasia include upper abdominal pain, indigestion, bloating, nausea, and vomiting.
How is Stomach Metaplasia Diagnosed?
Stomach metaplasia is diagnosed by endoscopy with biopsy.
How is Stomach Metaplasia Treated?
Stomach metaplasia is treated by removing the H. pylori infection completely, and using antioxidant agents.
What is the Prognosis of Stomach Metaplasia?
The prognosis of stomach metaplasia is good. Metaplasia is defined as a potentially reversible change from a fully differentiated cell type to another.
What is Gastritis Cystica?
Gastritis cystica is a rare pseudotumor of the stomach characterized by benign growths of deep gastric glands through the muscularis mucosae into the submucosa.
What is the Pathology of Gastritis Cystica?
The pathology of gastritis cystic is:
-Etiology: The cause of gastritis cystic is : weak immune system, major surgery.
-Genes involved: Targeted Deletion of Kcne2.
-Pathogenesis: The sequence of events that lead to gastritis cystic are a rare disease characterized by polypoid hyperplasia of the gastric mucosa. It is a rare hyperplastic lesion with unclear pathogenesis.
-Histology: The histology associated with gastritis cystic shows gastritis cystica superficialis, in which cystic glands are limited to the mucosal layer; and gastritis cystica profunda, in which there is cystic gland infiltration into the submucosal layer.
How does Gastritis Cystica Present?
Patients with gastritis cystic typically are male at older ages. The symptoms, features, and clinical findings associated with gastritis cystic include: epigastric pain and abdominal fullness, gastrointestinal bleeding and weight loss.
How is Gastritis Cystica Diagnosed?
Gastritis cystica is diagnosed by endoscopy.
How is Gastritis Cystica Treated?
Gastritis cystica is treated by antacids, protonix, surgical removal of the lesion
What is the Prognosis of Gastritis Cystica?
The prognosis of gastritis cystica is fair. It is usually considered a benign lesion, but it can be a precancerous gastric lesion. Although it is extremely rare, it should be considered in the differential diagnosis of elevated lesions in the stomach.
What are Hypertrophic Gastropathies?
Hypertrophic gastropathy is a rare idiopathic hyperproliferative disorder which may present as Menetrier’s disease MD characterized by foveolar hyperplasia in the gastric fundus and body. It is often accompanied by a severe loss of plasma proteins including albumin from the altered gastric mucosa.
What is the Pathology of Hypertrophic Gastropathies?
The pathology of hypertrophic gastropathies is:
-Etiology: The cause of hypertrophic gastropathies is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to hypertrophic gastropathiesare a rare idiopathic hyperproliferative disorder which may present as Menetrier’s disease (MD) characterized by foveolar hyperplasia in the gastric fundus and body. It is often accompanied by a severe loss of plasma proteins including albumin from the altered gastric mucosa.
-Histology: The histology associated with hypertrophic gastropathies shows hypertrophic hypersecretory gastropathy is a rare acquired gastropathy that involves hypersecretion of acid, pepsin, and mucin. endoscopically, it is characterized by hypertrophic gastric folds and “cobblestone” gastric body mucosa with atrophic antral mucosa.
How does Hypertrophic Gastropathies Present?
Patients with hypertrophic gastropathies typically are male at age range of 30 and 60 years. The symptoms, features, and clinical findings associated with hypertrophic gastropathies include: vomiting, diarrhea, and weight loss.
How is Hypertrophic Gastropathies Diagnosed?
Hypertrophic gastropathies is diagnosed by CT scan, an upper GI endoscopy, and a biopsy.
How is Hypertrophic Gastropathies Treated?
Hypertrophic gastropathies is treated by Cetuximab or other medications.
What is the Prognosis of Hypertrophic gastropathies?
The prognosis of hypertrophic gastropathies is good. In children, it is usually from CMV infection and lasts for 2-14 weeks, with complete resolution being the rule. In adults, this may increase a patient’s risk of stomach cancer. Thus, a periodic endoscopic surveillance is necessary.
What is Menetrier Disease?
Menetrier disease is the ridges along the inside of the stomach wall called rugae to enlarge, forming giant folds in the stomach lining. The rugae enlarge because of an overgrowth of mucous cells in the stomach wall. In a normal stomach, mucous cells in the rugae release protein-containing mucus.
What is the Pathology of Menetrier Disease?
The pathology of menetrier disease is:
-Etiology: The cause of menetrier disease is unknown.
-Genes involved: SMAD4.
-Pathogenesis: The sequence of events that lead to menetrier disease is incompletely understood but may involve transforming growth factor-alpha TGF-α. TGF-α increases gastric mucus production and inhibits acid secretion,241 and levels are usually elevated in the gastric mucous cells in patients with Ménétrier disease.
-Histology: The histology associated with menetrier disease shows evident by marked enlargement of gastric folds and rugae. On histopathological examination, foveolar hyperplasia, oxyntic glands atrophy, reduction in parietal acid-producing cells and chief pepsinogen- producing cells, and cystic dilation of pits are seen. The overall linear architecture is usually maintained. Edema and hyperplasia of smooth muscle in the lamina propria are observed.
How does Menetrier Disease Present?
Patients with menetrier disease typically more in male at age range 30-60 years mostly but cases in childhood are also reported. The symptoms, features, and clinical findings associated with menetrier disease include: nausea and frequent vomiting, Diarrhea,loss of appetite, extreme weight loss, Malnutrition, low levels of protein in the blood.
How is Menetrier Disease Diagnosed?
Menetrier disease is diagnosed by computerized tomography CT scan, and biopsy.
How is Menetrier Disease Treated?
Menetrier disease is treated by anticholergic drugs, acid suppression therapy, and antibiotic therapy directed against H. pylori infection.
What is the Prognosis of Menetrier Disease?
The prognosis of menetrier disease is good. The prognosis of Ménétrier disease varies from person to person. Resolution of symptoms may occur in adults with an underlying Helicobacter Pylori H. Pylori infection once treatment of the infection occurs. Cases in children may resolve spontaneously or with treatment of the underlying CMV infection.
What is Zollinger-Ellison Syndrome?
Zollinger-Ellison syndrome is a rare digestive disorder that results in too much gastric acid. This excess gastric acid can cause peptic ulcers in your stomach and intestine.
What is the Pathology of Zollinger-Ellison Syndrome?
The pathology of zollinger-ellison syndrome is:
-Etiology: The cause of zollinger-ellison syndrome is tumors.
-Genes involved: MEN1 mutations.
-Pathogenesis: The sequence of events that lead to zollinger-ellison syndrome are condition in which one or more tumors form in your pancreas or the upper part of your small intestine duodenum. These tumors, called gastrinomas, secrete large amounts of the hormone gastrin, which causes your stomach to produce too much acid.
-Histology: The histology associated with zollinger-ellison syndrome shows that the cells are arranged in a solid, trabecular, gyriform, or glandular pattern, with fairly uniform nuclei, salt-and-pepper chromatin, and finely granular cytoplasm. As with other pancreatic NETs, the degree of malignancy cannot be predicted by morphologic appearance alone.
How does Zollinger-Ellison Syndrome Present?
Patients with zollinger-ellison syndrome typically all sexes at age range of 20 to 50 years. The symptoms, features, and clinical findings associated with zollinger-ellison syndrome include nausea, vomiting, weight loss, diarrhea, abdominal painand severe heartburn.
How is Zollinger-Ellison Syndrome Diagnosed?
Zollinger-ellison syndrome is diagnosed by: blood test to look for high levels of gastrin.
How is Zollinger-Ellison Syndrome Treated?
Zollinger-ellison syndrome is treated by removing as much of the tumor as possible.
What is the Prognosis of Zollinger-Ellison Syndrome?
The prognosis of Zollinger-Ellison syndrome (ZES) is good. In most people with ZES, tumors grow slowly and don’t spread quickly. If you can manage the ulcers, you can enjoy good quality of life.
What are Gastric Polyps?
Gastric polyps are masses of cells that form on the lining inside your stomach. These polyps are rare and usually don’t cause any signs or symptoms. Stomach polyps are most often discovered when your doctor is examining you for some other reason.
Examples of gastric polyps are:
- Inflammatory polyps
- Fundic gland polyps
- Hyperplastic polyps
| Polyps’ types | Etiology | Histological changes | Diagnosis | Treatment | Prognosis |
| Inflammatory Polyps | Age, inflammatory intestinal conditions | inflammation of granulation tissue | Colonoscopy, biopsy | medications, removal of polyps | Good |
| Fundic Gland Polyps | Chronic stomach inflammation | larger size of dilated fundic gland cysts | Endoscopy | discontinuing proton pump inhibitors, removing polyp | Good |
| Hyperplastic Polyps | chronic gastritis, H. pylori gastritis, pernicious anemia | cell elongation, accentuation of lateral intercellular interdigitations | Colonoscopy, CT scan | endoscopic procedure, eating diet and nutritional changes | Good |
What are Inflammatory Polyps?
Inflammatory polyps are non-neoplastic intraluminal projections of mucosa consisting of stromal and epithelial components and inflammatory cells. Inflammatory polyps include inflammatory pseudopolyps and prolapse type inflammatory polyps.
What is the Pathology of Inflammatory Polyps?
The pathology of inflammatory polyps is:
-Etiology: The cause of inflammatory polyps is inflammatory intestinal conditions, such as ulcerative colitis or Crohn’s disease of the colon, smoking and excess alcohol use, obesity, lack of exercise and fat intake.
-Genes involved: GSE136825, GSE36830.
-Pathogenesis: The sequence of events that lead to inflammatory polyps were derived from polypoid mucosal tags after regeneration and the adjacent mucosa showed regenerative changes and submucosal scarring. The study confirms that ulceration which undermines the muscularis mucosae is the major precursor of inflammatory polyps.
-Histology: The histology associated with inflammatory polyps shows in children are predomination of the inflammatory component represented by granulation tissue.
How does Inflammatory Polyps Present?
Patients with inflammatory polyps typically more in male at 50 years older ages. The symptoms, features, and clinical findings associated with inflammatory polyps include rectal bleeding, change in bowel habits, abdominal pain, and anemia.
How is Inflammatory Polyps Diagnosed?
Inflammatory polyps is diagnosed by colonoscopy, and biopsy.
How is Inflammatory Polyps Treated?
Inflammatory polyps are treated by medications, and removal of polyps.
What is the Prognosis of Inflammatory Polyps?
The prognosis of inflammatory polyps is good. Inflammatory polyps are benign and generally do not carry the risk of developing into colon cancer.
What are Fundic Gland Polyps?
Fundic gland polyps are the most common stomach polyp. They occur in the fundus, or the upper portion of the stomach. When they are found during an endoscopy, there are usually several of them, and they appear as small, smooth flat bumps. These polyps rarely develop into cancer.
What is the Pathology of Fundic Gland Polyps?
The pathology of fundic gland polyps is:
-Etiology: The cause of fundic gland polyps is chronic stomach inflammation.
-Genes involved: beta-catenin gene mutation.
-Pathogenesis: The sequence of events that lead to fundic gland polyps are poorly understood. These lesions have usually been considered hamartomas, although up to 25% of FAP-associated fundic gland polyps and 1% of sporadic types are now known to show foveolar epithelial dysplasia, which is often proceeded by dysregulation of epithelial proliferation.
-Histology: The histology associated with fundic gland polyps shows larger size of dilated fundic gland cysts, larger number of foveolar and mixture type fundic gland cysts, foveolar cell hyperplasia, parietal cell protrusion, mononuclear cell infiltration.
How does Fundic Gland Polyps Present?
Patients with fundic gland polyps typically both genders at any age. The symptoms, features, and clinical findings associated with fundic gland polyps are not usually reported. They are usually found when a patient is being examined for another stomach issue. Larger polyps may cause internal bleeding or abdominal pain.
How is Fundic Gland Polyps Diagnosed?
Fundic gland polyps is diagnosed by endoscopy and biopsy.
How is Fundic Gland Polyps Treated?
Fundic gland polyps is treated by discontinuing proton pump inhibitors or removing the polyp or both.
What is the Prognosis of Fundic Gland Polyps?
The prognosis of fundic gland polyps is good. The lifetime risk of gastric cancer in FAP is estimated to be 0.6–4.2%. Sporadic FGPs have typically been regarded as benign lesions with no risk of malignant transformation; however, some reports have described sporadic FGPs containing low-grade dysplasia.
What are Hyperplastic Polyps?
Hyperplastic polyps are growth of extra cells that projects out from tissues inside your body. They occur in areas where your body has repaired damaged tissue, especially along your digestive tract. Hyperplastic colorectal polyps happen in your colon, the lining of your large intestine.
What is the Pathology of Hyperplastic Polyps?
The pathology of hyperplastic polyps is:
-Etiology: The cause of hyperplastic polyps is strongly linked with disorders that inflame or irritate the stomach, such as chronic gastritis, H. pylori gastritis, and pernicious anemia.
-Genes involved: APC gene mutations.
