Kidney pathology is any disease or disorder that affects the kidney.
Kidney pathology includes:
- Anomalies of the kidney
- Cystic diseases of the kidney
- Glomerular diseases
- Tubular and interstitial diseases
- Vascular diseases
- Urinary tract obstruction
- Neoplasms of the kidney
What are Anomalies of the Kidney?
Anomalies of the kidney are ailments affecting the normal functions of the kidney; excretion, fluid and salt regulation, hormonal secretion, and acid balance. The diseases also affect the normal anatomic structure of the kidney. Anomalies of the kidney may be congenital or developmental.
What are Congenital Anomalies?
Congenital anomalies of the kidney are congenital renal malformations that could be hereditary and result from acquired defects throughout the gestation period.
Examples of congenital anomalies of the kidney include:
- Agenesis of the kidney
- Hypoplasia of the kidney
- Ectopic kidney
- Horseshoe kidney
What is Agenesis of the Kidney?
Agenesis of the kidney is a congenital anomaly in which the individual lacks one kidney unilateral agenesis or lacks both kidneys total bilateral agenesis.
What is the Pathology of Agenesis of the Kidney?
The pathology of agenesis of the kidney is:
-Etiology: The cause of agenesis of the kidney is idiopathic, genetic, other congenital anomalies,
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to agenesis of the kidney is unknown.
-Morphology: The morphology associated with agenesis of the kidney shows the absence of one or both kidneys, hypertrophy of the remaining kidney.
How does Agenesis of the Kidney Present?
Patients with agenesis of the kidney are typically more frequent in male infants present at the age range of infancy period. The symptoms, features, and clinical findings associated with agenesis of the kidney include absence of one or both kidneys on imaging, absence of urine, wide-set eyes, receding chin, ears with reduced cartilage, dehydrated skin, hands, and feet deformities.
How is Agenesis of the Kidney Diagnosed?
Agenesis of the kidney is diagnosed through sonographic investigations, prenatal ultrasound
How is Agenesis of the Kidney Treated?
Agenesis of the kidney is treated through symptomatic and supportive care, dialysis. Surgical intervention kidney transplant.
What is the Prognosis of Agenesis of the Kidney?
The prognosis of agenesis of the kidney is poor in case of bilateral agenesis, it is incompatible with life.
What is Hypoplasia of the Kidney?
Hypoplasia of the kidney is the condition of the kidney characterized by failure to develop into the normal anatomical size.
What is the Pathology of Hypoplasia of the Kidney?
The pathology of hypoplasia of the kidney is:
-Etiology: The cause of hypoplasia of the kidney is genetic factors, congenital, acquired as a result of vesicular infection,
-Genes involved: PAX2, RET, GDNF, WT1 (Wilms tumor 1), wnt-4 genes.
-Pathogenesis: The sequence of events that lead to hypoplasia of the kidney result from arrested development of kidney tissues at 14- 20 gestational weeks.
-Morphology: The morphology associated with hypoplasia of the kidney shows small kidneys with hypertrophied and reduced number of nephrons.
-Histology: The histology associated with hypoplasia of the kidney shows few tubules, loose interstitial tissue, no/rare glomeruli and little or/no inflammation.
How does Hypoplasia of the Kidney Present?
Patients with hypoplasia of the kidney typically have a male predominance present at age range of prenatally and at childhood. The symptoms, features, and clinical findings associated with hypoplasia of the kidney include polyuria, polydipsia, proteinuria, short stature, and tapetoretinal dystrophy.
How is Hypoplasia of the Kidney Diagnosed?
Hypoplasia of the kidney is diagnosed through laboratory studies such as urinalysis proteinuria present, BUN, electrolyte and creatinine levels, hematocrit level. Imaging studies such as renal ultrasonography shows small sized kidneys.
How is Hypoplasia of the Kidney Treated?
Hypoplasia of the kidney is treated through medical supportive care, angiotensin-converting enzyme inhibitors. Surgical care and kidney transplant may be needed.
What is the Prognosis of Hypoplasia of the Kidney?
The prognosis of hypoplasia of the kidney is fair. A progressive disorder associated with kidney failure.
What is Ectopic Kidney?
Ectopic kidney is the kidney that is not located in its normal anatomic position.
What is the Pathology of Ectopic Kidney?
The pathology of ectopic kidney is:
-Etiology: The cause of ectopic kidney is idiopathic, congenital factors.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to ectopic kidney is not well understood.
-Morphology: The morphology associated with an ectopic kidney shows a normal or small sized kidney in an unusual position.
-Histology: Glomeruli and or tubules.
How does Ectopic Kidney Present?
Patients with ectopic kidney typically have no gender prevalence reported present at the age range of prenatal to adulthood. The symptoms, features, and clinical findings associated with ectopic kidney include; asymptomatic, urine retention, urinary frequency, frequent UTI, kidney stones, abdomen lump or mass, blood pressure.
How is Ectopic Kidney Diagnosed?
Ectopic kidney is diagnosed through lab work- Kidney function test. Imaging- prenatal ultrasound, MRI, x-ray.
How is Ectopic Kidney Treated?
Ectopic kidney is treated through symptomatic and supportive care.
What is the Prognosis of Ectopic Kidney?
The prognosis of ectopic kidney is good.
What is Horseshoe Kidney?
Horseshoe kidney is a congenital condition characterized by the fusion of the upper or lower poles of the kidneys.
What is the Pathology of Horseshoe Kidney?
The pathology of horseshoe kidney is:
-Etiology: The cause of horseshoe kidney is idiopathic, teratogenic event,
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to horseshoe kidney not understood.
-Morphology: The morphology associated with horseshoe kidney shows fused kidneys.
How does Horseshoe Kidney Present?
Patients with horseshoe kidney typically twice more common in males than females present at age range prenatal. The symptoms, features, and clinical findings associated with horseshoe kidney include asymptomatic, frequent UTI, abdominal pain, nausea, abdominal swelling and fullness.
How is Horseshoe Kidney Diagnosed?
Horseshoe kidney is diagnosed through laboratory studies such asurinalysis, and serum chemistry with creatinine for baseline renal function. Imaging studies such as CT scanning of the abdomen and pelvis. Voiding cystourethrography rules out vesicoureteral reflux.
How is Horseshoe Kidney Treated?
Horseshoe kidney is treated through symptomatic and supportive care. Surgical care therapy.
What is the Prognosis of Horseshoe Kidney?
The prognosis of horseshoe kidney is good. Presence of the condition alone doesn’t affect survival.
What are Cystic Diseases of the Kidney?
Cystic diseases of the kidney comprise a heterogeneous group of hereditary, developmental but nonhereditary, and acquired syndromes.
Examples of cystic diseases of the kidney include:
- Autosomal dominant polycystic kidney disease
- Autosomal recessive polycystic kidney disease
- Cystic diseases of the renal medulla
- Multicystic renal dysplasia
- Simple cysts
- Acquired (dialysis-associated) cystic disease
What is Autosomal Dominant Polycystic Kidney Disease?
Autosomal dominant polycystic kidney disease is a genetic disorder also called adult polycystic kidney disease, characterized by renal failure following multiple expanding cysts of both kidneys that eventually destroy the renal parenchyma.
What is the Pathology of Autosomal Dominant Polycystic Kidney Disease?
The pathology of autosomal dominant polycystic kidney disease is:
-Etiology: The cause of autosomal dominant polycystic kidney disease is genetic.
-Genes involved: PKD1 and PKD2 gene.
-Pathogenesis: The sequence of events that lead to autosomal dominant polycystic kidney disease follows a range of dissimilar mutations in PKD1 and PKD2 leading to numerous cellular fluctuations allied with cyst advancement.
-Morphology: The morphology associated with autosomal dominant polycystic kidney disease shows bilaterally enlargement of kidneys, composition of cyst masses.
-Histology: The histology associated with autosomal dominant polycystic kidney disease shows operational nephrons dispersed between the cysts which are filled with turbid, red to brown fluid.
How does Autosomal Dominant Polycystic Kidney Disease Present?
Patients with autosomal dominant polycystic kidney disease typically high in males present at the age range of 50 to 70 years. The symptoms, features, and clinical findings associated with autosomal dominant polycystic kidney disease include asymptomatic, abdominal masses, proteinuria, polyuria, and hypertension.
How is Autosomal Dominant Polycystic Kidney Disease Diagnosed?
