Joint pathology is any disease, disorder, or injury that affects human joints.
What is Osteoarthritis?
Osteoarthritis is a degenerative joint disease that damages articular cartilage of synovial joints.
What is the Pathology of Osteoarthritis?
The pathology of osteoarthritis is:
-Etiology: The cause of osteoarthritis is the damage or breakdown of joint cartilage between bones.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to osteoarthritis involves degeneration of cartilage and bone of synovial joints.
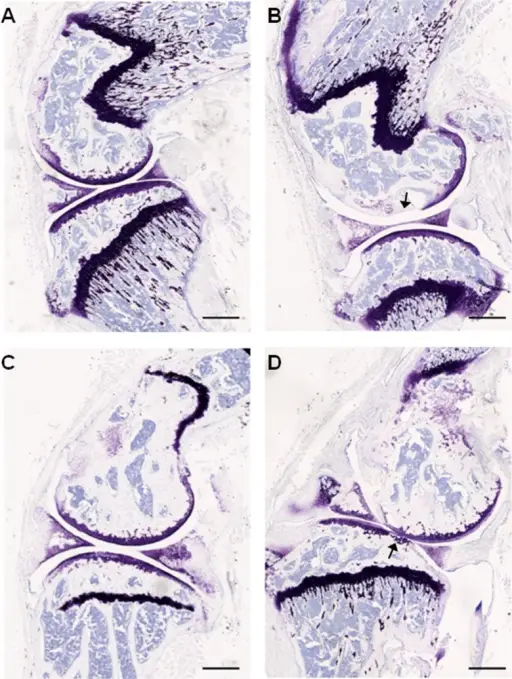
-Histology: The histology associated with osteoarthritis shows osteophytes and erosion of the articular surface.
How does Osteoarthritis Present?
Patients with osteoarthritis typically present with synovial joint pain and stiffness. The associated pain and stiffness in joints worsens with activity and is relieved by rest. The pain tends to worsen throughout the day, but the stiffness tends to improve throughout the day. Prolonged osteoarthritis can result in deformity and reduced range of motion.
How is Osteoarthritis Diagnosed?
Osteoarthritis is diagnosed by doing routine blood tests that can be useful to exclude inflammatory or infectious causes. Radiographic imaging may be useful for confirming the diagnosis and ruling out fractures.
How is Osteoarthritis Treated?
Osteoarthritis is treated using analgesics and topical NSAIDs. Intra-articular steroid injections may be considered for certain patients.
What is the Prognosis of Osteoarthritis?
The prognosis of osteoarthritis is good. Osteoarthritis is not reversible.
What is Rheumatoid Arthritis?
Rheumatoid arthritis is an autoimmune disorder that results in chronic inflammation of the joints.
What is the Pathology of Rheumatoid Arthritis?
The pathology of rheumatoid arthritis is:
-Etiology: Rheumatoid arthritis is an autoimmune condition.
-Genes involved: None.
-Pathogenesis: The pathogenesis of RA is not completely understood, but is thought to be due to external triggers which may include cigarette smoke, infection, or trauma. These triggers are believed to set off an autoimmune reaction that leads to synovial hypertrophy and chronic joint inflammation.
-Histology: The histology associated with rheumatoid arthritis shows perivascular mononuclear cell infiltrate in the synovium
How does Rheumatoid Arthritis Present?
Patients with rheumatoid arthritis typically present with joint stiffness, pain, swelling, and decreased movement of the affected joints. The smaller joints of the hands and feet are most commonly affected. Stiffness is usually worse in the morning.
How is Rheumatoid Arthritis Diagnosed?
Rheumatoid arthritis is diagnosed by blood tests, and radiographic imaging.
How is Rheumatoid Arthritis Treated?
Rheumatoid arthritis may be treated by disease-modifying antirheumatic drugs. There is no cure for rheumatoid arthritis.
What is the Prognosis of Rheumatoid Arthritis?
The prognosis of rheumatoid arthritis is good.
What is Juvenile Idiopathic Arthritis?
Juvenile idiopathic arthritis is a group of disorders characterized by arthritis in children.
What is the Pathology of Juvenile Idiopathic Arthritis?
The pathology of juvenile idiopathic arthritis is:
-Etiology: The cause of juvenile idiopathic arthritis is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to juvenile idiopathic arthritis is not known.
