Infectious esophagitis is a bacterial, viral or fungal infection in tissues of the esophagus.
What is the Pathology of Infectious Esophagitis?
The pathology of infectious esophagitis is:
-Etiology: The cause of infectious esophagitis is fungal, viral, bacterial or even parasitic agents. Risk factors include antibiotics and steroids use, chemotherapy and/or radiation therapy, malignancies and immunodeficiency syndromes including acquired immunodeficiency syndrome.
-Genes involved: TSLP, LRRC32.
-Pathogenesis: The sequence of events that lead to infectious esophagitis colonization with mucosal adherence and proliferation.
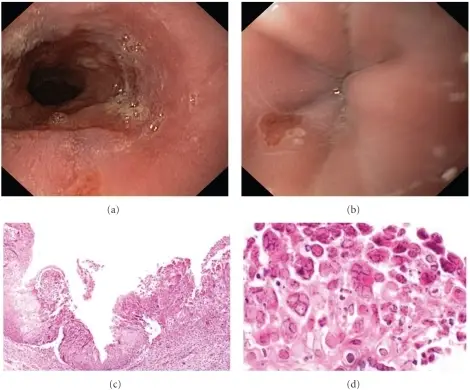
-Histology: The histology associated with infectious esophagitis shows nuclear molding, margination, and multinucleation of infected cells. Eosinophilic intranuclear and cytoplasmic inclusion bodies within squamous cells, referred to as Cowdry type A inclusions, may be seen.
How does Infectious Esophagitis Present?
Patients with infectious esophagitis typically more in males and present at age range of 11 to 84 years. The symptoms, features, and clinical findings associated with infectious esophagitis include: pain when swallowing, difficulty swallowing, mouth pain, chest pain, nausea or vomiting.
How is Infectious Esophagitis Diagnosed?
Infectious esophagitis is diagnosed by endoscopy and esophageal biopsy.
How is Infectious Esophagitis Treated?
Infectious esophagitis is treated with antiviral medicines, such as acyclovir. Bacterial esophagitis may be treated with broad-spectrum antibiotics. These are medicines that work against many types of bacteria. Sometimes acid blockers are used along with other treatments.
What is the Prognosis of Infectious Esophagitis?
The prognosis of infectious esophagitis is poor. Severe esophagitis may lead to dysphagia, pain, odynophagia, and malnutrition. Rarely, life-threatening bleeding occurs and may lead to death. Outcomes and survival in these patients are related to the severity of their underlying systemic illness.