Autosomal dominant polycystic kidney disease is diagnosed through imaging studies such as ultrasonography, CT scan, MRI/MRA. Laboratory studies such as genetic study, serum chemistry profile, urine culture, uric acid determination, intact parathyroid hormone assay.
How is Autosomal Dominant Polycystic Kidney Disease Treated?
Autosomal dominant polycystic kidney disease is treated through pharmacological therapy for symptomatic support, vasopressin V2-receptor antagonist (tolvaptan). Surgical drainage of cystic fluid fill.
What is the Prognosis of Autosomal Dominant Polycystic Kidney Disease?
The prognosis of autosomal dominant polycystic kidney disease is fair.
What is Autosomal Recessive Polycystic Kidney Disease?
Autosomal recessive polycystic kidney disease is a rare developmental anomaly also called Childhood polycystic kidney disease characterized by an autosomal-recessive type of inheritance.
What is the Pathology of Autosomal Recessive Polycystic Kidney Disease?
The pathology of autosomal recessive polycystic kidney disease is:.
-Etiology: The cause of autosomal recessive polycystic kidney disease is genetic.
-Genes involved: PKHD1.
-Pathogenesis: The sequence of events that lead to autosomal recessive polycystic kidney disease follow mutation of the PKHD1 gene.
-Morphology: The morphology associated with autosomal recessive polycystic kidney disease shows enlarged kidney, renal collecting duct dilatation and elongation. Small cysts in the cortex and medulla.
-Histology: The histology associated with autosomal recessive polycystic kidney disease shows cylindrical, saccular dilation of all collecting tubules.
How does Autosomal Recessive Polycystic Kidney Disease Present?
Patients with autosomal recessive polycystic kidney disease typically high in males present at the age range of infancy to childhood. The symptoms, features, and clinical findings associated with autosomal recessive polycystic kidney disease include abdominal masses, proteinuria, polyuria, and hypertension. Classic Potter facies.
How is Autosomal Recessive Polycystic Kidney Disease Diagnosed?
Autosomal recessive polycystic kidney disease is diagnosed through laboratory studies such as genetic testing, blood and urine studies, GFR, BUN, and urinalysis. Imaging studies such as abdominal radiography reveals enlarged kidney. Chest radiography reveals pulmonary hypertrophy.
How is Autosomal Recessive Polycystic Kidney Disease Treated?
Autosomal recessive polycystic kidney disease is treated through symptomatic medical care- antihypertensive therapy, (ACE) inhibitors, calcium channel blockers, and beta blockers. Surgical management.
What is the Prognosis of Autosomal Recessive Polycystic Kidney Disease?
The prognosis of autosomal recessive polycystic kidney disease is poor. Highly associated with end stage renal disease.
What is Cystic Disease of the Renal Medulla?
Cystic diseases of the renal medulla is a heterogeneous group of kidney disease comprising hereditary, developmental but nonhereditary, and acquired disorders.
Examples of cystic diseases of the renal medulla include:
- Adult-onset medullary cystic disease
- Medullary sponge kidney
- Nephronophthisis
What is Adult-Onset Medullary Cystic Disease?
Adult-onset medullary cystic disease is one of the variants of nephronophthisis-medullary cystic disease complex present in adults.
What is the Pathology of Adult-Onset Medullary Cystic Disease?
The pathology of adult-onset medullary cystic disease is:
-Etiology: The cause of adult-onset medullary cystic disease is genetic.
-Genes involved: MCKD1 and MCKD2.
-Pathogenesis: The sequence of events that lead to adult-onset medullary cystic disease results from MCKD1 and MCKD2 gene loci mutations with autosomal dominant transmission.
-Morphology: The morphology associated with adult-onset medullary cystic disease shows cysts.
-Histology: The histology associated with adult-onset medullary cystic disease shows
How does Adult-Onset Medullary Cystic Disease Present?
Patients with adult-onset medullary cystic disease typically affect both genders equally present at age range of 20 to 30 years. The symptoms, features, and clinical findings associated with adult-onset medullary cystic disease include polyuria, polydipsia, enuresis, dehydration, failure to thrive, weakness, and pallor.
How is Adult-Onset Medullary Cystic Disease Diagnosed?
Adult-onset medullary cystic disease is diagnosed by laboratory studies such as urinalysis, elevated serum BUN and creatinine concentrations, CBCs count, radiological studies such as plain radiograph, excretory urogram and CT scan.
How is Adult-Onset Medullary Cystic Disease Treated?
Adult-onset medullary cystic disease is treated through symptomatic management, renal replacement therapy- peritoneal, hemodialysis and kidney transplant.
What is the Prognosis of Adult-Onset Medullary Cystic Disease?
The prognosis of adult-onset medullary cystic disease is fair. Condition associated with ESRD.
What is Medullary Sponge Kidney?
Medullary sponge kidney is a benign congenital syndrome characterized by dilatation of collecting tubules in the renal papillae.
What is the Pathology of Medullary Sponge Kidney?
The pathology of medullary sponge kidney is:
-Etiology: The cause of medullary sponge kidney is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to medullary sponge kidney unknown.
-Morphology: The morphology associated with medullary sponge kidney shows dilated ducts and small cysts.
-Histology: The histology associated with medullary sponge kidney shows cysts lined with cuboidal epithelium or transitional epithelium.
How does Medullary Sponge Kidney Present?
Patients with medullary sponge kidney typically affect more females than males present at the age range of 20 to 30 years. The symptoms, features, and clinical findings associated with medullary sponge kidney include asymptomatic, hematuria, UTI, urinary obstruction, and nephrolithiasis.
How is Medullary Sponge Kidney Diagnosed?
Medullary sponge kidney is diagnosed by radiological studies such as plain radiograph, excretory urogram and CT scan.
How is Medullary Sponge Kidney Treated?
Medullary sponge kidney is treated by symptomatic management medical care, surgery extracorporeal shock wave lithotripsy, percutaneous surgery, ureteroscopy.
What is the Prognosis of Medullary Sponge Kidney?
The prognosis of medullary sponge kidney is good; it is a benign condition with low mortality and morbidity.
What is Nephronophthisis?
Nephronophthisis is a group of advancing renal conditions usually having their onset in childhood.
What is the Pathology of Nephronophthisis?
The pathology of nephronophthisis is:
-Etiology: The cause of nephronophthisis is genetic factors.
-Genes involved: NPH1, NPH2, NPH3, MCKD1 and MCKD2.
-Pathogenesis: The sequence of events that lead to nephronophthisis results from autosomal dominant and recessive modes of inheritance. NPH1, NPH2, NPH3, describe the juvenile type of nephronophthisis and cause autosomal recessive disease while MCKD1 and MCKD2 describes medullary cystic disease that is characterized by progression to end stage kidney disease in adult life.
-Morphology: The morphology associated with nephronophthisis shows small kidney, granular surface and small cysts.
-Histology: The histology associated with nephronophthisis shows cysts lined by flattened or cuboidal epithelium. Presence of inflammatory cells and fibrous tissues.
How does Nephronophthisis Present?
Patients with nephronophthisis typically affect both genders equally present at age range of childhood. The symptoms, features, and clinical findings associated with nephronophthisis include polyuria, polydipsia, enuresis, dehydration, failure to thrive, weakness, and pallor.
How is Nephronophthisis Diagnosed?
Nephronophthisis is diagnosed by laboratory studies such as urinalysis, elevated serum BUN and creatinine concentrations, CBCs count, radiological studies such as plain radiograph, excretory urogram and CT scan.
How is Nephronophthisis Treated?
Nephronophthisis is treated through symptomatic management, renal replacement therapy- peritoneal, hemodialysis and kidney transplant.
What is the Prognosis of Nephronophthisis?
The prognosis of nephronophthisis is fair, ESRD develops in all patients with NPH.
What is Multicystic Renal Dysplasia?
Multicystic renal dysplasia is a variant of renal dysplasia, most frequently recognized congenital anomalies to the urinary tract.
What is the Pathology of Multicystic Renal Dysplasia?
The pathology of multicystic renal dysplasia is:
-Etiology: The cause of multicystic renal dysplasia is a congenital, genetic factor.
-Genes involved: EYA1, SIX1 genes
-Pathogenesis: The sequence of events that lead to multicystic renal dysplasia results as a sporadic problem, familiar occurrence reported, EYA1 or SIX1 genes gene mutations in ureteric bud development.