-Pathogenesis: The sequence of events that lead to hyperplastic polyps are growth of extra cells that projects out from tissues inside your body. They occur in areas where your body has repaired damaged tissue, especially along your digestive tract. Hyperplastic colorectal polyps happen in your colon, the lining of your large intestine.
-Histology: The histology associated with hyperplastic polyps shows superficial location of maximal change, cell elongation, increase in the number and length of microvilli, accentuation of lateral intercellular interdigitations, and an increase in the breadth of basal lamina attachment.
How does Hyperplastic Polyps Present?
Patients with hyperplastic polyps typically men have a greater risk at any age but mostly over 50 years age. The symptoms, features, and clinical findings associated with hyperplastic polyps include rectal bleeding, change in stool color, change in bowel habits, pan and iron deficiency anemia.
How is Hyperplastic Polyps Diagnosed?
Hyperplastic polyps is diagnosed by colonoscopy, CT scan, and biopsy.
How is Hyperplastic Polyps Treated?
Hyperplastic polyps is treated by removing them during a routine endoscopic procedure, eating diet and nutritional changes.
What is the Prognosis of Hyperplastic Polyps?
The prognosis of hyperplastic polyps is good. Getting polyps removed before they become cancerous lowers your risk of developing colorectal or stomach cancer by almost 80 percent.
What are Gastric Tumors?
Gastric tumors are the tumors present at the wall of the stomach which are mostly cancerous and malignant.
Gastric tumours include:
- Gastric adenoma
- Gastric adenocarcinoma
- Gastric carcinoid tumor
- Gastric lymphoma
- Gastrointestinal stromal tumor
What is a Gastric Adenoma?
Gastric adenomas are neoplastic growths characterized by localized, polypoid proliferations of dysplastic epithelium
What is the Pathology of Gastric Adenoma?
The pathology of gastric adenoma is:
-Etiology: The cause of gastric adenoma is unhealthy diet and lifestyle, including high-salt food, smoking and drinking, are able to induce genotypic and phenotypic transformation of gastric epithelial cells.
-Genes involved: Mutation in E-cadherin.
-Pathogenesis: The sequence of events that lead to gastric adenoma are: it is affected by racial, regional, and environmental factors and that its molecular biological pathogenesis involves genetic and epigenetic alteration and histological differentiation; all this leads to various findings within tumors or tumor heterogeneity, suggesting biologically and/or genetically heterogeneous complexity.
-Histology: The histology associated with gastric adenoma shows benign epithelial tumors.
How does Gastric Adenoma Present?
Patients with gastric adenoma typically males mostly at older age. The symptoms, features, and clinical findings associated with gastric adenoma include weight loss, poor appetites, discomfort, abdominal pain, heartburn, nausea, and vomiting.
How is Gastric Adenoma Diagnosed?
Gastric adenoma is diagnosed by upper gastrointestinal series UGI, ultrasounds, MRIs, CT scans and X-rays, and biopsy.
How is Gastric Adenoma Treated?
Gastric adenoma is treated by resection of tumors by endoscopy.
What is the Prognosis of Gastric Adenoma?
The prognosis of gastric adenoma is fair. They are benign epithelial tumors. While some of them remain adenomas for a long time, others progress to carcinomas. However, long-term outcomes of such cases are not entirely clear.
What is a Gastric Adenocarcinoma?
Gastric adenocarcinoma is a malignant epithelial tumour, originating from glandular epithelium of the gastric mucosa.
What is the Pathology of Gastric Adenocarcinoma?
The pathology of gastric adenocarcinoma is:
-Etiology: The cause of gastric adenocarcinoma is multifactorial, more than 80% of cases have been attributed to H. pylori infection. In addition, diet, lifestyle, genetic, socioeconomic and other factors contribute to gastric carcinogenesis.
-Genes involved: E-cadherin mutation.
-Pathogenesis: The sequence of events that lead to gastric adenocarcinoma are: nonmalignant cells involved in the tumor microenvironment play indispensable roles throughout GC pathogenesis. Generally, nonmalignant cells participate in various mechanisms related to GC development, such as stromal interactions, angiogenesis, and some immune responses.
-Histology: The histology associated with gastric adenocarcinoma shows sharply demarcated advancing margins composed of irregular nests or sheets of polygonal tumor cells.
How does Gastric Adenocarcinoma Present?
Patients with gastric adenocarcinoma typically in males as compared to females mostly present at the age range of 50 to 70 years or older. The symptoms, features, and clinical findings associated with gastric adenocarcinoma include pain in the belly, nausea, vomiting, weight loss, weakness, dark stools color, jaundice, and low red blood cells.
How is Gastric Adenocarcinoma Diagnosed?
Gastric adenocarcinoma is diagnosed by blood tests, esophagogastroduodenoscopy, upper gastrointestinal endoscopy, and biopsy.
How is Gastric Adenocarcinoma Treated?
Gastric adenocarcinoma is treated by endoscopic resection, surgery, and chemotherapy.
What is the Prognosis of Gastric Adenocarcinoma?
The prognosis of gastric adenocarcinoma is poor. Long term survival of advanced gastric adenocarcinoma is poor with therapy and even worse without treatment.
What is a Gastric Carcinoid Tumor?
Gastric carcinoid tumors are rare tumors that develop within the gastric mucosa. They can present as an isolated lesion or there can be multiple lesions. The tumor can invade locally into deeper structures of the gastrointestinal GI tract wall.
What is the Pathology of Gastric Carcinoid Tumor?
The pathology of gastric carcinoid tumor is:
-Etiology: The cause of gastric carcinoid tumor is caused by mutations in genes. The develop In neuroendocrine cells.
-Genes involved: MEN1 and MEN2 mutations.
-Pathogenesis: The sequence of events that lead to gastric carcinoid tumor are: In response to persistent achlorhydria, G cells in the gastric antrum undergo hyperplasia, secrete more gastrin and hypergastrinaemia results. Approximately, 5% of patients with autoimmune chronic atrophic gastritis will develop a gastric carcinoid tumour.
-Histology: The histology associated with gastric carcinoid tumor shows sbnormal glands with neoplastic cells.
How does Gastric Carcinoid Tumor Present?
Patients with gastric carcinoid tumor typically women present at age range of 55 to 65 years. The symptoms, features, and clinical findings associated with gastric carcinoid tumor include: diarrhea, abdominal pain, vomiting, nausea, rectal bleeding, rectal pain.
How is Gastric Carcinoid Tumor Diagnosed?
Gastric carcinoid tumor is diagnosed by blood and urine tests, levels of 5-HIAA in a urine sample collected over 24 hours, blood tests for chromogranin A and gastrin.
How is Gastric Carcinoid Tumor Treated?
Gastric carcinoid tumor is treated by excision endoscopically or surgically, Antrectomy, by eliminating the trophic effect of gastrin, radiation therapy, chemotherapy, and hormone therapy.
What is the Prognosis of Gastric Carcinoid Tumor?
The prognosis of gastric carcinoid tumor is good. Carcinoid tumors usually grow slowly over many years. Surgically treated patients with carcinoid tumor have an overall favorable 83% 5-year survival rate.
What is a Gastric Lymphoma?
Gastric lymphoma is a general term for a type of cancer that originates within the stomach. Approximately 90 percent of patients of primary gastric lymphoma are either mucosa-associated lymphoid tissue MALT gastric lymphoma or diffuse large B-cell lymphoma DLBCL of the stomach.
What is the Pathology of Gastric Lymphoma?
The pathology of gastric lymphoma is:
-Etiology: The cause of gastric lymphoma is unknown. However, a strong association between infection with Helicobacter pylori H. pylori and the development of MALT gastric lymphoma has been established.
-Genes involved: CDH1.
-Pathogenesis: The sequence of events that lead to gastric lymphoma are: Pathogenesis is often related to Helicobacter pylori infection. When these cells are continuously stimulated by H pylori, they can give rise to lymphomas. In addition to B cells, T cells and macrophages play an important role in MALT lymphomagenesis.
-Histology: The histology associated with gastric lymphoma shows lymphoepithelial lesions formed by the invasion of individual crypts by aggregates.
How does Gastric Lymphoma Present?
Patients with gastric lymphoma typically in males present at age range of 60-65 years. The symptoms, features, and clinical findings associated with gastric lymphoma include unintended weight loss, fatigue, low levels of circulating red blood cells anemia, abdominal and/or back pain, loss of appetite anorexia, nausea, vomiting, and/or constipation. In some cases, it may be possible to feel a mass in the abdomen.
How is Gastric Lymphoma Diagnosed?
Gastric lymphoma is diagnosed by biopsy at the time of endoscopy, blood tests, bone marrow aspirates, and specialized imaging tests.
How is Gastric Lymphoma Treated?
Gastric lymphoma is treated by antibiotic therapy, surgery, chemotherapy, and radiation therapy. These treatments may be used alone or in varied combinations.
What is the Prognosis of Gastric Lymphoma?
The prognosis of gastric lymphoma is good. Low-grade gastric lymphomas involving the mucosa and submucosal layers carry a favorable prognosis with up to 90% survival at 10 years.
What is a Gastrointestinal Stromal Tumor?
Gastrointestinal Stromal Tumor also known as GIST, is type of tumor that occurs in the gastrointestinal tract, most commonly in the stomach or small intestine. This type of tumor is thought to grow from specialized cells found in the gastrointestinal tract.
What is the Pathology of Gastrointestinal Stromal Tumor?
The pathology of gastrointestinal stromal tumor is:
-Etiology: The cause of gastrointestinal stromal tumor is unknown, though they seem to be related to a mutation in the expression of the KIT protein.
-Genes involved: KIT gene, PDGFRA gene.
-Pathogenesis: The sequence of events that lead to gastrointestinal stromal tumor are: When there are mutations in the PDGFRA and KIT genes, these can cause the proteins to no longer require ligand binding to the stimulated and activated. In turn, the proteins and the signaling pathway is turned on consistently, leading to uncontrolled cell growth, and eventually, GIST development.
-Histology: The histology associated with gastrointestinal stromal tumor shows spindled, epithelioid, or mixed spindled and epithelioid type. The most common is spindle cell type. Nuclear pleomorphism can be seen especially in epithelioid cell type.
How does Gastrointestinal Stromal Tumor Present?
Patients with gastrointestinal stromal tumor typically men present at 50 years or older age. The symptoms, features, and clinical findings associated with gastrointestinal stromal tumor include: blood in stool, abdominal pain, pain while swallowing, tiredness, feeling full after eating little.
How is Gastrointestinal Stromal Tumor Diagnosed?
Gastrointestinal stromal tumor is diagnosed by CT scan, x-rays, Endoscopies, colonoscopies, and biopsy. Routine blood tests and stool tests may be useful.
How is Gastrointestinal Stromal Tumor Treated?
Gastrointestinal stromal tumor is treated by surgical removal and Tyrosine kinase inhibitors.
What is the Prognosis of Gastrointestinal Stromal Tumor?
The prognosis of gastrointestinal stromal tumor is good.
What is Small Intestine Pathology and Colon Pathology?
Small intestine pathology is the science of the causes and effects of diseases of small intestine which include inflammatory bowel disease and Crohn’s disease.
What is Intestinal Obstruction?
Intestinal obstruction is significant mechanical impairment or complete arrest of the passage of contents through the intestine due to pathology that causes blockage of the bowel.
Examples of conditions that may cause intestinal obstruction include:
- Adhesions
- Hernias
- Intussusception
- Volvulus
What are Adhesions?
Adhesions are bands of scar tissue that form between abdominal organs, mainly the small intestine. Adhesions occur after abdominal surgery and can cause your tissues to stick together.
What is the Pathology of Intestinal Adhesions?
The pathology of intestinal adhesions is:
-Etiology: The cause of intestinal adhesions is tissue incisions, contact of internal tissues with foreign materials, such as gauze, surgical gloves, and stitches.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to intestinal adhesions are: bands of fibrous tissue in the abdominal cavity that can form after abdominal or pelvic surgery, the inflammation occurs on the surface of the organ; the formation of scar tissue is a normal part of healing during inflammation. The fibrous bands are formed between tissues and organs.
-Histology: The histology associated with intestinal adhesions shows sticked scar tissues together.
How does Intestinal Adhesions Present?
Patients with intestinal adhesions typically in all genders present at any age. The symptoms, features, and clinical findings associated with intestinal adhesions include constipation, blotting, abdominal pain, nausea, and vomiting.
How is Intestinal Adhesions Diagnosed?
Intestinal adhesions is diagnosed by laparoscopy, and cannot be detected by tests or seen through imaging techniques such as x rays or ultrasound.
How is Intestinal Adhesions Treated?
Intestinal adhesions are typically not treated unless they are complications. If abdominal adhesions cause symptoms or complications, doctors can release the adhesions with laparoscopic or open surgery.
What is the Prognosis of Intestinal Adhesions?
The prognosis of intestinal adhesions is good but if adhesions cause intestinal obstruction, which then they could be life-threatening.
