Granulomatosis with polyangiitis is also known as inflammation of the blood vessels and the most affected blood vessels are those in the ears, lungs, kidneys, nose, and throat. Granulomatosis with polyangiitis is also known as Wegener’s granulomatosis with necrotizing vasculitis.
What is the Pathology of Granulomatosis with Polyangiitis?
The pathology of granulomatosis with polyangiitis is:
-Etiology: The cause of granulomatosis with polyangiitis is unknown but there is the involvement of anti-neutrophilic cytoplasmic antibodies.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to granulomatosis with polyangiitis is not fully understood.
-Morphology: NA.
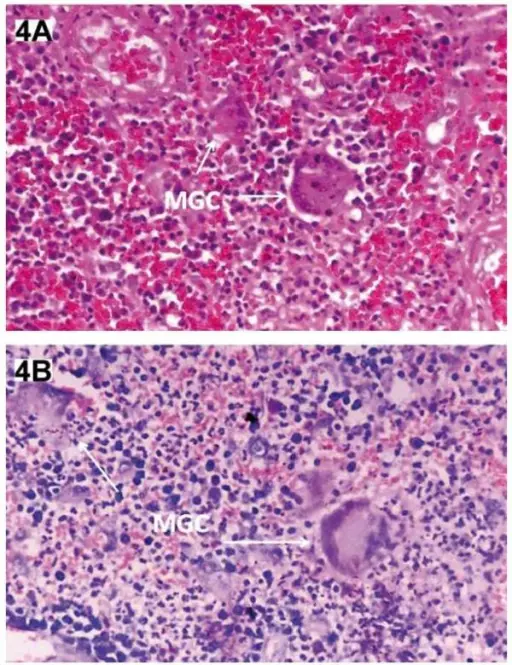
-Histology: The histology associated with granulomatosis with polyangiitis shows multinucleated giant cells, segmental necrotizing lesions, with crescent formation.
How does Granulomatosis with Polyangiitis Present?
Patients with granulomatosis with polyangiitis typically are both males and present at the age range of 40-60 years old. The symptoms, features, and clinical findings associated with granulomatosis with polyangiitis include fever, weight loss, asthenia, sinusitis, chronic otitis media alveolar hemorrhage, and saddle nose deformity.
How is Granulomatosis with Polyangiitis Diagnosed?
Granulomatosis with polyangiitis is diagnosed by biopsy, chest radiography, urinalysis, physical examination, and ANCA assay.
How is Granulomatosis with Polyangiitis Treated?
Granulomatosis with polyangiitis is treated by immunosuppressors, plasma exchange, corticosteroids, and cytotoxic agents.
What is the Prognosis of Granulomatosis with Polyangiitis?
The prognosis of granulomatosis with polyangiitis is poor.