-Morphology: The morphology associated with multicystic renal dysplasia shows the kidney is enlarged and abnormally shaped, irregularly sized cysts.
-Histology: The histology associated with multicystic renal dysplasia shows fibrous tissue stroma.
How does Multicystic Renal Dysplasia Present?
Patients with multicystic renal dysplasia typically slightly higher in males present at the age range of childhood. The symptoms, features, and clinical findings associated with multicystic renal dysplasia include flank abdominal mass, respiratory distress, voiding dysfunction, and hypertension,
How is Multicystic Renal Dysplasia Diagnosed?
Multicystic renal dysplasia is diagnosed in laboratory studies such as urinalysis, creatinine levels, electrolytes levels, and blood pressure. Imaging studies such as renal ultrasonography, voiding cystourethrography, dimercaptosuccinic acid (DMSA) renal scanning, and intravenous pyelography.
How is Multicystic Renal Dysplasia Treated?
Multicystic renal dysplasia is treated by symptomatic management.
What is the Prognosis of Multicystic Renal Dysplasia?
The prognosis of multicystic renal dysplasia is fair. Depends on whether the involvement is unilateral or bilateral.
What are Simple Cysts of the Kidney?
Simple cysts of the kidney are cysts occurring as single or multiple fluid-filled sacs in one or both kidneys.
What is the Pathology of Simple Cysts of the Kidney?
The pathology of simple cysts of the kidney is:
-Etiology: The cause of simple cysts of the kidney is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to simple cysts of the kidney is unclear.
-Morphology: The morphology associated with simple cysts of the kidney shows various size cysts.
-Histology: The histology associated with simple cysts of the kidney shows a simple cuboidal or flattened epithelial lining.
How does Simple Cysts of the Kidney Present?
Patients with simple cysts of the kidney typically higher in males present at the age range of 40 years and above. The symptoms, features, and clinical findings associated with simple cysts are typically unknown.
How is Simple Cysts of the Kidney Diagnosed?
Simple cysts of the kidney are diagnosed by a CT scan or ultrasound indicating an anechoic, thin imperceptible wall.
How is Simple Cysts of the Kidney Treated?
Simple cysts of the kidney are treated by antibiotics in case of infected cyst. Surgical drainage, aspiration and sclerotherapy. Laparoscopic surgery to remove the cyst.
What is the Prognosis of Simple Cysts of the Kidney?
The prognosis of simple cysts of the kidney is good. Do not affect mortality and/or morbidity.
What is Acquired (Dialysis-Associated) Cystic Disease?
Acquired (dialysis-associated) cystic disease is numerous cortical and medullary cysts associated with prolonged dialysis due to end stage renal failure.
What is the Pathology of Acquired (Dialysis-Associated) Cystic Disease?
The pathology of acquired (dialysis-associated) cystic disease is:
-Etiology: The cause of acquired (dialysis-associated) cystic disease is dialysis-associated.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to acquired (dialysis-associated) cystic disease form as a result of impediment of tubules by interstitial fibrosis or by oxalate crystals.
-Morphology: The morphology associated with acquired (dialysis-associated) cystic disease shows cysts measuring 0.5 to 2 cm in diameter, containing clear fluid.
-Histology: The histology associated with acquired (dialysis-associated) cystic disease shows cysts lined with either hyperplastic or flattened tubular epithelium.
How does Acquired (Dialysis-Associated) Cystic Disease Present?
Patients with acquired (dialysis-associated) cystic disease typically have no gender preference present at the age range of adulthood. The symptoms, features, and clinical findings associated with acquired (dialysis-associated) cystic disease include asymptomatic, hematuria.
How is Acquired (Dialysis-Associated) Cystic Disease Diagnosed?
Acquired (dialysis-associated) cystic disease is diagnosed by a medical history, Imaging tests- ultrasound, CT scan, MRI.
How is Acquired (Dialysis-Associated) Cystic Disease Treated?
Acquired (dialysis-associated) cystic disease is treated by symptomatic management, antibacterial. Surgical interventions- drainage, tumor removal and kidney transplant.
What is the Prognosis of Acquired (Dialysis-Associated) Cystic Disease?
The prognosis of acquired (dialysis-associated) cystic disease is good. The condition does not cause many complications.
What are Glomerular Diseases?
Glomerular diseases are anomalies of the glomerular part of the kidney constituting major problems in nephrology.
Glomerular disease may be due to one or more of the following:
- Activation of alternative complement pathway
- Antibodies against components of the glomerular basement membrane
- Cell-mediated immunity in glomerulonephritis
- Deposition of circulating immune complexes
- Epithelial cell injury
- In situ formation of immune complexes
- Glomerular injury following immune complex formation
Examples of glomerular disease include:
- Nephrotic syndromes
- Nephritic syndromes
- Isolated glomerular abnormalities
- Chronic glomerulonephritis
What are Nephrotic Syndromes?
Nephrotic syndromes are clinical complexes that includes; massive proteinuria, hypoalbuminemia, generalized edema, hyperlipidemia and lipiduria.
Examples of nephrotic syndrome include:
- Dense deposit disease
- Focal segmental glomerulosclerosis
- Membranoproliferative glomerulonephritis
- Membranous nephropathy
- Minimal change disease
What is Dense Deposit Disease?
Dense deposit disease is an infrequent autoimmune condition that affecting the kidneys
What is the Pathology of Dense Deposit Disease?
The pathology of dense deposit disease is:
-Etiology: The cause of dense deposit disease is genetic and non-genetic factors
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to dense deposit disease is less clear, abnormality in excessive complement activation and complement regulatory protein factor H gene mutations.
-Morphology: The morphology associated with dense deposit disease shows large glomeruli, with an accentuated lobular appearance.
-Histology: The histology associated with dense deposit disease shows proliferation of mesangial and endothelial cells and infiltrating leukocytes.
How does Dense Deposit Disease Present?
Patients with dense deposit disease typically have no gender preference present at the age range of 5 to 15 years. The symptoms, features, and clinical findings associated with dense deposit disease include proteinuria, reduced amounts of urine, hematuria, blood pressure and swelling.
How is Dense Deposit Disease Diagnosed?
Dense deposit disease is diagnosed by kidney biopsy.
How is Dense Deposit Disease Treated?
Dense deposit disease is treated through symptomatic management, aggressive blood pressure control, angiotensin-converting enzyme (ACE) inhibitors and angiotensin II type-1 receptor blockers therapy, peritoneal dialysis or hemodialysis and kidney transport.
What is the Prognosis of Dense Deposit Disease?
The prognosis of dense deposit disease is fair.
What is Focal Segmental Glomerulosclerosis?
Focal segmental glomerulosclerosis is a glomerular disease in adults characterized by sclerosis of some, but not all, glomeruli and only a portion of the capillary tuft is involved.
What is the Pathology of Focal Segmental Glomerulosclerosis?
The pathology of focal segmental glomerulosclerosis is:
-Etiology: The cause of focal segmental glomerulosclerosis is idiopathic, drugs, toxins, infections, and intrarenal hemodynamic alterations.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to focal segmental glomerulosclerosis is not clear.
-Morphology: The morphology associated with focal segmental glomerulosclerosis shows solidification of the glomerular tuft.
-Histology: The histology associated with focal segmental glomerulosclerosis shows accumulation of acellular matrix and hyaline deposits.
How does Focal Segmental Glomerulosclerosis Present?
Patients with focal segmental glomerulosclerosis are typically more common in males present at the age range of 18-45 years. The symptoms, features, and clinical findings associated with focal segmental glomerulosclerosis include leg edema, ascites, pleural effusion, abdominal pain, ulcerations, and hypertension.
How is Focal Segmental Glomerulosclerosis Diagnosed?
Focal segmental glomerulosclerosis is diagnosed through the clinical presentation, laboratory studies such as urinalysis, serum creatinine concentration, albumin levels, lipid studies. Imaging studies such as kidney ultrasonography.
How is Focal Segmental Glomerulosclerosis Treated?
Focal segmental glomerulosclerosis is treated by nonspecific measures, symptomatic treatment. Immunosuppressants, loop diuretics, angiotensin-converting enzyme inhibitors, potassium-sparing diuretics.
What is the Prognosis of Focal Segmental Glomerulosclerosis?
The prognosis of focal segmental glomerulosclerosis is fair.