What are Hernias?
Hernias are tear in muscle or tissue that allows part of insides to bulge out. It can be a bulge of an internal organ or the intestines.
What is the Pathology of Hernias?
The pathology of hernias is:
-Etiology: The cause of hernias is a combination of pressure and an opening or weakness of muscle or fascia; the pressure pushes an organ or tissue through the opening or weak spot. Sometimes the muscle weakness is present at birth; more often, it occurs later in life.
-Genes involved: WT1, EFEMP1, EBF2 and ADAMTS6.
-Pathogenesis: The sequence of events that lead to hernias are: It occurs as a result of the deep inguinal ring failing to close during embryogenesis after a testicle has moved through it. Once bowel or other abdominal tissue moves into and enlarges the empty space, a visible bulge forms and the hernia becomes clinically evident.
-Histology: The histology associated with hernias shows Incarceration, obstruction and strangulation.
What are the Different types of Hernias?
Different types of hernias include:
- Epigastric hernia which occurs in the epigastric region of the abdomen above the belly button and below the rib cage.
- Femoral hernia which occurs when tissue pushes through a weak point in the groin or inner thigh.
- Hiatal hernia occurs when a person’s stomach bulges through a weak point in the diaphragm.
- Incisional hernia occurs when a person has stomach surgery. It usually involves an incision down the middle of the stomach. If the surgical wound doesn’t heal completely, that person can be more vulnerable to developing a hernia.
- Inguinal hernia occurs when a portion of intestine or fat bulges through the lower stomach wall.
- Umbilical hernia occurs when tissues in the body bulge through an area of weakness in the belly button area.
How does Hernias Present?
Patients with hernias typically men at adult life mostly but some types of hernias could develop from age 0 to 5 years old. The symptoms, features, and clinical findings associated with hernias include: visible bulge in the affected area. Other reported symptoms include pressure, a cough, heartburn, and difficulty swallowing. Severe hernia symptoms are shooting pain, vomiting, and constipation.
How is Hernias Diagnosed?
Hernias is diagnosed by physical exam, and possibly imaging tests including MRI Scans.
How is Hernias Treated?
Hernias is treated by surgery.
What is the Prognosis of Hernias?
The prognosis of hernias is excellent. They do reappear, however, in about 10 percent of adults.
What is Intussusception?
Intussusception is a serious condition in which part of the intestine slides into an adjacent part of the intestine and blocks food or fluid from passing through and sometimes blood supply.
What is the Pathology of Intussusception?
The pathology of intussusception is:
-Etiology: The cause of intussusception is unknown. However, it is considered to be accidental. In most cases, it is preceded by a virus that produces swelling of the lining of the intestine, which then slips into the intestine below.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to intussusception are: imbalance between the forces of radial and smooth muscles which leads to a segment of intestine to invaginate into another leading to intussusception.
-Histology: The histology associated with intussusception shows a right hypochondrium sausage-shaped mass and emptiness in the right lower quadrant.
How does Intussusception Present?
Patients with intussusception typically in boys present at ages of three and 36 months, but may appear at any age. The symptoms, features, and clinical findings associated with intussusception include: stool mixed with blood and mucus, vomiting, lump in abdomen, diarrhea, and fatigue.
How is Intussusception Diagnosed?
Intussusception is diagnosed by Ultrasound or other abdominal imaging. including X-ray or CT scan.
How is Intussusception Treated?
Intussusception is treated by surgery.
What is the Prognosis of Intussusception?
The prognosis of intussusception is excellent if treated quickly, but if untreated it can lead to death within two to five days. The longer the intestine segment is prolapsed and the longer it goes without a blood supply, the less effective a non-surgical reduction.
What is Volvulus?
Volvulus is a condition in which the bowel twists on itself, causing obstruction to the flow of material through the bowel. It can also lead to obstruction of the blood supply to the intestine itself, which can result in tissue death within the bowel.
What is the Pathology of Volvulus?
The pathology of volvulus is:
-Etiology: The cause of volvulus is an increase in the span of the sigmoid colon, such as chronic constipation, infections, neuropsychiatric disorders, and electrolyte abnormalities.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to volvulus are: When the bowel loop is overloaded with material, it becomes susceptible to torsion along the axis of an elongated mesentery. A large pelvic mass or a large gravid uterus can alter the position of the intra-abdominal organs, predisposing to the formation of volvulus.
-Histology: The histology associated with volvulus shows bent inner tube sign with the apex of the volvulus located in the left upper quadrant.
How does Volvulus Present?
Patients with volvulus typically male and present in adults between the ages of 50 and 80. The symptoms, features, and clinical findings associated with volvulus include: Abdominal tenderness, nausea or vomiting, bloody or dark red stool, constipation, and disintended abdomen.
How is Volvulus Diagnosed?
Disease in sentence case is diagnosed by medical imaging such as plain X-rays, a GI series, or CT scan.
How is Volvulus Treated?
Volvulus is treated by surgery to correct a volvulus.
What is the Prognosis of Volvulus?
The prognosis of volvulus is poor unless treated.
What is Ischemic Bowel Disease?
Ischemic bowel disease is a lack of blood flow to the bowel temporarily, usually due to constriction of the blood vessels supplying the colon or lower flow of blood through the vessels due to low pressures.
What is the Pathology of Ischemic Bowel Disease?
The pathology of ischemic bowel disease is:
-Etiology: The cause of ischemic bowel disease is blockage in an artery caused by a blood clot, or a narrowing of an artery due to buildup of deposits, such as cholesterol.
-Genes involved: NOD2/CARD15, TNFSF15, ATG16L1, IL23R, and IRGM.
-Pathogenesis: The sequence of events that lead to ischemic bowel disease are: heterogeneous group of disorders caused by acute or chronic processes, arising from occlusive or nonocclusive etiologies, which result in decreased blood flow to the gastrointestinal tract. The clinical course may range from transient and reversible to fulminant.
-Histology: The histology associated with ischemic bowel disease shows bowel wall thickening.
How does Ischemic bowel disease Present?
Patients with ischemic bowel disease typically women of older ages older than 60 years. The symptoms, features, and clinical findings associated with ischemic bowel disease include: Abdominal cramps or fullness, abdominal pain, bloating, weight loss, diarrhea, nausea.
How is Ischemic Bowel Disease Diagnosed?
Ischemic bowel disease is diagnosed by Colonoscopy, blood tests, X-ray, ultrasound, CT scan and MRI.
How is Ischemic Bowel Disease Treated?
Ischemic bowel disease is treated by antibiotics and/or medications to prevent or treat clots. Surgery may also be indicated.
What is the Prognosis of Ischemic Bowel Disease?
The prognosis of ischemic bowel disease is good if treated. Nearly all people with ischemic colitis improve and recover over a period of 1 to 2 weeks. However, when the interruption to the blood supply is more severe or more prolonged, the affected portion of the large intestine may have to be surgically removed.
What is Angiodysplasia?
Angiodysplasia is an abnormal, tortuous, dilated small blood vessel in the mucosal and submucosal layers of the GI tract.
What is the Pathology of Angiodysplasia?
The pathology of angiodysplasia is:
-Etiology: The cause of angiodysplasia is unknown. But normal spasms occurring in the GI tract may be responsible for the enlargement of blood vessels. This enlargement leads to the development of small pathways between a vein and an artery, which can leak with blood.
-Genes involved: mutations in ACVRL1; ALK1, SMAD4 genes.
-Pathogenesis: The sequence of events that lead to angiodysplasia are: age and strain on the bowel wall. It is a degenerative lesion, acquired, probably resulting from chronic and intermittent contraction of the colon that is obstructing the venous drainage of the mucosa.
-Histology: The histology associated with angiodysplasia shows vascular lesion of the gastrointestinal tract.
How does Angiodysplasia Present?
Patients with angiodysplasia typically in all genders older than 60 years. The symptoms, features, and clinical findings associated with angiodysplasia include: shortness of breath, tiredness, weakness, pale skin, lightheadedness, dizziness, fast heartbeat.
How is Angiodysplasia Diagnosed?
Angiodysplasia is diagnosed by endoscopy, either colonoscopy or esophagogastroduodenoscopy EGD.
How is Angiodysplasia Treated?
Angiodysplasia is treated by surgical resection.
What is the Prognosis of Angiodysplasia?
The prognosis of angiodysplasia is fair.
What is Malabsorption?
Malabsorption is difficulty in the digestion or absorption of nutrients from food. Malabsorption can affect growth and development, or it can lead to specific illnesses.
What is the Pathology of Malabsorption?
The pathology of malabsorption is:
-Etiology: The cause of malabsorption is damage to the intestine from infection, inflammation, trauma, or surgery. prolonged use of antibiotics.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to malabsorption are physiological digestion and absorption of nutrients within the gastrointestinal tract requires a complex interaction between motor, secretory, digestive, and absorptive functions that is vulnerable to a multitude of potential disturbances which may lead to global or specific malabsorption syndromes.
-Histology: The histology associated with malabsorption shows autoantibodies for islet and parietal cells.
How does Malabsorption Present?
Patients with malabsorption typically men present at older ages. The symptoms, features, and clinical findings associated with malabsorption include: bloating and stomach distention, diarrhea, fatigue, gas, steatorrhea, or stool that is pale to white, stools that appear “greasy” in texture, stomach cramping, weakness.
How is Malabsorption Diagnosed?
Malabsorption is diagnosed by a stool test, complete blood cell count, and iron tests.
How is Malabsorption Treated?
Malabsorption is treated with vitamin supplements, enzyme supplements, and diet changes.
What is the Prognosis of Malabsorption?
The prognosis of malabsorption is good. Malabsorption may be temporary. Complications are directly related to the type of nutrient not being absorbed. In some cases, people get persistent diarrhea, weight loss, and abdominal pain.
What is Abetalipoproteinemia?
Abetalipoproteinemia is an inherited disorder that impairs the normal absorption of fats and certain vitamins from the diet
What is the Pathology of Abetalipoproteinemia?
The pathology of abetalipoproteinemia is:
-Etiology: The cause of abetalipoproteinemia is by mutations in the MTTP gene, which provides instructions for making a protein called microsomal triglyceride transfer protein. This protein is essential for creating molecules called beta-lipoproteins in the liver and intestine.
-Genes involved: MTTP gene.
-Pathogenesis: The sequence of events that lead to abetalipoproteinemia are: mutations in the gene encoding a subunit of a microsomal triglyceride transfer protein. As a consequence, circulating apoprotein B‐containing lipoproteins are almost completely missing, and the patients are unable to absorb and transport fat and fat‐soluble vitamins.
-Histology: The histology associated with abetalipoproteinemia shows marked fat vacuoles in apical villous cytoplasm, and normal villi.
How does Abetalipoproteinemia Present?
Patients with disease in lower case typically both males and females present at any age. The symptoms, features, and clinical findings associated with abetalipoproteinemia include failure to gain weight and grow at the expected rate failure to thrive; diarrhea; and fatty, foul-smelling stools steatorrhea.
How is Abetalipoproteinemia Diagnosed?
Abetalipoproteinemia is diagnosed by laboratory tests showing abnormally low cholesterol, and confirmed by genetic testing.
How is Abetalipoproteinemia Treated?
Abetalipoproteinemia is treated by low fat diet and large doses of fat-soluble vitamin.
What is the Prognosis of Abetalipoproteinemia?
The prognosis of abetalipoproteinemia is good. Most individuals with this condition are treated with excess vitamins and a special, fat-controlled diet and have few complications. Untreated individuals with abetalipoproteinemia can develop gradual vision loss, muscle weakness, tremors, and slow or slurred speech that gets worse over time.
What is Autoimmune Enteropathy?
Autoimmune enteropathy is a rare condition that causes children to have a lot of diarrheas, often to the point of needing intravenous IV fluids. Autoimmune enteropathy can also affect a child’s ability to absorb food and vitamins.
What is the Pathology of Autoimmune Enteropathy?
The pathology of autoimmune enteropathy is:
-Etiology: The cause of autoimmune enteropathy is when the body’s own immune system attacks itself, and irritates or inflames the lining of the intestine. Sometimes this is a problem only with the bowel or intestines; sometimes the body attacks itself in other places such as the thyroid or other glands in the body.
-Genes involved: FOXP3 and alpha chain of the interleukin-2 receptor genes.
-Pathogenesis: The sequence of events that lead to autoimmune enteropathy are: Exact pathogenesis is unclear. Intestinal epithelial damage from anti-enterocyte antibodies and antigoblet cell antibodies lead to the disaese.
-Histology: The histology associated with autoimmune enteropathy shows celiac-like changes.
How does Autoimmune Enteropathy Present?
Patients with autoimmune enteropathy typically in all genders present at early ages of life. The symptoms, features, and clinical findings associated with autoimmune enteropathy include diarrhea, weight loss, decreased urine output, frequent infections, occasional blood in the stool, and skin rash.
How is Autoimmune Enteropathy Diagnosed?