-Histology: The histology associated with juvenile idiopathic arthritis shows mixed infiltrating inflammatory cells, hyperplasia of synoviocytes, endothelial hyperplasia, and hyperemia.
How does Juvenile Idiopathic Arthritis Present?
Patients with juvenile idiopathic arthritis typically present with joint inflammation before 16 years of age that lasts for six weeks or more.
How is Juvenile Idiopathic Arthritis Diagnosed?
Juvenile idiopathic arthritis is diagnosed by clinical history, physical, radiographic imaging, and excluding other causes of the symptoms.
How is Juvenile Idiopathic Arthritis Treated?
Juvenile idiopathic arthritis is treated with NSAIDs, steroids, and DMARDS.
What is the Prognosis of Juvenile Idiopathic Arthritis?
The prognosis of juvenile idiopathic arthritis is good.
What are Seronegative Spondyloarthropathies?
Seronegative spondyloarthropathies are a group of disorders that involve sacroiliac joints and are associated with HLA-B27.
Examples of seronegative spondyloarthropathies include:
Ankylosing spondyloarthritis
Enteritis associated arthritis
Psoriatic arthritis
Reactive arthritis
What is Ankylosing Spondyloarthritis?
Ankylosing Spondyloarthritis is a type of arthritis that mainly affects the spine.
What is the Pathology of Ankylosing Spondyloarthritis?
The pathology of ankylosing spondyloarthritis is:
-Etiology: The cause of ankylosing spondyloarthritis is unknown.
-Genes involved: HLA-B27.
-Pathogenesis: The sequence of events that lead to ankylosing spondyloarthritis is HLA-B27 associated inflammation of the spinal joints.
-Histology: The histology associated with ankylosing spondyloarthritis shows diffuse lymphocytes and plasma cells infiltrate. Lymphoid follicles may also be present.
How does Ankylosing Spondyloarthritis Present?
Patients with ankylosing spondyloarthritis may be male or female. Symptoms typically begin before 45 years of age. The symptoms, features, and clinical findings associated with ankylosing spondyloarthritis include insidious onset of back pain in the sacroiliac joints, which progresses to involve other areas of the spine. Exercise helps ease the pain and stiffness.
How is Ankylosing Spondyloarthritis Diagnosed?
Ankylosing spondyloarthritis is diagnosed with physical examinations, laboratory tests, and imaging studies.
How is Ankylosing Spondyloarthritis Treated?
Ankylosing spondyloarthritis is treated with physical therapy and NSAIDS.
What is the Prognosis of Ankylosing Spondyloarthritis?
The prognosis of ankylosing spondyloarthritis is fair.
What is Enteritis Associated Arthritis?
Enteritis-associated arthritis is a type of chronic, inflammatory arthritis associated with inflammatory bowel disease.
What is the Pathology of Enteritis Associated Arthritis?
The pathology of enteritis associated arthritis is:
-Etiology: The cause of enteritis-associated arthritis is unknown at this time.
-Genes involved: HLA-B27.
-Pathogenesis: The sequence of events that lead to enteritis-associated arthritis is not completely understood.
-Histology: The histology associated with enteritis-associated arthritis shows extensive cryptitis, crypt abscesses, and crypt destruction.
How does Enteritis Associated Arthritis Present?
Patients with enteritis-associated arthritis are typically either male or female, with arthritis and inflammatory bowel disease.
How is Enteritis Associated Arthritis Diagnosed?
Enteritis-associated arthritis is diagnosed through a complete medical examination, and laboratory tests.
How is Enteritis Associated Arthritis Treated?
Enteritis associated arthritis is treated using corticosteroids, DMARDs, anti-TNFα, or Intra-articular injections.
What is the Prognosis of Enteritis Associated Arthritis?
The prognosis of enteritis-associated arthritis in the elderly is good, however, there is increased mortality associated with younger patients.
What is Psoriatic Arthritis?
Psoriatic arthritis is a type of inflammatory arthritis that occurs in a subset of patients with psoriasis.
What is the Pathology of Psoriatic Arthritis?
The pathology of psoriatic arthritis is:
-Etiology: The cause of psoriatic arthritis is unknown. Heredity may play a role.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to psoriatic arthritis include potential triggers such as trauma, stress, environmental factors, infections, obesity, and smoking.