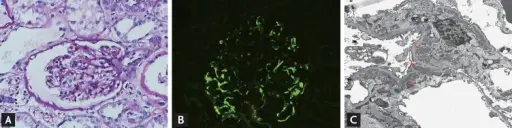
What is Membranoproliferative Glomerulonephritis?
Membranoproliferative glomerulonephritis is a disease of the glomerular caused by an abnormal immune response.
What is the Pathology of Membranoproliferative Glomerulonephritis?
The pathology of membranoproliferative glomerulonephritis is the scientific study of the abnormal immune response that leads to glomerulonephritis.
-Etiology: The cause of membranoproliferative glomerulonephritis is an autoimmune response, malignancies, infections,
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to membranoproliferative glomerulonephritis is the deposition of antibodies in the glomerular membrane damaging the membrane hindering it from performing its function normally.
-Morphology: The morphology associated with membranoproliferative glomerulonephritis shows thickening of the capillary walls, diffuse mesangial cell proliferation.
-Histology: The histology associated with membranoproliferative glomerulonephritis shows chunky irregular capillary wall mesangial deposits, endocapillary proliferation.
How does Membranoproliferative Glomerulonephritis Present?
Patients with membranoproliferative glomerulonephritis typically are female and young children present at the age range of 2-30 years. The symptoms, features, and clinical findings associated with membranoproliferative glomerulonephritis include edema, azotemia, cloudy urine, tea-colored urine, reduced urine output.
How is Membranoproliferative Glomerulonephritis Diagnosed?
Membranoproliferative glomerulonephritis is diagnosed by physical examination and history taking, urinalysis, protein levels in urine, creatinine levels, and a kidney biopsy.
How is Membranoproliferative Glomerulonephritis Treated?
Membranoproliferative glomerulonephritis is treated by diuretics, steroids, immunosuppressors, dialysis, or kidney transplant.
What is the Prognosis of Membranoproliferative Glomerulonephritis?
The prognosis of membranoproliferative glomerulonephritis is fair though the long-term effect is chronic kidney disease.
What is Membranous Nephropathy?
Membranous nephropathy is a disease of the small blood vessels of the kidney which helps in the filtering of the waste products from the blood.
What is the Pathology of Membranous Nephropathy?
The pathology of membranous nephropathy is the study of the disease that affects the small vessels of the kidney.
-Etiology: The cause of membranous nephropathy is an autoimmune disease, infection, medication e.g. NSAIDS, malignancies e.g. solid cancerous tumor.
-Genes involved: PLA2R1 gene.
-Pathogenesis: The sequence of events that lead to membranous nephropathy is the formation of the immune complexes in the small blood vessels of the kidney in between the podocytes and the glomerular basement membrane that hinders the normal functioning leading to the disease.
-Morphology: The morphology associated with membranous nephropathy shows diffuse thickening of the capillary walls.
-Histology: The histology associated with membranous nephropathy shows hyaline droplets on the proximal convoluted tubules, narrow capillary lumina.
How does Membranous Nephropathy Present?
Patients with membranous nephropathy typically are males present at the age range of more than 50. The symptoms, features, and clinical findings associated with membranous nephropathy include edema, proteinuria, weight gain, fatigue, poor appetite, foamy urine, bloody urine.
How is Membranous Nephropathy Diagnosed?
Membranous nephropathy is diagnosed with routine urine tests, symptoms presenting, blood tests, glomerular filtration rate, antinuclear antibody tests, kidney ultrasound, kidney biopsy.
How is Membranous Nephropathy Treated?
Membranous nephropathy is treated by managing the symptoms as the present, removal of the cause.
What is the Prognosis of Membranous Nephropathy?
The prognosis of membranous nephropathy is good due to full remission after proper management.
What is Minimal Change Disease?
Minimal change disease is a type of disease of the glomeruli that can lead to a nephrotic syndrome characterized by increased loss of protein in urine.
What is the Pathology of Minimal Change Disease?
The pathology of minimal change disease is:
-Etiology: The cause of minimal change disease is allergic reactions, tumors, viral infections, NSAIDs,
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to minimal change in disease is not clearly understood but some factors include autoimmune infections that lead to the damage of the podocytes of the glomerular cells.
-Morphology: Not applicable.
-Histology: The histology associated with minimal change disease shows fused foot process, protein particles.
How does Minimal Change Disease Present?
Patients with minimal change disease typically more in boys than girls in children but in adults, both male and female are affected present at the age range of 2-6 years and 40 years. The symptoms, features, and clinical findings associated with minimal change disease include proteinuria, edema, high cholesterol.
How is Minimal Change Disease Diagnosed?
Minimal change disease is diagnosed by urine tests, blood tests, glomerular filtration rate, kidney biopsy.
How is Minimal Change Disease Treated?
Minimal change disease is treated steroids in children, diuretics, limited sodium use, ACEC inhibitors.
What is the Prognosis of Minimal Change Disease?
The prognosis of minimal change disease is good with a 90% recovery to oral medication.
What are Nephritic Syndromes?
Nephritic syndromes are glomerular syndromes characterized by hematuria, hypertension, reduced urine output, and edema.
Examples of nephritic syndrome include:
- Acute proliferative glomerulonephritis
- Postinfectious glomerulonephritis
- Poststreptococcal glomerulonephritis
- Rapidly progressive glomerulonephritis
- Crescentic glomerulonephritis
What is Acute Proliferative Glomerulonephritis?
Acute proliferative glomerulonephritis is a disease of the glomeruli that is caused by bacterial infection.
What is the Pathology of Acute Proliferative Glomerulonephritis?
The pathology of acute proliferative glomerulonephritis is the scientific study of the disease of the glomeruli caused by bacterial infection, especially the streptococcus type.
-Etiology: The cause of acute proliferative glomerulonephritis is streptococcus bacteria.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to acute proliferative glomerulonephritis, the infection affects the blood vessels leading to inflammation of the glomeruli rendering the renal organ ineffective if the process of urine filtering.
-Morphology: Not applicable.
-Histology: The histology associated with acute proliferative glomerulonephritis shows diffuse, focal and mesangial patterns.
How does Acute Proliferative Glomerulonephritis Present?
Patients with acute proliferative glomerulonephritis typically are males present at the the age range of 5-15 years. The symptoms, features, and clinical findings associated with acute proliferative glomerulonephritis include hematuria, oliguria, edema, hypertension, fever, headache.
How is Acute Proliferative Glomerulonephritis Diagnosed?
Acute proliferative glomerulonephritis is diagnosed with kidney biopsy, blood tests, physical examination.
How is Acute Proliferative Glomerulonephritis Treated?
Acute proliferative glomerulonephritis is treated by blood pressure control, low sodium diet, loop diuretics, beta blockers.
What is the Prognosis of Acute Proliferative Glomerulonephritis?
The prognosis of acute proliferative glomerulonephritis is good since once the symptoms are managed the disease resolves.
What is Postinfectious Glomerulonephritis?
Postinfectious glomerulonephritis is a disease of the glomeruli that results after the effects of an infection.
What is the Pathology of Postinfectious Glomerulonephritis?
The pathology of postinfectious glomerulonephritis is the study of the effects of infection occurring in other parts that affects the glomeruli.
-Etiology: The cause of postinfectious glomerulonephritis is bacterial infection in other body parts.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to postinfectious glomerulonephritis during the disease process, antibodies, antigens and the complement system are responsible to fight infection. In this disease those immune complexes get trapped in the kidney filters hindering them from filtering normally causing glomerulonephritis.
-Morphology: Not applicable.
-Histology: The histology associated with postinfectious glomerulonephritis shows larger glomeruli cells, increased inflammatory cells, hump-like subendothelial immune complex deposits.
How does Postinfectious Glomerulonephritis Present?
Patients with postinfectious glomerulonephritis typically are females present at the the age range of 6-10 years. The symptoms, features, and clinical findings associated with postinfectious glomerulonephritis include generalized edema of all parts of the body including g the face, hypertension, coca-cola coloured urine, oliguria, joint pain and stiffness.
How is Postinfectious Glomerulonephritis Diagnosed?
Postinfectious glomerulonephritis is diagnosed through physical examination, auscultation, blood tests, urinalysis, kidney biopsy.
How is Postinfectious Glomerulonephritis Treated?
Postinfectious glomerulonephritis is treated by mainly managing the symptoms, blood pressure regulation, and salt restriction.
What is the Prognosis of Postinfectious Glomerulonephritis?