Autoimmune enteropathy is diagnosed by antinuclear antibody test ANA, endoscopy, and biopsy.
How is Autoimmune Enteropathy Treated?
Autoimmune enteropathy is treated by long-term immunosuppression, steroid-sparing treatment strategies, special diet, intravenous nutrirtion.
What is the Prognosis of Autoimmune Enteropathy?
The prognosis of autoimmune enteropathy is fair. The prognosis of autoimmune enteropathy patients depends on the severity of digestive symptoms including fecal output, on the severity and extension of histological lesions along the gastrointestinal apparatus, and on the presence of extra-intestinal involvement.
What is Celiac Disease?
Celiac disease is a digestive and autoimmune disorder that can damage your small intestine. Celiac disease can be triggered by a protein called gluten. Gluten is found in grains, like wheat, barley and rye.
What is the Pathology of Celiac Disease?
The pathology of celiac disease is:
-Etiology: The cause of celiac disease is by sensitivity to the gliadin fraction of gluten. In a genetically susceptible person, gluten-sensitive T cells are activated when gluten-derived peptide epitopes are presented.
-Genes involved: HLA-DQA1 and HLA-DQB1 genes.
-Pathogenesis: The sequence of events that lead to celiac disease are: activation of both a cell-mediated T-cell and humoral B-cell immune response resulted from exposure to the glutens. Transglutaminase deamidates gliadin which results in greater proliferative response of gliadin-specific T-cells that lead to mucosal inflammation and further B-cell activation in patients with the disease.
-Histology: The histology associated with celiac disease shows intraepithelial lymphocytosis, lamina propria inflammation and villous atrophy.
How does Celiac Disease Present?
Patients with celiac disease typically in women at any age from infancy well into senior adulthood. The symptoms, features, and clinical findings associated with celiac disease include diarrhea, fatigue, weight loss, bloating and gas, abdominal pain, nausea and vomiting, and constipation.
How is Celiac Disease Diagnosed?
Celiac disease is diagnosed by Serology testing looks for antibodies, Genetic testing for human leukocyte antigens, intestinal biopsy.
How is Celiac Disease Treated?
Celiac disease is treated by following a gluten-free diet.
What is the Prognosis of Celiac Disease?
The prognosis of celiac disease is fair. Overall, people with untreated or unresponsive celiac disease have increased early mortality compared to the general population.
What is Cystic Fibrosis?
Cystic fibrosis is an inherited disorder that causes severe damage to the lungs, digestive system and other organs in the body. Cystic fibrosis affects the cells that produce mucus, sweat and digestive fluids.
What is the Pathology of Cystic Fibrosis?
The pathology of cystic fibrosis is:
-Etiology: The cause of cystic fibrosis is mutations in a gene called the cystic fibrosis transmembrane conductance regulator CFTR gene.
-Genes involved: CFTR gene mutation.
-Pathogenesis: The sequence of events that lead to cystic fibrosis are: mutation in gene causes production of a protein that does not fold normally and is not appropriately transported to the cell membrane, resulting in its degradation.
-Histology: The histology associated with cystic fibrosis shows hyperplasia of mucous cells, increased numbers of pulmonary neuroendocrine and indeterminate cells, degeneration and sloughing of epithelial cells.
How does Cystic Fibrosis Present?
Patients with cystic fibrosis typically present during childhood. The diagnosis after 30 to 60 years is rare. The symptoms, features, and clinical findings associated with cystic fibrosis include salty-tasting skin, persistent coughing, frequent lung infections, poor weight gain in spite of a good appetite, and frequent greasy bulky stools. Nasal polyps may also be present.
How is Cystic Fibrosis Diagnosed?
Cystic fibrosis is diagnosed by sweat test, genetic tests, blood sample to check for higher levels of a chemical called immunoreactive trypsinogen.
How is Cystic Fibrosis Treated?
Cystic fibrosis is treated by antibiotics to treat and prevent lung infections. Anti-inflammatory medications to lessen swelling in the airways in your lungs. Mucus-thinning drugs, such as hypertonic saline, to help you cough up the mucus, which can improve lung function.
What is the Prognosis of Cystic Fibrosis?
The prognosis of cystic fibrosis is not good. It tends to get worse over time and can be fatal if it leads to a serious infection or the lungs stop working properly.
What is Lactase Deficiency?
Lactase deficiency is due to an insufficient level of lactase, which hydrolyzes lactose into glucose and galactose.
What is the Pathology of Lactase Deficiency?
The pathology of lactase deficiency is:
-Etiology: The cause of lactase deficiency is an inherited genetic fault that runs in families.
-Genes involved: LCT gene mutation.
-Pathogenesis: The sequence of events that lead to lactase deficiency are: A deficiency of intestinal lactase prevents hydrolysis of ingested lactose. The osmotic load of the unabsorbed lactose causes secretion of fluid and electrolytes until osmotic equilibrium is reached. Dilation of the intestine caused by the osmosis induces an acceleration of small intestinal transit, which increases the degree of maldigestion.
-Histology: The histology associated with lactase deficiency shows normal villi.
How does Lactase Deficiency Present?
Patients with lactase deficiency typically women present at age range of 25 to 30 years. The symptoms, features, and clinical findings associated with lactase deficiency include diarrhea.
How is Lactase Deficiency Diagnosed?
Lactase deficiency is diagnosed by hydrogen breath test, lactose tolerance blood test, and small bowel biopsy.
How is Lactase Deficiency Treated?
Lactase deficiency is treated by lactase tablets, and limiting milk and other dairy products.
What is the Prognosis of Lactase Deficiency?
The prognosis of lactase deficiency is excellent. Most patients have a considerable improvement in signs and symptoms with dietary modification alone.
What is Disaccharidase Deficiency?
Disaccharidase deficiency involves decreased hydrolysis of the disaccharides double-sugars by the disaccharidase enzymes lactase; maltase-glucoamylase; sucrase-isomaltase; palatinase and trehalase.
What is the Pathology of Disaccharidase Deficiency?
The pathology of disaccharidase deficiency is:
-Etiology: The cause of disaccharidase deficiency is autoimmune disorder that is triggered by hypersensitivity to ingested gliadins from wheat and other cereals, due to genetic variations.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to disaccharidase deficiency are: A deficiency of an intestinal disaccharidase prevents hydrolysis of ingested substrate, a disaccharide. The osmotic load of the unabsorbed disaccharide causes secretion of fluid and electrolytes until osmotic equilibrium is reached. Dilation of the intestine caused by the osmosis induces an acceleration of small intestinal transit, which increases the degree of maldigestion.
-Histology: The histology associated with disaccharidase deficiency shows reactive epithelial changes in distal end of small intestine.
How does Disaccharidase Deficiency Present?
Patients with disaccharidase deficiency typically in all genders present at any age. The symptoms, features, and clinical findings associated with disaccharidase deficiency include: abdominal pain, bloating, and flatulence. A less common but still frequent symptom is diarrhea.
How is Disaccharidase Deficiency Diagnosed?
Disaccharidase deficiency is diagnosed by biopsies during upper endoscopy, direct assessment of enzyme activity spectrophotometry, fluorescence, and radiolabeling.
How is Disaccharidase Deficiency Treated?
Disaccharidase deficiency is treated by Complete dietary elimination of the symptom causing disaccharidase is curative, enzyme supplementation for specific enzyme.
What is the Prognosis of Disaccharidase Deficiency?
The prognosis of disaccharidase deficiency is good. Most patients have a considerable improvement in signs and symptoms with dietary modification alone.
What is Diarrhea?
Diarrhea is frequent, loose, and watery bowel movements.
Conditions that may cause diarrhea include:
- Infectious enterocolitis
- Campylobacter enterocolitis
- Escherichia coli
- Parasitic enterocolitis
- Pseudomembranous colitis
- Salmonella
- Shigellosis
- Typhoid fever
- Whipple disease
- Viral gastroenteritis
- Yersinia
What is Infectious Enterocolitis?
Infectious enterocolitis is bowel inflammation caused by bacteria, viruses, or parasites. A key radiologic feature of infectious enterocolitis is the distribution of inflammation produced by the offending organism.
What is the Pathology of Infectious Enterocolitis?
The pathology of infectious enterocolitis is:
-Etiology: The cause of infectious enterocolitis is food poisoning. You can get it after ingesting food or water that is contaminated with bacteria.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to infectious enterocolitis are: direct bacterial or indirect bacterial toxin invasion of the colonic mucosa, leading to toxicity, volume loss, hemorrhage, and colonic inflammation.
-Histology: The histology associated with infectious enterocolitis shows immune cells in the lining of the tissue.
How does Infectious Enterocolitis Present?
Patients with infectious enterocolitis typically in all genders at any age. The symptoms, features, and clinical findings associated with infectious enterocolitis include: cramps and bloating, the urge to use the bathroom more frequently, watery diarrhea, fever, tiredness.
How is Infectious Enterocolitis Diagnosed?
Infectious enterocolitis is diagnosed by fever and/or dysentery, stools containing inflammatory markers such as leukocytes, lactoferrin, or calprotectin, or positive stool culture for an invasive or inflammatory bacterial enteropathogen including Shigella, and Salmonella.
How is Infectious Enterocolitis Treated?
Infectious enterocolitis is treated by therapy of broad-spectrum antibiotics and IV fluid resuscitation.
What is the Prognosis of Infectious Enterocolitis?
The prognosis of infectious enterocolitis is good. For most people, symptoms go away within a few days. Recovery can take two to three weeks in more severe cases depending on the cause.
What is Campylobacter Enterocolitis?
Campylobacter enterocolitis is a common cause of intestinal infection. These bacteria are also one of the many causes of traveler’s diarrhea or food poisoning.
What is the Pathology of Campylobacter Enterocolitis?
The pathology of campylobacter enterocolitis is:
-Etiology: The cause of campylobacter enterocolitis is eating raw or undercooked poultry or eating something that touched it.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to campylobacter enterocolitis
-Histology: The histology associated with campylobacter enterocolitis shows campylobacter.
How does Campylobacter Enterocolitis Present?
Patients with disease in lower case typically all genders at any age. The symptoms, features, and clinical findings associated with campylobacter enterocolitis include bloody diarrhea, fever, and stomach cramps.
How is Campylobacter Enterocolitis Diagnosed?
Campylobacter enterocolitis is diagnosed by laboratory test detects Campylobacter bacteria in stool, body tissue, or fluids.
How is Campylobacter Enterocolitis Treated?
Campylobacter enterocolitis is treated by Azithromycin therapy.
What is the Prognosis of Campylobacter enterocolitis?
The prognosis of campylobacter enterocolitis is excellent. Most people recover from infection without antibiotic treatment.
What is Escherichia coli?
Escherichia coli is a type of bacteria that normally lives in your intestines. It’s also found in the gut of some animals. Most types of E. coli are harmless and even help keep the digestive tract healthy.
What is Parasitic Enterocolitis?
Parasitic enterocolitis is an inflammation that occurs in a person’s digestive tract with parasites infections.
What is the Pathology of Parasitic Enterocolitis?
The pathology of parasitic enterocolitis is:
-Etiology: The cause of parasitic enterocolitis is Entamoeba histolytica which the most common cause of parasitic colitis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to parasitic enterocolitis.
-Histology: The histology associated with parasitic enterocolitis shows.
How does Parasitic Enterocolitis Present?
Patients with parasitic enterocolitis typically all genders at any age. The symptoms, features, and clinical findings associated with parasitic enterocolitis include abdominal pain and bloating, bloody stools, dehydration, diarrhea, and fever.
How is Parasitic Enterocolitis Diagnosed?
Parasitic enterocolitis is diagnosed by fecal exam, endoscopy, colonoscopy, blood tests, X-ray, and MRI.
How is Parasitic Enterocolitis Treated?
Parasitic enterocolitis is treated by albendazole and mebendazole.
What is the Prognosis of Parasitic Enterocolitis?
The prognosis of parasitic enterocolitis is good because they could easily be treated and prevented.
What is Pseudomembranous Colitis?
Pseudomembranous colitis is inflammation swelling, irritation of the large intestine. In many cases, it occurs after taking antibiotics. Using antibiotics can cause the bacterium Clostridium difficile C. diff to grow and infect the lining of the intestine, which produces the inflammation.
What is the Pathology of Pseudomembranous Colitis?
The pathology of pseudomembranous colitis is:
-Etiology: The cause of pseudomembranous colitis is antibiotics.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pseudomembranous colitis are: pathognomonic of infection by toxin-producing Clostridium difficile and develops as a result of altered normal microflora usually by antibiotic therapy that favors overgrowth and colonization of the intestine by Clostridium difficile and production of its toxins.
-Histology: The histology associated with pseudomembranous colitis shows whitish plaques attached to mucosa.
How does Pseudomembranous Colitis Present?
Patients with pseudomembranous colitis typically all genders at any age. The symptoms, features, and clinical findings associated with pseudomembranous colitis include diarrhea, abdominal cramps, pain or tenderness, fever, mucus in the stool, nausea, and dehydration.