-Histology: The histology associated with psoriatic arthritis shows predominantly tortuous, bushy vessels
How does Psoriatic Arthritis Present?
Psoriatic arthritis usually appears in people between the ages of 30 to 50 years old. Symptoms vary from person to person but typically include arthritis and psoriasis.
How is Psoriatic Arthritis Diagnosed?
Psoriatic arthritis is diagnosed through various tests. X-rays often are taken to look for joint damage. MRI, ultrasound, or CT scans can be used to look at the joints in more detail. Blood tests may be done to rule out other types of arthritis that have similar signs and symptoms, including gout, osteoarthritis, and rheumatoid arthritis.
How is Psoriatic Arthritis Treated?
Psoriatic arthritis is treated with NSAIDs, DMARDS, and TNF inhibitors.
What is the Prognosis of Psoriatic Arthritis?
The prognosis of psoriatic arthritis is fair.
What is Reactive Arthritis?
Reactive Arthritis is a painful type of inflammatory arthritis in reaction to an infection.
What is the Pathology of Reactive Arthritis?
The pathology of reactive arthritis is:
-Etiology: The cause of reactive arthritis is an infectious organism, most commonly Chlamydia trachomatis.
-Genes involved: HLA-B27.
-Pathogenesis: The sequence of events that lead to reactive arthritis is triggered by an infection.
-Histology: The histology associated with reactive arthritis shows macrophages, Reiter cells, and mixed inflammatory infiltrate.
How does Reactive Arthritis Present?
Patients with reactive arthritis are typically men between ages 20 and 50. Some patients with reactive arthritis carry a gene called HLA-B27. Patients who test positive for HLA-B27 often have a more sudden and severe onset of symptoms. The classic triad of symptoms includes conjunctivitis, non-infectious urethritis, and arthritis.
How is Reactive Arthritis Diagnosed?
Reactive arthritis is diagnosed clinically. If indicated a Chlamydia infection test may be obtained.
How is Reactive Arthritis Treated?
Reactive arthritis is treated with NSAIDS and DMARDS.
What is the Prognosis of Reactive Arthritis?
The prognosis of reactive arthritis is good, and symptoms typically resolve in about four months.
What is Infectious Arthritis?
Infectious arthritis is a painful infection in the joint. Infectious arthritis usually occurs in only one joint.
Examples of infectious arthritis include:
Lyme arthritis
Mycobacterial arthritis
Suppurative arthritis
Viral arthritis
What is Lyme Arthritis?
Lyme arthritis is caused by Lyme disease infection of the joint.
What is the Pathology of Lyme Arthritis?
The pathology of Lyme arthritis is:
-Etiology: The cause of Lyme arthritis is bacteria.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to Lyme arthritis includes spirochete-induced activity that induces infiltration of mononuclear cells into the synovial tissue.
-Histology: The histology associated with Lyme arthritis shows papillary synovitis, mononuclear cellular infiltrate, and fibrin deposition. Onion skin thickening of arterial walls may also be present.
How does Lyme Arthritis Present?
Patients with Lyme arthritis are typically male or female. The main feature of Lyme arthritis is swelling of the affected joints. The joint may feel warm, and painful.
How is Lyme Arthritis Diagnosed?
Lyme arthritis is diagnosed with serologic testing or synovial fluid PCR testing.
How is Lyme Arthritis Treated?
Lyme arthritis is treated using oral antibiotics.
What is the Prognosis of Lyme Arthritis?
The prognosis of Lyme arthritis is good when they are treated early with appropriate antibiotic regimens.
What is Mycobacterial Arthritis?
Mycobacterial arthritis is an infection of the joints due to tuberculosis
What is the Pathology of Mycobacterial Arthritis?
The pathology of mycobacterial arthritis is:
-Etiology: Mycobacterial arthritis is caused by infection by several different mycobacterial organisms which include M. tuberculosis, M. kansasii, M. Bovis, and M. leprae among others.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to mycobacterial arthritis is not known.
-Histology: The histology associated with mycobacterial arthritis shows multiple well-formed, epithelioid granulomas, lacking caseous necrosis.
How does Mycobacterial Arthritis Present?