The prognosis of postinfectious glomerulonephritis is goodsince it resolves after the infection is treated.
What is Poststreptococcal Glomerulonephritis?
Poststreptococcal glomerulonephritis is the disease of the glomeruli that arises after the infection of the group A streptococcal bacteria.
What is the Pathology of Poststreptococcal Glomerulonephritis?
The pathology of poststreptococcal glomerulonephritis is:
-Etiology: The cause of poststreptococcal glomerulonephritis is group A strep bacteria.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to poststreptococcal glomerulonephritis is once the infection occurs, there is rapid inflammation of the glomeruli and deterioration of this function.
-Morphology: Not applicable.
-Histology: The histology associated with poststreptococcal glomerulonephritis shows increased mesangial cells, increased mesangial matrix, and segmental thickening of the bowman’s capsule.
How does Poststreptococcal Glomerulonephritis Present?
Patients with poststreptococcal glomerulonephritis typically are male present at the the age range of 3-7 years. The symptoms, features, and clinical findings associated with poststreptococcal glomerulonephritis include dark reddish brown urine, edema, oliguria, fatigue, malaise, proteinuria.
How is Poststreptococcal Glomerulonephritis Diagnosed?
Poststreptococcal glomerulonephritis is diagnosed history taking and physical examination, blood tests, urinalysis.
How is Poststreptococcal Glomerulonephritis Treated?
Poststreptococcal glomerulonephritis is treated mainly by management of the symptoms.
What is the Prognosis of Poststreptococcal Glomerulonephritis?
The prognosis of poststreptococcal glomerulonephritis is good with a 90% survival rate.
What is Rapidly Progressive Glomerulonephritis?
Rapidly progressive glomerulonephritis is a disease of the glomeruli characterized by rapid loss of function of the kidney.
What is the Pathology of Rapidly Progressive Glomerulonephritis?
The pathology of rapidly progressive glomerulonephritis is:
-Etiology: The cause of rapidly progressive glomerulonephritis is infections, multisystemic disease, drugs and toxic agents.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to rapidly progressive glomerulonephritis, the antigen formed against the GBM antibodies lead to increased damage to the kidney.
-Morphology: Not applicable.
-Histology: The histology associated with rapidly progressive glomerulonephritis shows crescentic formation, fibrinoid necrosis, focal breakage of the glomerular basement membrane, necrotizing lesions,
How does Rapidly Progressive Glomerulonephritis Present?
Patients with rapidly progressive glomerulonephritis typically both male and female present at the age range of 20-30 years the first peak and 60-70 years the second peak. The symptoms, features, and clinical findings associated with rapidly progressive glomerulonephritis include oliguria, anuria, fever, myalgia, haemoptysis, anemia.
How is Rapidly Progressive Glomerulonephritis Diagnosed?
Rapidly progressive glomerulonephritis is diagnosed with history taking , urinalysis, serologic tests, renal biopsy.
How is Rapidly Progressive Glomerulonephritis Treated?
Rapidly progressive glomerulonephritis is treated with plasmapheresis, corticosteroids, cyclophosphamide.
What is the Prognosis of Rapidly Progressive Glomerulonephritis?
The prognosis of rapidly progressive glomerulonephritis is poor.
What is Crescentic Glomerulonephritis?
Crescentic Glomerulonephritis is a chronic disease of the glomerular that is immune mediated.
What is the Pathology of Crescentic Glomerulonephritis?
The pathology of crescentic glomerulonephritis is the study of the disease of the glomerular leading to inflammation and injury.
-Etiology: The cause of crescentic glomerulonephritis is autoimmune antibodies.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to crescentic glomerulonephritis macrophages involve producing toxins that lead to destruction of the glomerular leading to end stage renal failure.
-Morphology: Not applicable.
-Histology: The histology associated with crescentic glomerulonephritis shows glomerular crescent formation, fibrin deposition.
How does Crescentic Glomerulonephritis Present?
Patients with crescentic glomerulonephritis typically are both male and female present at the age range of 60-85 years. The symptoms, features, and clinical findings associated with crescentic glomerulonephritis include hematuria, proteinuria, imparued GFR.
How is Crescentic Glomerulonephritis Diagnosed?
Crescentic glomerulonephritis is diagnosed history, urinalysis, kidney biopsy.
How is Crescentic Glomerulonephritis Treated?
Crescentic glomerulonephritis is treated with immunosuppressors, corticosteroids, and plasma exchange.
What is the Prognosis of Crescentic Glomerulonephritis?
The prognosis of crescentic glomerulonephritis is fair with partial or total recovery.
What are Isolated Glomerular Abnormalities?
Isolated glomerular abnormalities are diseases of the kidney that occur as a result of genetic factors
Examples of isolated glomerular abnormalities include:
- Hereditary nephritis
- IgA nephropathy (Berger disease)
What is Hereditary Nephritis?
Hereditary Nephritis is also known as Alport syndrome. A group of diseases caused by gene mutation
What is the Pathology of Hereditary Nephritis?
The pathology of hereditary nephritis is:
-Etiology: The cause of hereditary nephritis is genetic factors.
-Genes involved: COL4A1-A6 genes.
-Pathogenesis: The sequence of events that lead to hereditary nephritis is poorly understood but maybe due to the mutation of genes.
-Morphology: Not applicable.
-Histology: The histology associated with hereditary nephritis shows thin GBM with thickening.
How does Hereditary Nephritis Present?
Patients with hereditary nephritis typically are males present at the first years of life. The symptoms, features, and clinical findings associated with hereditary nephritis include hematuria, renal dysfunction, proteinuria, deafness,edema, and vision changes.
How is Hereditary Nephritis Diagnosed?
Hereditary nephritis is diagnosed through history taking, physical examination, urinalysis, renal biopsy, hearing and vision tests, genetic testing.
How is Hereditary Nephritis Treated?
Hereditary nephritis is treated mainly by managing the symptoms, diuretics, limiting sodium intake, and managing high blood pressure.
What is the Prognosis of Hereditary Nephritis?
The prognosis of hereditary nephritis is poor.
What is IgA Nephropathy?
IgA nephropathy is also known as Berger disease. Is a disease of the kidney that arises when there is a deposition of the IgA antibody in great amounts.
What is the Pathology of IgA Nephropathy?
The pathology of IgA nephropathy is:
-Etiology: The cause of IgA nephropathy is genetic predisposition, liver disease, infections, celiac diseases.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to IgA nephropathy is due to the accumulation of immunoglobulin A in the mesangial membranes. The tapped IgA causes inflammation and poor filtration process causing nephropathy.
-Morphology: Not applicable.
-Histology: The histology associated with IgA nephropathy shows branching mesangial deposits, immune deposits.
How does IgA Nephropathy Present?
Patients with IgA nephropathy typically are affected more present at the age range of 12-30 years. The symptoms, features, and clinical findings associated with IgA nephropathy include tea-colored urine, foamy urine, pain at the location of the kidneys, edema, hypertension.
How is IgA Nephropathy Diagnosed?
IgA nephropathy is diagnosed by urine tests, blood tests, kidney biopsy, iothalamate clearance test.
How is IgA Nephropathy Treated?
IgA nephropathy is treated by antihypertensives, omega-3 fatty acids, immunosuppressants, statin therapy, diuretics.
What is the Prognosis of IgA Nephropathy?
The prognosis of IgA nephropathy is fair since 70% of those with this disease have a normal life expectancy.
What is Chronic Glomerulonephritis?
Chronic glomerulonephritis is a disease of the kidney in which the inflammation caused leads to scarring, slow and cumulative damage of the kidney.
What is the Pathology of Chronic Glomerulonephritis?
The pathology of chronic glomerulonephritis is:
-Etiology: The cause of chronic glomerulonephritis is infections bacterial or viral, autoimmune diseases,
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to chronic glomerulonephritis glomerular scarring, leading to cortical tubular atrophy, interstitial fibrosis and infiltration.
-Morphology: Not applicable.
-Histology: The histology of chronic glomerulonephritis shows partial and complete hyalinization of glomeruli. There may also be an inflammatory infiltrate.
How does Chronic Glomerulonephritis Present?
Patients with chronic glomerulonephritis typically bothe male and female but men reach kidney failure faster than male present at age range of 18-65 years. The symptoms, features, and clinical findings associated with chronic glomerulonephritis include blood in urine, confusion, drowsiness, lethargy, foamy urine, loss of sensation in the lower limbs.