How is Pseudomembranous Colitis Diagnosed?
Pseudomembranous colitis is diagnosed by examining a sample of feces in a laboratory to identify toxins produced by bacteria.
How is Pseudomembranous Colitis Treated?
Pseudomembranous colitis is treated by metronidazole, vancomycin, or fidaxomicin.
What is the Prognosis of Pseudomembranous Colitis?
The prognosis of pseudomembranous colitis is good. Most patients will experience complete recovery within 10 days.
What is Salmonella?
Salmonella is a type of bacteria that can affect the intestinal tract.
What is the Pathology of Salmonellosis?
The pathology of salmonellosis is:
-Etiology: The cause of salmonellosis is food poisoning.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to salmonellosis are: ingested in food survive passage through the gastric acid barrier and invade the mucosa of the small and large intestine and produce toxins. Invasion of epithelial cells stimulates the release of proinflammatory cytokines which induce an inflammatory reaction.
-Histology: The histology associated with salmonellosis shows enteropathy.
How does Salmonellosis Present?
Patients with Salmonellosis typically all genders at all ages. The symptoms, features, and clinical findings associated with salmonellosis include diarrhea, fever, and stomach cramps.
How is Salmonellosis Diagnosed?
Salmonellosis is diagnosed by testing a sample of stool, body tissue, or fluids.
How is Salmonellosis Treated?
Salmonellosis is treated by fluoroquinolones for adults and azithromycin for children.
What is the Prognosis of Salmonellosis?
The prognosis of salmonellosis is very good. it is a self-limiting disease in most patients. Even immunosuppressed patients can do well if the disease is diagnosed and treated promptly.
What is Shigellosis?
Shigellosis is an intestinal infection caused by a family of bacteria known as shigella.
What is the Pathology of Shigellosis?
The pathology of shigellosis is:
-Etiology: The cause of shigellosis is the Shigella bacteria
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to shigellosis are: fewer than 100 bacterial cells can be enough to cause an infection. Shigella species generally invade the epithelial lining of the colon, causing severe inflammation and death of the cells lining the colon.
-Histology: The histology associated with shigellosis shows bacteria.
How does Shigellosis Present?
Patients with shigellosis typically all genders at all ages. The symptoms, features, and clinical findings associated with shigellosis include fever, bloody diarrhea, and cramps.
How is Shigellosis Diagnosed?
Shigellosis is diagnosed by laboratory identification of Shigella in the stool poop of an ill person.
How is Shigellosis Treated?
Shigellosis is treated by ciprofloxacin and azithromycin which are recommended oral antibiotics.
What is the Prognosis of Shigellosis?
The prognosis of shigellosis is good. Most people with shigellosis feel better in 4–7 days, but may still be contagious for up to 2 weeks after they recover.
What is Typhoid Fever?
Typhoid fever is a bacterial infection that can spread throughout the body, affecting many organs. Without prompt treatment, it can cause serious complications and can be fatal. It’s caused by a bacterium called Salmonella typhi.
What is the Pathology of Typhoid Fever?
The pathology of typhoid fever is:
-Etiology: The cause of typhoid fever is Salmonella enterica.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to typhoid fever are: the intake of bacteria with contaminated food consequently ingested and the infectious bacteria taken up by macrophages towards lymph nodes where they multiply and enter blood stream at the end of incubation period hence causing fever.
-Histology: The histology associated with typhoid fever shows sinusoids are enlarged and distended by large collections of macrophages and reticuloendothelial cells.
How does Typhoid Fever Present?
Patients with typhoid fever typically in all genders at any age. The symptoms, features, and clinical findings associated with typhoid fever include: High fever, headache, Stomach pain, Constipation or diarrhea.
How is Typhoid Fever Diagnosed?
Typhoid fever is diagnosed analysing samples of blood, stool, or urine.
How is Typhoid Fever Treated?
Typhoid fever is treated by Ciprofloxacin, Azithromycin, Ceftriaxone
What is the Prognosis of Typhoid Fever?
The prognosis of typhoid fever is good. Generally, untreated typhoid fever carries a mortality rate of 15%-30%. In properly treated disease, the mortality rate is less than 1%.
What is Whipple Disease?
Whipple disease is rare bacterial infection that most often affects your joints and digestive system. Whipple disease interferes with normal digestion by impairing the breakdown of foods, and hampering your body’s ability to absorb nutrients, such as fats and carbohydrates.
What is the Pathology of Whipple Disease?
The pathology of whipple disease is:
-Etiology: The cause of Whipple disease is type of bacterium called Tropheryma whipplei.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to whipple disease are: The bacteria affect the mucosal lining of your small intestine first, forming small sores lesions within the wall of the intestine. The bacteria also damage the fine, hairlike projections villi that line the small intestine.
-Histology: The histology associated with whipple disease shows mesenteric lymph nodes and large, foamy macrophages.
How does Whipple Disease Present?
Patients with whipple disease typically in all genders at all ages. The symptoms, features, and clinical findings associated with whipple disease include: Fever. Cough. Enlarged lymph nodes, Difficulty walking, Vision problems, including lack of control of eye movements, Confusion, Memory loss.
How is Whipple Disease Diagnosed?
Whipple disease is diagnosed by PCR to detect bacteria in biopsy specimens or spinal fluid samples, Blood tests such as CBC.
How is Whipple Disease Treated?
Whipple disease is treated by antibiotics.
What is the Prognosis of Whipple Disease?
The prognosis of whipple disease is poor If Whipple disease is untreated. If this condition is treated for a full year, the prognosis usually is good. Clinical remission occurs in approximately 70% of patients.
What is Viral Gastroenteritis?
Viral gastroenteritis is an intestinal infection marked by watery diarrhea, abdominal cramps, nausea or vomiting, and sometimes fever.
What is the Pathology of Viral Gastroenteritis?
The pathology of viral gastroenteritis is:
-Etiology: The cause of viral gastroenteritis is rotavirus, norovirus, adenovirus, and other viruses.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to viral gastroenteritis The virus uses the enterocyte to replicate, leading to interference with brush border enzyme production, which in turn leads to malabsorption and osmotic diarrhea. Additionally, viral toxins lead to direct damage and cell lysis of enterocytes and intestinal villa, causing a transudative loss of fluid into the intestine. The loss of cell function can lead to electrolyte abnormalities which are caused by the loss of transporter functionality.
-Histology: The histology associated with viral gastroenteritis shows inflammation, swelling, and irritation of the inside lining of your gastrointestinal tract.
How does Viral Gastroenteritis Present?
Patients with viral gastroenteritis typically in all genders at all ages. The symptoms, features, and clinical findings associated with viral gastroenteritis include: watery diarrhea and vomiting, headache, fever, and abdominal cramps.
How is Viral Gastroenteritis Diagnosed?
Disease in sentence case is diagnosed by rapid stool test, and PCR.
How is Viral Gastroenteritis Treated?
Viral gastroenteritis is treated by self-care measures. There’s often no specific medical treatment for viral gastroenteritis. Antibiotics aren’t effective against viruses, and overusing them can contribute to the development of antibiotic-resistant strains of bacteria.
What is the Prognosis of Viral Gastroenteritis?
The prognosis of viral gastroenteritis is excellent. Estimates for mortality and morbidity widely vary.
What is Yersinia?
Yersinia is genus of bacteria in the family Yersiniaceae. Yersinia enterocolitica is an infection caused most often by eating raw or undercooked pork contaminated with Yersinia enterocolitica bacteria.
What is the Pathology of Yersinia Enterocolitica?
The pathology of yersinia enterocolitica is:
-Etiology: The cause of yersinia enterocolitica is bacteria Yersinia.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to yersinia enterocolitica are: colonization of the intestinal tract, particularly the distal small intestine terminal ileum and proximal colon. Accordingly, most of the pathologic effects and, hence, clinical manifestations occur at this location.
-Histology: The histology associated with yersinia enterocolitica shows bacteria.
How does Yersinia Enterocolitica Present?
Patients with yersinia enterocolitica in all genders and at all ages. The symptoms, features, and clinical findings associated with yersinia enterocolitica include: Diarrhea, low-grade fever, abdominal pain, and vomiting.
How is Yersinia Enterocolitica Diagnosed?
Yersinia enterocolitica is diagnosed by detecting the organism in the stool of an infected person.
How is Yersinia Enterocolitica Treated?
Yersinia enterocolitica is treated by aminoglycosides and trimethoprim-sulfamethoxazole.
What is the Prognosis of Yersinia Enterocolitica?
The prognosis of yersinia enterocolitica is good. The symptoms usually last for 1 to 3 weeks. People with mild symptoms usually recover on their own without treatment.
What is Irritable Bowel Syndrome?
Irritable bowel syndrome is a group of symptoms that occur together, including repeated pain in your abdomen and changes in your bowel movements, which may be diarrhea, constipation, or both.
What is the Pathology of Irritable Bowel Syndrome?
The pathology of irritable bowel syndrome is:
-Etiology: The cause of irritable bowel syndrome is a bacteria or a virus
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to irritable bowel syndrome Altered gastrointestinal motility, visceral hypersensitivity, post infectious reactivity, brain-gut interactions, alteration in fecal micro flora, bacterial overgrowth, food sensitivity, carbohydrate malabsorption, and intestinal inflammation all have been implicated in the pathogenesis of IBS
-Histology: The histology associated with irritable bowel syndrome shows increase in mucosal T-lymphocytes.
How does Irritable Bowel Syndrome Present?
Patients with irritable bowel syndrome typically in women present at under age 50 years. The symptoms, features, and clinical findings associated with irritable bowel syndrome include: cramping, abdominal pain, bloating, gas, and diarrhea or constipation, or both.
How is Irritable Bowel Syndrome Diagnosed?
Disease in sentence case is diagnosed by blood tests, stool tests, sigmoidoscopy, and colonoscopy.
How is Irritable Bowel Syndrome Treated?
Irritable bowel syndrome is treated by Alosetron, Eluxadoline, Rifaximin, Lubiprostone, and Linaclotide.
What is the Prognosis of Irritable Bowel Syndrome?
The prognosis of irritable bowel syndrome is not good. IBS tends to last a lifetime and the symptoms often come and go.
What is Inflammatory Bowel Disease?
Inflammatory bowel disease is a term for two conditions Crohn’s disease and ulcerative colitis that are characterized by chronic inflammation of the gastrointestinal GI tract. Prolonged inflammation results in damage to the GI tract.
What is the Pathology of Inflammatory Bowel Disease?
The pathology of inflammatory bowel disease is:
-Etiology: The cause of inflammatory bowel disease is defective immune system.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to inflammatory bowel disease are: the presence of pathogenic factors such as abnormal gut microbiota, immune response dysregulation, environmental changes, and gene variants. an aberrant immune response in which antibodies are formed against colonic epithelial protein.
-Histology: The histology associated with inflammatory bowel disease shows mucosal architecture, lamina propria and submucosal cellularity, neutrophil granulocyte infiltration, and epithelial abnormality.
How does Inflammatory Bowel Disease Present?
Patients with inflammatory bowel disease typically females, present at age older than 20 years. The symptoms, features, and clinical findings associated with inflammatory bowel disease include persistent diarrhea, abdominal pain, rectal bleeding/bloody stools, weight loss, and fatigue.
How Is Inflammatory Bowel Disease Diagnosed?
Inflammatory bowel disease is diagnosed by endoscopy, colonoscopy, contrast radiography, magnetic resonance imaging MRI, or computed tomography CT
How is Inflammatory Bowel Disease Treated?
Inflammatory bowel disease is treated by aminosalicylates, antibiotics, corticosteroids, and immunomodulators.
What is the Prognosis of Inflammatory Bowel Disease?
The prognosis of inflammatory bowel disease is good. Most patients with inflammatory bowel disease are able to lead a normal life and are not disabled by their disease.
What is Colitis-Associated Neoplasia?
Colitis-associated neoplasia is one of the most important causes for morbidity and mortality in patients with inflammatory bowel diseases.
What is the Pathology of Colitis-Associated Neoplasia?
The pathology of disease in lower case is:
-Etiology: The cause of colitis-associated neoplasia is inflammatory bowel disease.
-Genes involved: SMAD, WNT, β-catenin
-Pathogenesis: The sequence of events that lead to colitis-associated neoplasia are: Multiple processes like tumor initiation and metastasis are involved in colitis-associated neoplasia. The pathogenesis of CAC is reported to be affected by multiple pathways, including TGF-β/SMAD, WNT/β-catenin, NOD/TLR, NLRP3 inflammasome, and the cell cycle as well as apoptosis, etc
-Histology: The histology associated with colitis-associated neoplasia shows colonic neoplasia.
How does Colitis-Associated Neoplasia Present?
Patients with colitis-associated neoplasia typically all genders at all ages. The symptoms, features, and clinical findings associated with colitis-associated neoplasia include urgent bowel movements as well as cramps.
How is Colitis-Associated Neoplasia Diagnosed?