Patients with mycobacterial arthritis are typically older males or females. Symptoms typically include decreased movement in the affected joints, and night sweats.
How is Mycobacterial Arthritis Diagnosed?
Mycobacterial arthritis is diagnosed by aspiration of fluid in the joint.
How is Mycobacterial Arthritis Treated?
Mycobacterial arthritis is treated using antibiotics and steroids.
What is the Prognosis of Mycobacterial Arthritis?
The prognosis of mycobacterial arthritis is poor, and may result in joint destruction. Controlling the infection is important to prevent involving more joints.
What is Suppurative Arthritis?
Suppurative arthritis is an infection in the synovial fluid and joint tissues.
What is the Pathology of Suppurative arthritis?
The pathology of suppurative arthritis is:
-Etiology: The cause of suppurative arthritis is a bacterial infection.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to suppurative arthritis includes seeding of the joint with bacteria, most commonly Staphylococcus, Streptococcus, or gram-negative rods. Syphilis may also cause suppurative arthritis.
-Histology: The histology associated with suppurative arthritis shows neutrophils and bacteria.
How does Suppurative Arthritis Present?
Patients with suppurative arthritis are typically either male or female. The clinical features include extreme pain, chills. fatigue and generalized weakness, fever, and inability to move the affected joint.
How is Suppurative Arthritis Diagnosed?
Suppurative arthritis diagnosis is made by analysis of fluid that has been removed from the joint, including microscopic examination and culture.
How is Suppurative Arthritis Treated?
Suppurative arthritis requires drainage of the joint and antibiotics, usually intravenously administered.
What is the Prognosis of Suppurative Arthritis?
The prognosis of suppurative arthritis is fair if treated in a timely manner.
What is Viral Arthritis?
Viral arthritis is inflammation of the joints from a viral infection.
What is the Pathology of Viral Arthritis?
The pathology of viral arthritis is:
-Etiology: The cause of viral arthritis is a viral infection, the most common of which includes parvovirus B19, chikungunya, and dengue.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to viral arthritis involves immune complex mediated antibodies being deposited at sites of viral infection or in the synovium which causes virus-induced autoimmunity.
-Histology: The histology associated with viral arthritis shows mixed inflammatory infiltrate, and hypertrophic synovial cells.
How does Viral Arthritis Present?
Patients with viral arthritis typically are males or females. They commonly have symmetrical small-joint involvement.
How is Viral Arthritis Diagnosed?
Viral arthritis is diagnosed using aspiration and radiologic findings.
How is Viral Arthritis Treated?
Viral arthritis is treated with simple analgesics or NSAIDs.
What is the Prognosis of Viral Arthritis?
The prognosis of viral arthritis is good. The disease is generally mild and self-limited, typically lasting no longer than three weeks.
What is Crystal Induced Arthritis?
Crystal-induced arthropathies are a group of disorders that involve crystal deposition in joints that result in arthritis.
Examples of crystal-induced arthritis include:
Pseudogout (calcium pyrophosphate crystal deposition disease)
Gout
What is Pseudogout?
Pseudo-gout is a form of arthritis that results from deposits of calcium pyrophosphate crystals.
What is the Pathology of Pseudogout?
The pathology of pseudo-gout is:
-Etiology: The cause of pseudogout is the deposits of calcium pyrophosphate dihydrate crystals in the joint.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to pseudo-gout involves formation of calcium pyrophosphate dihydrate (CPPD) crystals in the cartilage of the synovial fluid.
-Histology: The histology associated with pseudogout shows pale pink areas that may be surrounded by histiocytes and multinucleated giant cells. Rhomboid crystals may be appreciated.
How does Pseudogout Present?
Patients with pseudogout are typically over 60 years old, and are of any gender. The symptoms of pseudo-gout typically include swelling, pain, stiffness, and warmth in large joints.
How is Pseudogout Diagnosed?
Pseudo-gout is diagnosed by assessing the synovial fluid from the inflamed joint.
How is Pseudogout Treated?
Pseudo-gout is treated with NSAIDs and corticosteroids.
What is the Prognosis of Pseudogout?
The prognosis of pseudo-gout is very good in acute attacks. Acute attacks of pseudogout usually resolve within 10 days.
What is Gout?