How is Chronic Glomerulonephritis Diagnosed?
Chronic glomerulonephritis is diagnosed with complete blood count, kidney biopsy and scan, history taking, physical examination and, urinalysis.
How is Chronic Glomerulonephritis Treated?
Chronic glomerulonephritis is treated by managing the symptoms. Antihypertensives, diuretics, corticosteroids, dietary restrictions, immunosuppressives, dialysis, a kidney transplant.
What is the Prognosis of Chronic Glomerulonephritis?
The prognosis of chronic glomerulonephritis is:
What are Systemic Diseases Associated with Glomerular Lesions?
Systemic diseases associated with glomerular lesions are diseases of the kidney that arise from the injury of the kidney that forms lesions.
Examples of systemic diseases associated with glomerular lesions include:
- Diabetic nephropathy
- Fibrillary glomerulonephritis
- Glomerulonephritis associated with bacterial endocarditis
- Glomerulonephritis associated with systemic infections
- Henoch-Schonlein purpura
- Lupus nephritis
What is Diabetic Nephropathy?
Diabetic nephropathy is a clinical syndrome characterized by reduced GFR, albuminemia, and elevated arterial blood pressure.
What is the Pathology of Diabetic Nephropathy?
The pathology of diabetic nephropathy is:
-Etiology: The cause of diabetic nephropathy is high blood pressure, high blood sugar levels.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to diabetic nephropathy is mostly mediated by the metabolic and hemodynamic changes that occur as a result of diabetes. These changes affect the blood vessels of the kidney affecting normal function.
-Morphology: The morphology associated with diabetic nephropathy shows glomerular lesions, basal membrane thickening, glomerular aneurysm.
-Histology: The histology associated with diabetic nephropathy shows thickening of tubular basement membrane, mesangial expansion.
How does Diabetic Nephropathy Present?
Patients with diabetic nephropathy typically are females present at the age range of 10-60 years. The symptoms, features, and clinical findings associated with diabetic nephropathy include proteinuria, hypertension, decreased glomerular filtration rate, frequent urination, dyspnea, confusion, and edema.
How is Diabetic Nephropathy Diagnosed?
Diabetic nephropathy is diagnosed with urinalysis, urine albumin tests, glomerular filtration rate, imaging tests, and kidney biopsy.
How is Diabetic Nephropathy Treated?
Diabetic nephropathy is treated by either dialysis or kidney transplant.
What is the Prognosis of Diabetic Nephropathy?
The prognosis of diabetic nephropathy is good with a mortality rate of 10%.
What is Fibrillary Glomerulonephritis?
Fibrillary glomerulonephritis is a disease of the glomerulus that is characterized by the deposition of the fibril proteins in the glomerulus.
What is the Pathology of Fibrillary Glomerulonephritis?
The pathology of fibrillary glomerulonephritis is:
-Etiology: The cause of fibrillary glomerulonephritis is malignancies, autoimmune diseases,
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to fibrillary glomerulonephritis
-Morphology: The morphology associated with fibrillary glomerulonephritis shows an accumulation of nonbranching randomly arranged fibrils.
-Histology: The histology associated with fibrillary glomerulonephritis shows mesangial expansion, endocapillary proliferation.
How does Fibrillary Glomerulonephritis Present?
Patients with fibrillary glomerulonephritis typically male present at the age range of 55-60 years. The symptoms, features, and clinical findings associated with fibrillary glomerulonephritis include hematuria, proteinuria, renal insufficiency, and hypertension.
How is Fibrillary Glomerulonephritis Diagnosed?
Fibrillary glomerulonephritis is diagnosed by microscopic examination.
How is Fibrillary Glomerulonephritis Treated?
Fibrillary glomerulonephritis is treated with rituximab.
What is the Prognosis of Fibrillary Glomerulonephritis?
The prognosis of fibrillary glomerulonephritis is poor.
What is Glomerulonephritis Associated with Bacterial Endocarditis?
Glomerulonephritis associated with bacterial endocarditis is glomerulitis that results from bacterial endocarditis.
What is the Pathology of Glomerulonephritis Associated with Bacterial Endocarditis?
The pathology of glomerulonephritis associated with bacterial endocarditis is:
-Etiology: The cause of glomerulonephritis associated with bacterial endocarditis is bacterial based mainly staphylococcus aureus.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to glomerulonephritis associated with bacterial endocarditis is the presence of immune complexes that are found as a result of bacterial endocarditis.
-Morphology: Not applicable.
-Histology: Lymphocytic infiltrate of glomeruli.
How does Glomerulonephritis Associated with Bacterial Endocarditis Present?
Patients with glomerulonephritis associated with bacterial endocarditis are typically male present at the age range of 30-50 years. The symptoms, features, and clinical findings associated with glomerulonephritis associated with bacterial endocarditis include urinary symptoms.
How is Glomerulonephritis Associated with Bacterial Endocarditis Diagnosed?
Glomerulonephritis associated with bacterial endocarditis is diagnosed in blood tests.
How is Glomerulonephritis Associated with Bacterial Endocarditis Treated?
Glomerulonephritis associated with bacterial endocarditis is treated with a short term low dose of corticosteroids.
What is the Prognosis of Glomerulonephritis Associated with Bacterial Endocarditis?
The prognosis of glomerulonephritis associated with bacterial endocarditis is poor.
What is Glomerulonephritis Associated with Systemic Infections?
Glomerulonephritis associated with systemic infections is the infection manifestation syndrome of the kidney in which an immunologic mechanism initiates inflammation and proliferation of glomerular tissue.
What is the Pathology of Glomerulonephritis Associated with Systemic Infections?
The pathology of glomerulonephritis associated with systemic infections is:
-Etiology: The cause of glomerulonephritis associated with systemic infections is infections.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to glomerulonephritis associated with systemic infections
-Morphology: Not applicable.
-Histology: Lymphocytic infiltrate of glomeruli.
How does Glomerulonephritis Associated with Systemic Infections Present?
Patients with glomerulonephritis associated with systemic infections typically are both female and male present at the age range of 20-60 years. The symptoms, features, and clinical findings associated with glomerulonephritis associated with systemic infections include pink or cola-colored urine, hematuria, foamy urine, and proteinuria.
How is Glomerulonephritis Associated with Systemic Infections Diagnosed?
Glomerulonephritis associated with systemic Infections is diagnosed through blood tests, urinalysis, and kidney biopsy.
How is Glomerulonephritis Associated with Systemic Infections Treated?
Glomerulonephritis associated with systemic infections is treated with immunosuppressors, dialysis.
What is the Prognosis of Glomerulonephritis Associated with Systemic Infections?
The prognosis of glomerulonephritis associated with systemic infections is fair since once the infections are managed it can be resolved.
What is Henoch-Schonlein Purpura?
Henoch-Schonlein purpura is an acute immunoglobulin A mediated disorder that is characterized by inflammation of the small blood vessels of the kidney.
What is the Pathology of Henoch-Schonlein Purpura?
The pathology of Henoch-schonlein purpura is:
-Etiology: The cause of Henoch-schonlein purpura is Ig A.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to Henoch-Schonlein purpura occurs when the underlying infections cause production of the IgA immune complexes that become deposited in the walls of the kidney and the mesangium. These accumulation causes inflammation hence causing glomerulonephritis.
-Morphology: Not applicable.
-Histology: The histology associated with Henoch-Schonlein purpura shows mesangial proliferation, small crescents, infiltration of neutrophils.
How does Henoch-Schonlein Purpura Present?
Patients with Henoch-Schonlein purpura typically both male and female present at the age range of 6 years. The symptoms, features, and clinical findings associated with henoch-schonlein purpura include palpable purpura, arthralgia, abdominal pain, renal disease, headache, anorexia, fever.
How is Henoch-Schonlein Purpura Diagnosed?
Henoch-Schonlein purpura is diagnosed by physical examination, history taking, blood tests, urinalysis, ultrasound and biopsy.
How is Henoch-Schonlein Purpura Treated?
Henoch-Schonlein purpura is treated with supportive care, good hydration, pain medication, glucocorticoids, immunosuppressors.
What is the Prognosis of Henoch-Schonlein Purpura?
The prognosis of Henoch-Schonlein purpura is good since it resolves completely.
What is Lupus Nephritis?
Lupus nephritis is an autoimmune disease that affects the kidney.
What is the Pathology of Lupus Nephritis?