Colitis-associated neoplasia is diagnosed by sigmoidoscope, MRI, CT scan.
How is Colitis-Associated Neoplasia Treated?
Colitis-associated neoplasia is treated by drug therapy or surgery.
What is the Prognosis of Colitis-Associated Neoplasia?
The prognosis of colitis-associated neoplasia is fair.
What is Crohn Disease?
Crohn disease is type of inflammatory bowel disease IBD. It causes inflammation of your digestive tract.
What is the Pathology of Crohn Disease?
The pathology of crohn disease is:
-Etiology: The cause of crohn disease is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to crohn disease are: Chronic inflammation from T-cell activation leading to tissue injury is implicated in the pathogenesis of Crohn disease. After activation by antigen presentation, unrestrained responses of type 1 T helper Th1 cells predominate in Crohn disease as a consequence of defective regulation.
-Histology: The histology associated with Crohn disease shows abnormal colonic tissue.
How does Crohn Disease Present?
Patients with Crohn disease typically all genders present at age of 15 to 70 years. The symptoms, features, and clinical findings associated with Crohn disease include diarrhea, fever, fatigue, abdominal pain and cramping, blood in your stool, mouth sores, reduced appetite and weight loss.
How is Crohn Disease Diagnosed?
Crohn disease is diagnosed by colonoscopy, intestinal endoscopies, and biopsy.
How is Crohn Disease Treated?
Crohn disease is treated by Corticosteroids, a more powerful type of anti-inflammatory drug, Anti-inflammatory drugs, Immune system modifiers such as azathioprine Imuran, Azasan and methotrexate Rheumatrex, Trexall.
What is the Prognosis of Crohn Disease?
The prognosis of Crohn disease is good. Most people with Crohn’s disease enjoy healthy, active lives. While there isn’t a cure for Crohn’s disease, treatments and lifestyle changes can keep the disease in remission.
What is Diversion Colitis?
Diversion colitis is a nonspecific inflammatory disorder that occurs in segments of the colon and rectum
What is the Pathology of Diversion Colitis?
The pathology of diversion colitis is:
-Etiology: The cause of diversion colitis is inflammation.
-Genes involved: FFAR2 gene.
-Pathogenesis: The sequence of events that lead to diversion colitis deficiency of short-chain fatty acids due to alterations in gene, which are usually derived from fermentation of dietary starches by normal colonic bacterial flora. Short-chain fatty acids are the main source of energy for colonocytes.
-Histology: The histology associated with diversion colitis shows inflammation of colon.
How does Diversion Colitis Present?
Patients with diversion colitis typically in all genders at any age. The symptoms, features, and clinical findings associated with diversion colitis include mucous discharge, abdominal pain, or low-grade fevers.
How is Diversion Colitis Diagnosed?
Diversion colitis is diagnosed when bloody mucopus is passed from the separate colorectal segment. The colon may be isolated by diverting ileostomy, end or loop colostomy, mucous fistula, or Hartmann procedure.
How is Diversion Colitis Treated?
Diversion colitis is treated by reanastomosis, or the rejoining of the defunctioned bowel to the rest of the intestines.
What is the Prognosis of Diversion Colitis?
The prognosis of diversion colitis is fair. In some severe cases if diversion colitis is left untreated, it may lead to colonic stricture the narrowing of a section of the intestines or the complete loss of function of the defunctioned bowel.
What is Indeterminate Colitis?
Indeterminate colitis is originally referred to those 10-15% of cases of inflammatory bowel disease IBD in which there was difficulty distinguishing between ulcerative colitis UC and Crohn’s disease CD in the colectomy specimen.
What is the Pathology of Indeterminate Colitis?
The pathology of indeterminate colitis is:
-Etiology: The cause of indeterminate colitis is unknown however it might be an autoimmune disease.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to indeterminate colitis are inflammation.
-Histology: The histology associated with indeterminate colitis shows diffuse and uniform chronic active colitis.
How does Indeterminate Colitis Present?
Patients with indeterminate colitis typically women at any age. The symptoms, features, and clinical findings associated with indeterminate colitis include abdominal pain and cramping, diarrhea, weight loss, reduced appetite, fever, and fatigue.
How is Indeterminate Colitis Diagnosed?
Indeterminate colitis is diagnosed by anti-Saccharomyces cerevisiae antibody ASCA and perinuclear antineutrophil cytoplasmic antibody pANCA.
How is Indeterminate Colitis Treated?
Indeterminate colitis has no cure. Sometimes surgery to remove some symptoms of inflammatory bowel disease.
What is the Prognosis of Indeterminate Colitis?
The prognosis of indeterminate colitis is good.
What is Microscopic Colitis?
Microscopic colitis is an inflammation of the large intestine colon that causes persistent watery diarrhea. The disorder gets its name from the fact that it’s necessary to examine colon tissue under a microscope to identify it.
What is the Pathology of Microscopic Colitis?
The pathology of microscopic colitis is:
-Etiology: The cause of microscopic colitis is unknown but it is associated with autoimmune disorders, such as celiac disease.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to microscopic colitis are: The underlying mechanisms involved in the pathogenesis of microscopic colitis remain unspecified but is probably multifactorial. Collagenous colitis and lymphocytic colitis may represent specific mucosal responses to different luminal agents in predisposed individuals, resulting in an uncontrolled immune response.
-Histology: The histology associated with microscopic colitis shows different changes in tissues.
How does Microscopic Colitis Present?
Patients with microscopic colitis typically females present commonly at 50 to 70 years. The symptoms, features, and clinical findings associated with microscopic colitis include chronic watery diarrhea, abdominal pain, cramps or bloating, weight loss, nausea, fecal incontinence, and dehydration.
How is Microscopic Colitis Diagnosed?
Microscopic colitis is diagnosed by colonoscopy with a biopsy .
How is Microscopic Colitis Treated?
Microscopic colitis is treated by antidiarrheal medication such as Pepto-Bismol or Imodium.
What is the Prognosis of Microscopic Colitis?
The prognosis of microscopic colitis is good. Approximately 20% of patients with microcytic colitis may have a spontaneous remission without specific therapy. More than half of patients treated for lymphocytic colitis experienced resolution of symptoms after 6 months of treatment, whereas only 15% of patients had significant persistent symptoms.
What is Ulcerative Colitis?
Ulcerative colitis is an inflammatory bowel disease that causes inflammation and ulcers sores in your digestive tract. Ulcerative colitis affects the innermost lining of your large intestine colon and rectum.
What is the Pathology of Ulcerative Colitis?
The pathology of ulcerative colitis is:
-Etiology: The cause of ulcerative colitis might be autoimmune condition but exact cause is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to ulcerative colitis are: an aberrant immune response in which antibodies are formed against colonic epithelial protein.
-Histology: The histology associated with ulcerative colitis shows expansion of chronic inflammation in the mucosa.
How does Ulcerative Colitis Present?
Patients with ulcerative colitis typically in men t ages 15 to 70 years. The symptoms, features, and clinical findings associated with ulcerative colitis include diarrhea, often with blood or pus, abdominal pain and cramping, rectal pain, rectal bleeding, passing small amount of blood with stool, urgency to defecate, inability to defecate despite urgency, weight loss, and fatigue.
How is Ulcerative Colitis Diagnosed?
Ulcerative colitis is diagnosed by endoscopic procedures with tissue biopsy.
How is Ulcerative Colitis Treated?
Ulcerative colitis is treated by infliximab, remicade, adalimumab, golimumab, vedolizumab, and ustekinumab stelara.
What is the Prognosis of Ulcerative Colitis?
The prognosis of ulcerative colitis is good. It is a lifelong illness with no specific cause or cure. The life expectancy of patients with ulcerative colitis UC is usually the same as anybody without the disease.
What is Sigmoid Diverticular Disease?
Sigmoid diverticular disease is called so because diverticula can form while straining during a bowel movement, such as with constipation. They are most common in the lower portion of the large intestine called the sigmoid colon.
What is the Pathology of Sigmoid Diverticular Disease?
The pathology of sigmoid diverticular disease is:
-Etiology: The cause of sigmoid diverticular disease is when naturally weak places in your colon give way under pressure.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to sigmoid diverticular disease are: the obstruction of the diverticulum sac by fecalith, which by irritation of the mucosa causes low-grade inflammation, congestion and further obstruction.
-Histology: The histology associated with sigmoid diverticular disease shows structural abnormalities of colonic wall.
How does Sigmoid Diverticular Disease Present?
Patients with sigmoid diverticular disease typically in females present after 40 years of age. The symptoms, features, and clinical findings associated with sigmoid diverticular disease include: pain at lower left part of the abdomen.
How is Sigmoid Diverticular Disease Diagnosed?
Sigmoid diverticular disease is diagnosed by stool test, to rule out infection in people who have diarrhea. A CT scan, which can identify inflamed or infected pouches and confirm a diagnosis of diverticulitis. CT can also indicate the severity of diverticulitis and guide treatment.
How is Sigmoid Diverticular Disease Treated?
Sigmoid diverticular disease is treated by antibiotics to resolve bacterial infections, surgery, gentle bowel stimulation and cleansing with small aliquots of magnesium citrate, might help reduce the stool load
What is the Prognosis of Sigmoid diverticular disease?
The prognosis of sigmoid diverticular disease is good.
What are Colonic Polyps?
Colonic polyps are a small clump of cells that forms on the lining of the colon. Most colon polyps are harmless. But over time, some colon polyps can develop into colon cancer, which may be fatal when found in its later stages.
Examples of colonic polyps are:
- Hamartomatous polyps: juvenile polyps. Peutz-Jeghers syndrome
- Hyperplastic polyps
- Inflammatory polyps
- Neoplastic polyps
- Adenomatous polyps
What are Hamartomatous Polyps?
Hamartomatous polyps are the gastrointestinal GI tract are rare compared to other types of GI polyps, yet they are the most common type of polyp in children. The symptoms are usually rectal bleeding, abdominal pain, obstipation, anaemia, and/or small bowel obstruction.
Examples of hamartomatous polyps include:
- Juvenile polyps
- Peutz-Jeghers syndrome
What are Juvenile Polyps?
Juvenile polyps are a hereditary condition that is characterized by the presence of hamartomatous polyps in the digestive tract. The term “juvenile polyposis” refers to the examination of the polyp under a microscope.
What is the Pathology of Juvenile Polyps?
The pathology of juvenile polyps is:
-Etiology: The cause of juvenile polyps is mutation.
-Genes involved: BMPR1A, SMAD4.
-Pathogenesis: The sequence of events that lead to juvenile polyps is unknown.
-Histology: The histology associated with juvenile polyps shows spherical appearance with extensive surface erosion; a marked increase of the stromal cell compartment; inflammatory and reactive changes of the epithelium and distorted and dilated crypts.
How does Juvenile Polyps Present?
Patients with juvenile polyps typically are all genders between 2 to 5 years of age.The symptoms, features, and clinical findings associated with juvenile polyps include bleeding from the rectum, diarrhea, constipation, cramping/abdominal pain, chronic long-term weight loss.
How is Juvenile Polyps Diagnosed?
Juvenile polyps is diagnosed by colonoscopy and biopsy.
How is Juvenile Polyps Treated?
Juvenile polyps is treated by endoscopy and surgical removal.
What is the Prognosis of Juvenile Polyps?
The prognosis of juvenile polyps is good. It usually affects the colon, but can occur in the small intestine, stomach, or pancreas. People with JPS have a 10 percent to 50 percent risk of developing cancer in the GI tract.
What is Peutz-Jeghers Syndrome?
Peutz-Jeghers syndrome is an inherited condition that puts people at an increased risk for developing hamartomatous polyps in the digestive tract, as well as cancers of the breast, colon, rectum, pancreas, stomach, testicles, ovaries, lung, and cervix.
What is the Pathology of Peutz-Jeghers Syndrome?
The pathology of peutz-jeghers syndrome is:
-Etiology: The cause of peutz-jeghers syndrome is a mutation in the STK11 gene, also known as the LKB1 gene.
-Genes involved: STK11.
-Pathogenesis: The sequence of events that lead to peutz-jeghers syndrome an autosomal dominant syndrome with incomplete and variable penetrance. About 50% of PJS patients have loss-of-function heterozygous mutations in a tumor suppressor gene STK11.
-Histology: The histology associated with peutz-jeghers syndrome shows a distinctive arborization of smooth muscle within the lamina propria.
How does Peutz-Jeghers Syndrome Present?
Patients with peutz-jeghers syndrome typically are all genders and symptoms appear at 10 years of age. The symptoms, features, and clinical findings associated with peutz-jeghers syndrome include: characteristic dark-colored spots, development of hamartomatous polyps non-cancerous overgrowths of tissue, small bowel obstruction, and gastrointestinal bleeding.
How is Peutz-Jeghers Syndrome Diagnosed?
Peutz-jeghers syndrome is diagnosed by gastroenterology GI endoscopy and a colonoscopy.
How is Peutz-Jeghers Syndrome Treated?