Gout is a common form of inflammatory arthritis that is very painful.
What is the Pathology of Gout?
The pathology of gout is:
-Etiology: Gout is caused by accumulation of uric acid.
-Genes involved: None.
-Pathogenesis: Uric acid crystals (monosodium urate) build up in joints.
-Histology: The histology associated with gout shows urate crystals and histiocytes.
How does Gout Present?
Patients with gout typically present in older males or females with old age. Symptoms typically include sudden painful monoarthritis.
How is Gout Diagnosed?
Gout is diagnosed by assessing the symptoms and the results of the physical examination, X-rays, and lab tests.
How is Gout Treated?
Gout is treated and managed with medical treatment and self-management strategies. Treatment options include nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, steroids, anti-inflammatory drug colchicine, allopurinol, febuxostat, and pegloticase.
What is the Prognosis of Gout?
The prognosis of gout is fair when managed properly.
What are Joint Tumors?
Joint tumors are synovial tumors and can be categorized into benign tumors and malignant tumors.
Examples of joint tumors and joint tumor-like conditions are:
Ganglion cysts
Synovial cysts
Tenosynovial giant cell tumor
What are Ganglion Cysts?
Ganglion cysts are nodular lesions that most commonly develop in the wrist.
What is the Pathology of Ganglion Cysts?
The pathology of ganglion cysts is:
-Etiology: The cause of ganglion cysts is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to ganglion cysts is unknown.
-Histology: The histology associated with ganglion cysts shows cystic lesions that are lined by connective tissue. Ganglion cysts are typically composed of bland spindle-shaped cells in a background of myxoid matrix.
How does Ganglion Cysts Present?
Patients with ganglion cysts typically present with pain, and a subcutaneous nodule.
How are Ganglion Cysts Diagnosed?
Ganglion cysts are usually diagnosed utilizing physical examination, ultrasound, and needle aspiration.
How Are Ganglion Cysts Treated?
Many ganglion cysts resolve on their own. Needle aspiration or surgery may be considered for certain patients.
What is the Prognosis of Ganglion Cysts?
The prognosis of ganglion cysts is good.
What are Synovial Cysts?
Synovial cysts are abnormal fluid-filled sacs in joints in the spine.
What is the Pathology of Synovial Cysts?
The pathology of synovial cysts is:
-Etiology: The cause of synovial cysts is a result of degenerative changes associated with aging.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to synovial cysts remains unclear.
-Histology: The histology associated with synovial cysts shows pseudocysts and degenerative changes. There may be granular calcifications and a foreign body giant cell reaction.
How do Synovial Cysts Present?
Patients with synovial cysts are typically males or females over 65 years old. Symptoms depend on the size and location of the cyst, but are typically only a nodule and milde pressure discomfort.
How are Synovial Cysts Diagnosed?
Synovial cysts are diagnosed using X-ray and MRI.
How are Synovial Cysts Treated?
Synovial cysts are treated with pain medication and seeking physical therapy.
What is the Prognosis of Synovial Cysts?
The prognosis of synovial cysts is fair. The symptoms and level of pain or discomfort may remain stable for many years.
What is Tenosynovial Giant Cell Tumor?
Tenosynovial giant cell tumors are a group of rare, benign tumors that involve bursae, synovium, and tendon sheath.
What is the Pathology of Tenosynovial Giant Cell Tumor?
The pathology of tenosynovial giant cell tumor is:
-Etiology: The cause of tenosynovial giant cell tumor is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to tenosynovial giant cell tumors is unknown.
-Histology: The histology associated with tenosynovial giant cell tumors shows mononuclear stromal cells with small round nuclei.
How does Tenosynovial Giant Cell Tumor Present?
Patients with tenosynovial giant cell tumors are males or females typically between 25 and 40 years old. The signs and symptoms of tenosynovial giant cell tumors vary depending upon the location, but tend to include swelling.
How is Tenosynovial Giant Cell Tumor Diagnosed?
Tenosynovial giant cell tumor is diagnosed using X-ray and MRI.
How is Tenosynovial Giant Cell Tumor Treated?
Tenosynovial giant cell tumor is treated using surgical excision.
What is the Prognosis of Tenosynovial Giant Cell Tumor?
The prognosis of tenosynovial giant cell tumors is fair.