The pathology of lupus nephritis is:
-Etiology: The cause of lupus nephritis is genetic factors, immunologic factors, environmental factors.
-Genes involved: MBL2, TNF, CTLA4 genes.
-Pathogenesis: The sequence of events that lead to lupus nephritis is due to the autoimmune e disease that leads to the formation of antibodies and immune complexes which leads to renal damage and finally nephritis.
-Morphology: The morphology associated with lupus nephritis shows thickening of capillary walls.
-Histology: The histology associated with lupus nephritis shows mesangial or capillary immune deposits, increased mesangial cellularity, thickening of capillary walls,
How does Lupus Nephritis Present?
Patients with lupus nephritis typically are female present at the age range of 20-40 years. The symptoms, features, and clinical findings associated with lupus nephritis are at first asymptomatic later fatigue, malar rash, discoid lupus, oral ulcers,photosensitivity hypoalbuminemia, joint pain, hematuria, proteinuria, serositis.
How is Lupus Nephritis Diagnosed?
Lupus nephritis is diagnosed through blood tests, urinalysis, ultrasound of the kidney, kidney biopsy, X-ray.
How is Lupus Nephritis Treated?
Lupus nephritis is treated with corticosteroids, cytotoxic agents, plasma exchange, rituximab.
What is the Prognosis of Lupus Nephritis?
The prognosis of lupus nephritis is fair with a survival rate of 73%.
What are Tubular and Interstitial Diseases?
Tubular and interstitial diseases are the disease of the kidney that mostly affects the renal tubules and the renal interstitium respectively.
Examples of tubular and interstitial diseases include:
- Acute drug-induced interstitial nephritis
- Bile cast nephropathy
- Hypercalcemia induced tubulointerstitial disease
- Light chain cast nephropathy
- Nephrocalcinosis
- Urate nephropathy
What is Acute Drug-Induced Interstitial Nephritis?
Acute drug-induced Interstitial nephritis is a disease of the interstitium that occurs due to the hypersensitivity reaction towards a certain drug.
What is the Pathology of Acute Drug-Induced Interstitial Nephritis?
The pathology of acute drug-induced interstitial nephritis is:
-Etiology: The cause of acute drug-induced interstitial nephritis is hypersensitivity to drugs,
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to acute drug-induced interstitial nephritis toxicity from the ingested drugs causes a hypersensitive reaction to the nephrons of the kidneys leading to nephritis.
-Morphology: Unknown.
-Histology: Interstitial inflammatory infiltrate.
How does Acute Drug-Induced Interstitial Nephritis Present?
Patients with acute drug-induced interstitial nephritis typically present at the age range of 40-80 years. The symptoms, features, and clinical findings associated with acute drug-induced interstitial nephritis include rash fever, eosinophilia after 7 days of consumption of the medicine.
How is Acute Drug-Induced Interstitial Nephritis Diagnosed?
Acute drug-induced interstitial nephritis is diagnosed kidney biopsy, physical examination and history taking.
How is Acute Drug-Induced Interstitial Nephritis Treated?
Acute drug-induced interstitial nephritis is treated by mainly withdrawing the suspected medication, corticosteroids.
What is the Prognosis of Acute Drug-Induced Interstitial Nephritis?
The prognosis of acute drug-induced interstitial nephritis is fair if the medication is withdrawn.
What is Bile Cast Nephropathy?
Bile cast Nephropathy also known as cholemic nephropathy, is an acute kidney injury that may be caused by increased bilirubin or bile acids levels.
What is the Pathology of Bile Cast Nephropathy?
The pathology of bile cast nephropathy is:
-Etiology: The cause of bile cast nephropathy is not well understood but some factors are obstruction of the kidney tubules, toxicity from bile acids, and systemic hypoperfusion.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to bile cast nephropathy is when there are increased amounts of bilirubin in the kidney that cause damage to the tubules leading to nephropathy.
-Morphology: The morphology associated with bile cast nephropathy shows bilirubin casts deposition in the distal, nephron,
-Histology: The histology associated with bile cast nephropathy shows yellow cortex, bilirubin casts deposition.
How does Bile Cast Nephropathy Present?
Patients with bile cast nephropathy typically are male present at the age range of 30-80 years. The symptoms, features, and clinical findings associated with bile cast nephropathy include acute jaundice, renal insufficiency.
How is Bile Cast Nephropathy Diagnosed?
Bile cast nephropathy is diagnosed by physical and history taking, kidney biopsy, blood tests, bilirubin levels.
Bile cast nephropathy is a treatment for reduction in the levels of bilirubin and bile salts, renal replacement therapy.
How is Bile Cast Nephropathy Treated?
Bile cast nephropathy is treated symptomatically.
What is the Prognosis of Bile Cast Nephropathy?
The prognosis of bile cast nephropathy is fair if diagnosed early and appropriate management adhered to.
What is Hypercalcemia?
Hypercalcemia induced tubulointerstitial disease is the disease of the interstitium that is caused by increased levels of calcium in the body.
What is the Pathology of Hypercalcemia Induced Tubulointerstitial Disease
The pathology of hypercalcemia induced tubulointerstitial disease is:
-Etiology: The cause of hypercalcemia induced tubulointerstitial disease is increased calcium levels,
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to hypercalcemia induced tubulointerstitial disease is that too much calcium in the kidneys cause damage to the tubulointerstitial layers leading to nephropathy.
-Morphology: Not applicable.
-Histology: The histology associated with hypercalcemia induced tubulointerstitial disease shows eosinophilic cellular infiltration, fibrosis and atrophy.inflammatory infiltrate with no glomerular changes.
How does Hypercalcemia Induced Tubulointerstitial Disease Present?
Patients with hypercalcemia induced tubulointerstitial disease typically are female and the age range is not clearly stated. The symptoms, features, and clinical findings associated with hypercalcemia induced tubulointerstitial disease include polyuria, dehydration, renal stones, hematuria,
How is Hypercalcemia Induced Tubulointerstitial Disease Diagnosed?
Hypercalcemia induced tubulointerstitial disease is diagnosed with renal biopsy, urinalysis, blood count, radiography and ultrasonography, CT scan.
How is Hypercalcemia Induced Tubulointerstitial Disease Treated?
Hypercalcemia induced tubulointerstitial disease is treated with dialysis, transplantation.
What is the Prognosis of Hypercalcemia Induced Tubulointerstitial Disease?
The prognosis of hypercalcemia induced tubulointerstitial disease is fair but it will mostly depend on the management of the symptoms but the chances of it causing end stage renal failure is high.
What is Light Chain Cast Nephropathy?
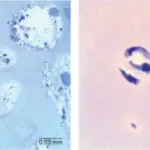
Light chain cast nephropathy is a disease of the kidney that is mainly caused by multiple myeloma hence the name myeloma kidney that can present with amyloid cast or the crystal casts.
What is the Pathology of Light Chain Cast Nephropathy?
The pathology of light chain cast nephropathy is:
-Etiology: The cause of light chain cast nephropathy is underlying multiple myeloma, decreased urine flow rate, protein complexes formation.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to light chain cast nephropathy are precipitated by the presence of multiple myeloma in the patient, this disease causes production of the proteinaceous casts in the kidney tubules and the collecting ducts hence causing nephropathy.
-Morphology: The morphology associated with light chain cast nephropathy shows fractured casts in the lumen of the distal tubule.
-Histology: The histology associated with light chain cast nephropathy shows irregular or rectangular light chain casts, plasma cells in the bone marrow evidence of myeloma, eosinophilic, dense, homogenous casts.
How does Light Chain Cast Nephropathy Present?
Patients with light chain cast nephropathy typically are female present at the age range of 58 years. The symptoms, features, and clinical findings associated with light chain cast nephropathy include weight loss, constipation, anemia, fatigue,
How is Light Chain Cast Nephropathy Diagnosed?
Light chain cast nephropathy is diagnosed in blood samples for elevated serum levels, kidney biopsy, urinalysis, myelogram, peripheral smear, complete blood count and serum calcium.
How is Light Chain Cast Nephropathy Treated?
Light chain cast nephropathy is treated by lowering the light chains and chemotherapy agents but this process is still new, plasmapheresis,
What is the Prognosis of Light Chain Cast Nephropathy?
The prognosis of light chain cast nephropathy is poor since its association with multiple myeloma leads to reduced survival chances.
What is Nephrocalcinosis?