Peutz-jeghers syndrome is treated by endoscopy and removal.
What is the Prognosis of Peutz-Jeghers Syndrome?
The prognosis of Peutz-Jeghers syndrome is fair. It is a life-long condition that can be passed on to children. People with PJS need to be checked frequently for developing polyps. Those polyps can develop into cancer or cause a blockage that could require surgery.
What are Hyperplastic Polyps?
Hyperplastic polyps is a growth of extra cells that projects out from tissues inside your body. They occur in areas where your body has repaired damaged tissue, especially along your digestive tract. Hyperplastic colorectal polyps happen in your colon, the lining of your large intestine.
What is the Pathology of Hyperplastic Polyps?
The pathology of hyperplastic polyps is:
-Etiology: The cause of hyperplastic polyps is chronic stomach inflammation, and mutations.
-Genes involved: MLH-1, MGMT.
-Pathogenesis: The sequence of events that lead to hyperplastic polypsis unclear. It had no malignant potential. However, it is recommended to biopsy the lesion and surrounding mucosa shows mixture of normal, ulcerated, and regenerating mucosa which is surrounded by areas of mucosal loss.
-Histology: The histology associated with hyperplastic polyps shows serrated architecture with a sawtooth appearance, with serrations generally limited to the upper half of the crypts mild nuclear enlargement, stratification and hyperchromasia, limited to the crypt bases.
How does Hyperplastic Polyps Present?
Patients with hyperplastic polyps typically all genders over the age of 50 years. The symptoms, features, and clinical findings associated with hyperplastic polyps include: pain or tenderness, nausea, blood in your stool, anemia.
How is Hyperplastic Polyps Diagnosed?
Hyperplastic polyps is diagnosed endoscopy and biopsy.
How is Hyperplastic Polyps Treated?
Hyperplastic polyps is treated by endoscopy and removal.
What is the Prognosis of Hyperplastic Polyps?
The prognosis of hyperplastic polyps is fair. Polyps must be removed before they become cancerous lowers your risk of developing colorectal or stomach cancer by almost 80 percent. Most are harmless and won’t ever become cancerous.
What are Inflammatory Polyps?
Inflammatory polyps are non-neoplastic intraluminal projections of mucosa consisting of stromal and epithelial components and inflammatory cells.
What is the Pathology of Inflammatory Polyps?
The pathology of inflammatory polyps is:
-etiology: the cause of inflammatory polyps is inflammatory intestinal conditions, smoking and excess alcohol use, obesity, lack of exercise and fat intake.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to inflammatory polyps are polypoid mucosal tags after regeneration and the adjacent mucosa showed regenerative changes and submucosal scarring.
-Histology: The histology associated with inflammatory polyps shows predomination of the inflammatory component represented by granulation tissue and does not contain glands but may contain foreign bodies and giant cells.
How does Inflammatory Polyps Present?
Patients with inflammatory polyps typically are all genders with age 50 years of age or older. The symptoms, features, and clinical findings associated with inflammatory polyps include change in bowel habits, pain, iron deficiency anemia.
How is Inflammatory Polyps Diagnosed?
Inflammatory polyps is diagnosed by colonoscopy, CT scan, and biopsy.
How is Inflammatory Polyps Treated?
Inflammatory polyps is treated by surgery and medication.
What is the Prognosis of Inflammatory Polyps?
The prognosis of inflammatory polyps is good. These types of polyps are also known as pseudopolyps because they are not true polyps, but rather develop as a reaction to chronic inflammation in the colon.
What are Neoplastic Polyps?
Neoplastic polyps include adenomas and serrated types. These polyps have the potential to become cancer if given enough time to grow. Most of these colon polyps are called adenomas. Serrated polyps may also become cancerous, depending on their size and location in the colon.
What is the Pathology of Neoplastic Polyps?
The pathology of neoplastic polyps is:
-Etiology: The cause of neoplastic polyps is smoking and excess alcohol use, obesity, lack of exercise and fat intake, race.
-Genes involved: None.
-Pathogenesis: the sequence of events that lead to neoplastic polyps are hyperplastic epithelial foci and small hyperplastic polyps with juvenile polyps with focal adenomatous epithelium.
-Histology: The histology associated with neoplastic polyps shows tubular, tubulovillous, or villous based on the glandular architecture.
How does Neoplastic Polyps Present?
Patients with neoplastic polyps typically more in men at age of 50 or older. The symptoms, features, and clinical findings associated with neoplastic polyps include: mixture of normal, ulcerated, and regenerating mucosa which is surrounded by areas of mucosal loss.
How is Neoplastic Polyps Diagnosed?
Neoplastic polyps is diagnosed by virtual colonoscopy, CT colonography, stool-based tests, flexible sigmoidoscopy, and biopsy.
How is Neoplastic Polyps Treated?
Neoplastic polyps is treated by removal with forceps or a wire loop polypectomy, surgery.
What is the Prognosis of Neoplastic Polyps?
The prognosis of neoplastic polyps is poor.
What are Adenomatous Polyps?
Adenomatous polyps are often known as adenomas, a type of polyps that can turn into cancer. Adenomas may form in the mucous membrane of the lining in the large intestine, making them colon polyps.
What is the Pathology of Adenomatous Polyps?
The pathology of adenomatous polyps is:
-Etiology: The cause of adenomatous polyps is: genetics, age, ethnicity, and smoking.
-Genes involved: APC
-Pathogenesis: The sequence of events that lead to adenomatous polyps are not completely known.
-Histology: The histology associated with adenomatous polyps shows their histological appearance as tubular, villous, or tubule-villous adenomas. A tubular adenoma has the histological appearance of branched tubular glands.
How does Adenomatous Polyps Present?
Patients with adenomatous polyps typically are both male and female at mid-teens age. The symptoms, features, and clinical findings associated with adenomatous polyps include: abdominal pain, anemia, constipation or diarrhea, a change in stool color.
How is Adenomatous Polyps Diagnosed?
Adenomatous polyps is diagnosed by colonoscopy, sigmoidoscopy, and biopsy.
How is Adenomatous Polyps Treated?
Adenomatous polyps is treated by surgery.
What is the Prognosis of Adenomatous Polyps?
The prognosis of adenomatous polyps is fair. These are usually harmless however, in some cases, they may be precancerous. If a doctor does not remove them, they may grow and develop into cancer.
What is Adenomatous Polyposis?
Adenomatous polyposis is an area where normal cells that line the inside of a person’s colon form a mass on the inside of the intestinal tract.
What is the Pathology of Adenomatous Polyposis?
The pathology of adenomatous polyposis is:
-Etiology: The cause of adenomatous polyposis is a defected gene.
-Genes involved: POLE, POLD1.
-Pathogenesis: The sequence of events that lead to adenomatous polyposis are not completely known.
-Histology: The histology associated with adenomatous polyposis shows numerous adenomatous polyps form mainly in the epithelium of the large intestine. While these polyps start out benign, malignant transformation into colon cancer occurs when they are left untreated.
How does Adenomatous Polyposis Present?
Patients with adenomatous polyposis typically are both sexes at age range of 35years. The symptoms, features, and clinical findings associated with adenomatous polyposis include: unexplained diarrhea, a long period of constipation, abdominal cramps, decrease in size or caliber of stool, gas pain, bloating, fullness, unexplained weight loss, lethargy and vomiting.
How is Adenomatous Polyposis Diagnosed?
Adenomatous polyposis is diagnosed by biopsy, genetic testing, and colonoscopy.
How is Adenomatous Polyposis Treated?
Adenomatous polyposis is treated by surgical removal.
What is the Prognosis of Adenomatous Polyposis?
The prognosis of adenomatous polyposis is poor. Patients untreated have a median life expectancy of 42 years old. Life expectancy is extended greatly in those treated with colectomy. Upper gastrointestinal cancers and desmoid tumors are the most common causes of death in patients who have undergone colectomy.
What is Hereditary Non-Polyposis Colorectal Cancer?
Hereditary non-polyposis colorectal cancer is a condition in which the tendency to develop colorectal cancer is inherited. “Nonpolyposis” means that colorectal cancer can occur when only a small number of polyps are present. In families with HNPCC, cancer usually occurs on the right side of the colon.
What is the Pathology of Hereditary Non-Polyposis Colorectal Cancer?
The pathology of hereditary non-polyposis colorectal cancer is:
-Etiology: The cause of hereditary non-polyposis colorectal cancer is an inherited mutation or abnormality.
-Genes involved: hMSH2.
-Pathogenesis: The sequence of events that lead to hereditary non-polyposis colorectal cancer are inherited mutations of DNA mismatch repair MMR genes responsible for the correction of DNA mismatches, such as base substitution mismatch and insertion-deletion mismatch.
-Histology: The histology associated with hereditary non-polyposis colorectal cancer shows that these cancers are more often mucinous, poorly differentiated, signet ring cells with lymphocytic infiltrate, or rimmed by a germinal center producing a lymphoid reaction.
How does Hereditary Non-Polyposis Colorectal Cancer Present?
Patients with hereditary non-polyposis colorectal cancer typically are all genders at age range before 40 years. The symptoms, features, and clinical findings associated with hereditary non-polyposis colorectal cancer include: rectal bleeding, stomach pain , weight loss and fatigue.
How is Hereditary Non-Polyposis Colorectal Cancer Diagnosed?
Hereditary non-polyposis colorectal cancer is diagnosed by sigmoidoscopy, colonoscopy, and biopsy.
How is Hereditary Non-Polyposis Colorectal Cancer Treated?
Hereditary non-polyposis colorectal cancer is treated by surgery.
What is the Prognosis of Hereditary Non-Polyposis Colorectal Cancer?
The prognosis of hereditary non-polyposis colorectal cancer is good. The 5-year survival rate in patients with hereditary nonpolyposis colorectal cancer HNPCC is estimated to be approximately 60%, compared with 40-50% for sporadic cases.
What are Tumors of the Anal Canal?
Tumors of the anal canal are squamous cell carcinoma, adenocarcinoma, cloacogenic or basaloid carcinoma, melanoma, leiomyosarcoma, and carcinoid tumors.
Examples of tumors of the anal canal:
- Anal transition zone carcinoma
- Basaloid anal transition zone tumor
- Condyloma acuminatum
What is Anal transition zone carcinoma?
Anal transition zone carcinoma is he mucosa of the anal transition zone having both squamous and transitional features. Carcinomas arising in this zone. have, in the past, been referred to as “cloacogenic”, a term of doubtful validity.
What is the Pathology of Anal transition zone Carcinoma?
The pathology of anal transition zone carcinoma is:
-Etiology: The cause of anal transition zone carcinoma is human papilloma virus HPV infection.
-Genes involved: 5q21.
-Pathogenesis: The sequence of events that lead to anal transition zone carcinoma are tumors arise from anal transition zone and are grouped together.
-Histology: The histology associated with anal transition zone carcinoma vary from well-differentiated squamous cell carcinomas with evident keratinization to basaloid carcinomas composed of small undifferentiated cells with peripheral palisading.
How does Anal transition zone Carcinoma Present?
Patients with anal transition zone carcinoma typically more females and younger than 30 years of age. The symptoms, features, and clinical findings associated with anal transition zone carcinoma include: pain or a feeling of fullness around the anus, lumps that may resemble hemorrhoids, changes in bowel movements, a discharge from the anus, swollen lymph nodes in the groin or anal area.
How is Anal transition zone Carcinoma Diagnosed?
Anal transition zone carcinoma is diagnosed by anoscopy, flexible sigmoidoscopy, and biopsy.
How is Anal transition zone Carcinoma Treated?
Anal transition zone carcinoma is treated by chemotherapy and radiation.
What is the Prognosis of Anal transition zone Carcinoma?
The prognosis of anal transition zone carcinoma is poor.
What is Basaloid Anal Transition Zone Tumor?
Basaloid anal transition zone tumor is the pattern mixed with squamous-basaloid. Basaloid tumors must be differentiated from a basal cell carcinoma extending from perianal skin.
What is the Pathology of Basaloid Anal Transition Zone Tumor?
The pathology of basaloid anal transition zone tumor is:
-Etiology: The cause of basaloid anal transition zone tumor is STD, increased spinchter tone, other diseases.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to basaloid anal transition zone tumor arises from the entodermal-ectodermal junctional zone of the anal canal at or above the dentate line particular the presence of palisading of the nuclei at the periphery of the clumps of tumour cells, but are potentially metastasizing tumours.
-Histology: The histology associated with basaloid anal transition zone tumor shows palisading solid circumscribed clumps of tumour cells containing small, round, or ovoid nuclei which are regular in shape and size.
How does Basaloid Anal Transition Zone Tumor Present?
Patients with basaloid anal transition zone tumor typically more in females at age of 41 to 80 years. The symptoms, features, and clinical findings associated with basaloid anal transition zone tumor include the feeling of a lump or mass at the anal opening, persistent or recurring pain in the anal area, persistent or recurrent itching.
How is Basaloid Anal Transition Zone Tumor Diagnosed?
Basaloid anal transition zone tumor is diagnosed by anoscopy, flexible sigmoidoscopy, and biopsy.
How is Basaloid Anal Transition Zone Tumor Treated?
Basaloid anal transition zone tumor is treated by radiotherapy.
What is the Prognosis of Basaloid Anal Transition Zone Tumor?
The prognosis of basaloid anal transition zone tumor is poor.
What is Condyloma Acuminatum?
Condyloma acuminatum is known as anogenital warts, manifestations of HPV infection that occur in a subset of individuals with anogenital HPV infection.
What is the Pathology of Condyloma Acuminatum?
The pathology of condyloma acuminatum is:
-Etiology: The cause of condyloma acuminatum is human papillomavirus HPV.
-Genes involved: TLR2 597.
-Pathogenesis: The sequence of events that lead to condyloma acuminatum are cells of the basal layer of the epidermis are invaded by human papillomavirus HPV. These penetrate through skin and cause mucosal microabrasions.
-Histology: The histology associated with condyloma acuminatum generally demonstrates disruption of the epidermis with hyperkeratosis, coarse keratohyaline granules, and koilocytes in a prominent granular layer. The epidermis or mucosa of flat condylomata demonstrates acanthosis.
How does Condyloma Acuminatum Present?
Patients with condyloma acuminatum typically are all genders at age range of 18–59 years. The symptoms, features, and clinical findings associated with condyloma acuminatum include: small, skin-colored or gray spots in your genital area that are raised or flat, several warts close together that are shaped like a cauliflower, itching or discomfort in your genital area.
How is Condyloma Acuminatum Diagnosed?
Condyloma acuminatum is diagnosed clinically.
How is Condyloma Acuminatum Treated?
Condyloma acuminatum is treated by: cryotherapy, trichloroacetic acid, surgical excision, electrosurgery, and laser therapy.
What is the Prognosis of Condyloma Acuminatum?
The prognosis of condyloma acuminatum is good. It is cleared up without any intervention within a few months after acquisition, and about 90% clear within 2 years. The treatment can be delayed in children, adolescents, and young, healthy adults, as lesions often resolve spontaneously over months to years.
What are Hemorrhoids?
Hemorrhoids are are swollen veins in your lower rectum also called piles, are swollen veins in your anus and lower rectum, similar to varicose veins. There are two types of hemorrhoids, internal or external hemorrhoids. Internal hemorrhoids lie inside the rectum. You usually can’t see or feel them and they rarely cause discomfort.
What is the Pathology of Internal Hemorrhoids?
The pathology of internal hemorrhoids is:
-Etiology: The cause of internal hemorrhoids is straining during bowel movements, sitting for long periods of time on the toilet, having chronic diarrhea or constipation.
-Genes involved: MMP9.
-Pathogenesis: The sequence of events that lead to internal hemorrhoids is not fully understood. Many functional, histopathological and anatomical findings have been accumulated during the last decades, but the relation between them remains obscure.
-Histology: The histology associated with internal hemorrhoids shows as piles, are swollen veins in the lower part of the anus and rectum. When the walls of these vessels are stretched, they become irritated.
How does Internal Hemorrhoids Present?
Patients with internal hemorrhoids typically are all genders in adults aged 45 to 65 years old. The symptoms, features, and clinical findings associated with internal hemorrhoids include: hard lumps near the anus that feel sore or tender, pain or ache in the anus, especially when you sit, rectal bleeding.
How is Internal Hemorrhoids Diagnosed?
Internal hemorrhoids is diagnosed by digital examination, and visual inspection.
How is Internal Hemorrhoids Treated?
Internal hemorrhoids is treated by surgical removal, or symptomatic management.
What is the Prognosis of Internal Hemorrhoids?
The prognosis of internal hemorrhoids is fair. This is not dangerous, but can result in pain and swelling. Internal hemorrhoids may bleed, but they usually aren’t painful.
What is the Pathology of External Hemorrhoids?
The pathology of external hemorrhoids is:
-Etiology: The cause of external hemorrhoids is straining while pooping, repeated straining while having a bowel movement, sitting on the toilet for a long time, weakened support tissues, Pregnancy.
-Genes involved: MMP9.
-Pathogenesis: The sequence of events that lead to external hemorrhoids shows that the veins become distended as they lose their support. The descended loose lining becomes more sensitive to pressure from straining and to trauma from the stool.
-Histology: The histology associated with external hemorrhoids shows tufts of engorged, dilated veins and arteries with thrombi and hemorrhage, in a dense stroma, covered by anal or rectal mucosa, which often is ulcerated.
How does External Hemorrhoids Present?
Patients with external hemorrhoids typically are all genders at age range of 50years.The symptoms, features, and clinical findings associated with external hemorrhoids include: pain or discomfort, swelling around your anus, bleeding.
How is External Hemorrhoids Diagnosed?
External hemorrhoids is diagnosed by anoscopy, and digital rectal exam.
How is External Hemorrhoids Treated?
External hemorrhoids is treated by symptomatic management and surgery if needed.
What is the Prognosis of External Hemorrhoids?
The prognosis of external hemorrhoids is good. They often go away on their own within a few days or weeks as the body reabsorbs the blood clot within the protruding blood vessel.
What is Acute Appendicitis?
Acute appendicitis is the sudden and severe inflammation of the appendix. It can cause pain in the abdomen, and this pain may occur quickly and worsen within hours. The appendix is a narrow tube that attaches to the large intestine.
What is the Pathology of Acute Appendicitis?
The pathology of acute appendicitis is:
-Etiology: The cause of acute appendicitis are various infections such as virus, bacteria, or parasites.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to acute appendicitis are obstruction of the appendiceal lumen, typically by lymphoid hyperplasia but occasionally by a fecalith, foreign body, or even worms. The obstruction leads to distention, bacterial overgrowth, ischemia, and inflammation. If untreated, necrosis, gangrene, and perforation occur.
-Histology: The histology associated with acute appendicitis shows the swollen organ and serosa shows hypereamia and engorged vessels on the surface.
How does Acute Appendicitis Present?
Patients with acute appendicitis are typically all genders and present at age between the ages 10 and 30 years old. The symptoms, features, and clinical findings associated with acute appendicitis include sudden pain that begins on the right side of the lower abdomen, sudden pain that begins around your navel and often shifts to your lower right abdomen, pain that worsens if you cough, walk or make other jarring movements, nausea and vomiting, loss of appetite.
How is Acute Appendicitis Diagnosed?
Acute appendicitis is diagnosed by physical exam, abdominal ultrasound, and complete blood count.
How is Acute Appendicitis Treated?
Acute appendicitis is treated appendectomy.
What is the Prognosis of Acute Appendicitis?
The prognosis of acute appendicitis is good. With an early operation, the chance of death from appendicitis is very low. The person can usually leave the hospital in 1 to 3 days, and recovery is normally quick and complete. However, older people often take longer to recover.
What are Tumors of the Appendix?
Tumors of the appendix are a part of the lymphatic, exocrine, or endocrine systems. Appendix cancer occurs when healthy cells in the appendix change and grow out of control. These cells form a growth of tissue, called a tumor.
Examples of tumors of the appendix include:
- Neuroendocrine tumors
- Adenomas
- Adenocarcinomas
- Mucocele
- Mucinous cystadenoma
What is Peritoneal Cavity Pathology?
Peritoneal cavity pathology is the space within the abdomen that contains the intestines, the stomach, and the liver. It is bound by thin membranes.
What is Peritoneal Cavity Inflammatory Disease?
Peritoneal cavity inflammatory disease is the tissue disease that lines the inner wall of the abdomen and covers and supports most of your abdominal organs. Peritonitis is usually caused by infection from bacteria or fungi.
What is Peritoneal Cavity Infections?
Peritoneal cavity Infections is a silk-like membrane that lines your inner abdominal wall and covers the organs within your abdomen that is usually due to a bacterial or fungal infection.
What is Sclerosing Retroperitonitis?
Sclerosing retroperitonitis are fibrotic lesions of soft tissue that simulate clinically certain types of malignant neoplasms. The medical history of a patient having either of these diseases is that of a patient having a malignant disorder.
What is the Pathology of Sclerosing Retroperitonitis?
The pathology of sclerosing retroperitonitis is:
-Etiology: The cause of sclerosing retroperitonitis are kidney infections, abscesses, and stones.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to sclerosing retroperitonitis were not exactly known.
-Histology: The histology associated with sclerosing retroperitonitis shows obliterative phlebitis, fat necrosis.
How does Sclerosing Retroperitonitis Present?
Patients with sclerosing retroperitonitis typically are all genders of all ages.The symptoms, features, and clinical findings associated with sclerosing retroperitonitis include abdominal pain, pain in nearby areas such as the back or scrotum, circulation problems in the legs, which can cause pain and skin discolouration.
How is Sclerosing Retroperitonitis Diagnosed?
Sclerosing retroperitonitis is diagnosed by CT or MRI scans.
How is Sclerosing Retroperitonitis Treated?
Sclerosing retroperitonitis is treated by anti-inflammatory medications, or surgery.
What is the Prognosis of Sclerosing Retroperitonitis?
The prognosis of sclerosing retroperitonitis is poor. Most patients have an average survival of approximately 3-6 months.
What is Tumors of the Peritoneal Cavity?
Tumors of the peritoneal cavity are ovarian cancer, primary colorectal cancer, appendiceal cancer, or mesothelioma and pseudomyxoma peritonei known as peritoneal carcinomatosis.
Tumors of the peritoneal cavity include:
- Mesotheliomas
- Mucinous carcinomas
What are Mesotheliomas?
Mesotheliomas are a type of cancer that occurs in the thin layer of tissue that covers the majority of your internal organs mesothelium. Mesothelioma is an aggressive and deadly form of cancer.
What is the Pathology of Mesotheliomas?
The pathology of mesotheliomas is:
-Etiology: The cause of mesotheliomas is Asbestos exposure.
-Genes involved: BAP1.
-Pathogenesis: The sequence of events that lead to mesotheliomas shows an aggressive tumor arising primarily from the pleural or peritoneal cavities. It develops by asbestos exposure after a long latency, which is characterized by insidious growth and clinical presentation at an advanced stage of disease.
-Histology: The histology associated with mesotheliomas shows epithelioid type, sarcomatoid type, biphasic type, desmoplastic type, among others.
How does Mesotheliomas Present?
Patients with mesotheliomas typically are all genders and mostly have disease at 69 years age. The symptoms, features, and clinical findings associated with mesotheliomas include: pain in the side of the chest or lower back, shortness of breath, cough, trouble swallowing feeling like food gets stuck, hoarseness, swelling of the face and arms.
How is Mesotheliomas Diagnosed?
Mesotheliomas is diagnosed by chest X-ray and a computerized tomography CT scan.
How is Mesotheliomas Treated?
Mesotheliomas is treated by surgery, chemotherapy, and immunotherapy.
What is the Prognosis of Mesotheliomas?
The prognosis of mesotheliomas is poor. The mesothelioma survival rates are typically 4–18 months after diagnosis, but there have been patients diagnosed with mesothelioma who have lived longer than 10 years. The current five-year survival rate for the disease is just 10 percent.
What are Mucinous Carcinomas?
Mucinous carcinomas are a rare form of invasive ductal carcinoma cancer that begins in the milk duct and spreads beyond it into nearby healthy tissue.
What is the Pathology of Mucinous Carcinomas?
The pathology of mucinous carcinomas is:
-Etiology: The cause of mucinous carcinomas is age, gender, obesity, tobacco, sedentary lifestyle, alcohol, breast density specifically for breast cancer, and unhealthy diet.
-Genes involved: TP53.
-Pathogenesis: The sequence of events that lead to mucinous carcinomas harbor a low level of genetic instability and rare recurrent amplifications, and the genomic profiles of the tumor components of mixed mucinous tumors are remarkably similar to those of pure mucinous carcinomas. More than 90% of pure mucinous carcinomas are diploid, whereas only 42% of mixed mucinous carcinoma are diploid.
-Histology: The histology associated with mucinous carcinomas shows there is a dermal mass composed of glands and solid nests of epithelial cells which appear to be floating in copious mucin. The cells are enlarged, show mild pleomorphism and often have an eosinophilic cytoplasm.
How does Mucinous Carcinomas Present?
Patients with mucinous carcinomas typically more in females mostly at age between 35 to 70 years. The symptoms, features, and clinical findings associated with mucinous carcinomas include: irritation or dimpled area of the skin, scales or redness of the skin of the breast, underarm lump swelling of the breast, pain in the breast.
How is Mucinous Carcinomas Diagnosed?
Mucinous carcinomas is diagnosed by ultrasound, MRI, or biopsy.
How is Mucinous Carcinomas Treated?
Mucinous carcinomas is treated by surgery, radiation therapy, hormonal therapy, and chemotherapy.
What is the Prognosis of Mucinous Carcinomas?
The prognosis of mucinous carcinomas is good.