Nephrocalcinosis is kidney syndrome in which the calcium levels are increased, inducing the formation and deposition of calcium stones in the kidney.
What is the Pathology of Nephrocalcinosis?
The pathology of nephrocalcinosis is:
-Etiology: The cause of nephrocalcinosis is conditions with cortical calcium deposition. Tuberculosis, pyelonephritis, glomerulonephritis, acute transplant rejection etc. Condition with medullary calcium deposition such as hyperparathyroidism and ADCK4 mutations.
-Genes involved: ADCK4 mutations.
-Pathogenesis: The sequence of events that lead to nephrocalcinosis is due to conditions characterized by hypercalcemia, damage at intracellular level, inducing the establishment of calcium stones and deposition of calcium in the kidney. Calcified cellular debris contributes to impediment of tubular lumens, obstructive atrophy to the nephrons with interstitial fibrosis and nonspecific lingering inflammation.
-Morphology: The morphology associated with nephrocalcinosis shows atrophy of entire cortical
-Histology: The histology associated with nephrocalcinosis shows interstitium crystal deposition,
How does Nephrocalcinosis Present?
Patients with nephrocalcinosis typically no gender preference is reported present at age range of any age. The symptoms, features, and clinical findings associated with nephrocalcinosis include asymptomatic, polyuria polydipsia, hypertension, proteinuria, pyuria, kidney failure, and bone deformity.
How is Nephrocalcinosis Diagnosed?
Nephrocalcinosis is diagnosed by laboratory works- serum calcium, phosphate, albumin, potassium, creatine. BUN, urinalysis and urine culture. Radiological studies such as CT scan, and ultrasonography.
How is Nephrocalcinosis Treated?
Nephrocalcinosis is treated by pharmacologic therapy- thiazide diuretics, calcium metabolism modifiers, vitamins, antimalarial agent, and calcimimetic agent. Surgical therapy in case of urinary stones.
What is the Prognosis of Nephrocalcinosis?
The prognosis of nephrocalcinosis is fair. The morbidity and mortality allied with nephrocalcinosis depend on the disease-associated.
What is Urate Nephropathy?
Urate nephropathy is the deterioration of the kidney function due to hyperuricemia disorders.
What is the Pathology of Urate Nephropathy?
The pathology of urate nephropathy is:
-Etiology: The cause of urate nephropathy is hereditary enzyme disorder, HGPRT deficiency, hyperuricemia, leukemia treatment, and conditions such as gout.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to urate nephropathy follows the uric acid deposition in the kidney.
-Morphology: Not applicable.
-Histology: Stone or nidus formation.
How does Urate Nephropathy Present?
Patients with urate nephropathy typically slightly high in males present at age range of any age. The symptoms, features, and clinical findings associated with urate nephropathy include gout, ureteral obstruction, and oliguria.
How is Urate Nephropathy Diagnosed?
Urate nephropathy is diagnosed through laboratory study- urate levels in the plasma> 15 mg/dL indicate hyperuricemia, urinalysis and elevate serum uric acid.
How is Urate Nephropathy Treated?
Urate nephropathy is treated by medical therapy- allopurinol. Surgical care in case of uric acid stones.
What is the Prognosis of Urate Nephropathy?
The prognosis of urate nephropathy is fair depending on the underlying cause.
What are Vascular Diseases of the Kidney?
Vascular diseases of the kidney are the condition affecting the blood vessel supplying the kidneys.
Examples of vascular diseases of the kidney include:
- Malignant nephrosclerosis
- Nephrosclerosis
- Renal artery stenosis
- Thrombotic microangiopathies involving the kidney
- Atheroembolic renal disease
- Atherosclerotic ischemic renal disease
- Diffuse cortical necrosis
- Renal infarcts
- Sickle cell nephropathy
What is Malignant Nephrosclerosis?
Malignant nephrosclerosis is a renal disease linked with the malignant and/or enhanced phase of hypertension.
What is the Pathology of Malignant Nephrosclerosis?
The pathology of malignant nephrosclerosis is:
-Etiology: The cause of malignant nephrosclerosis is idiopathic, long-standing hypertension.
-Genes involved: APOL1 gene.
-Pathogenesis: The sequence of events that lead to malignant nephrosclerosis unclear, kidney vascular damage from chronic benign hypertension, vascular fibrinoid necrosis, and mitogenic factor from platelets and plasma, result in hyperplastic arteriolosclerosis, a typical of malignant hypertension.
-Morphology: The morphology associated with malignant nephrosclerosis shows small, pinpoint petechial hemorrhages on the cortical surface.
-Histology: The histology associated with malignant nephrosclerosis shows fibrinoid necrosis of arterioles and interlobular arteries intimal thickening.
How does Malignant Nephrosclerosis Present?
Patients with malignant nephrosclerosis typically slightly high in females present at the age range of 45-65 years. The symptoms, features, and clinical findings associated with malignant nephrosclerosis include headaches, nausea, vomiting, hypertension, hypertensive retinal changes, proteinuria less than 0.5 g/d, encephalopathy, cardiovascular abnormalities, and renal failure.
How is Malignant Nephrosclerosis Diagnosed?
Malignant nephrosclerosis is diagnosed through clinical presentation, lab works- Urinary albumin-to-creatinine ratio, serum potassium, calcium, blood glucose, lipid panel, urinalysis. Imaging studies such as echocardiogram assess left ventricular size, ultrasonography, electrocardiogram (ECG).
How is Malignant Nephrosclerosis Treated?
Malignant nephrosclerosis is treated through managing hypertension with antihypertensive.
What is the Prognosis of Malignant Nephrosclerosis?
The prognosis of malignant nephrosclerosis is good. About 75% of patients will survive 5 years.
What is Nephrosclerosis?
Nephrosclerosis is a clinical syndrome categorized by long-term vital hypertension.
What is the Pathology of Nephrosclerosis?
The pathology of nephrosclerosis is:
-Etiology: The cause of nephrosclerosis is hypertensive condition.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to nephrosclerosis is unclear.
-Morphology: Not applicable.
-Histology: The histology associated with nephrosclerosis shows wrinkling glomerular basement membranes and shrunken glomerular tufts.
How does Nephrosclerosis Present?
Patients with nephrosclerosis typically higher in females present at the age range of 45-65 years. The symptoms, features, and clinical findings associated with nephrosclerosis include, hypertensive retinal changes, proteinuria less than 0.5 g/d, encephalopathy, cardiovascular abnormalities, and renal failure.
How is Nephrosclerosis Diagnosed?
Nephrosclerosis is diagnosed through clinical presentation, lab works- Urinary albumin-to-creatinine ratio, serum potassium, calcium, blood glucose, lipid panel, urinalysis. Imaging studies such as echocardiogram assess left ventricular size, ultrasonography, electrocardiogram (ECG).
How is Nephrosclerosis Treated?
Nephrosclerosis is treated through management of hypertension.
What is the Prognosis of Nephrosclerosis?
The prognosis of nephrosclerosis is good with proper management of hypertension.
What is Renal Artery Stenosis?
Renal artery stenosis is the narrowing of one or more of the renal arteries, main cause of renovascular hypertension and chronic kidney insufficiency.
What is the Pathology of Renal Artery Stenosis?
The pathology of renal artery stenosis is:
-Etiology: The cause of renal artery stenosis is hypertension, atherosclerosis in old age, extrarenal atherosclerosis, diabetes mellitus, smoking, and kidney insufficiency.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to renal artery stenosis follows formation of atherosclerosis lesions, narrowing the renal arterial lumen.
-Morphology: The morphology associated with renal artery stenosis shows a small ischemic kidney.
-Histology: The histology associated with renal artery stenosis shows atheromatous plaque presence, fibromuscular dysplasia.
How does Renal Artery Stenosis Present?
Patients with renal artery stenosis typically higher in females present at the age range of 65-74 years. The symptoms, features, and clinical findings associated with renal artery stenosis include abdominal bruit, hypertension, sudden kidney function worsening, azotemia.
How is Renal Artery Stenosis Diagnosed?
Renal artery stenosis is diagnosed by laboratory studies such as kidney function test, elevated plasma or renal vein renin, urinalysis. Imaging studies such as ultrasonography, radionuclide scanning, spiral CT angiography, MRI and conventional arteriography.
How is Renal Artery Stenosis Treated?
Renal artery stenosis is treated by medical care- ACE inhibitors, surgical care and revascularization.
What is the Prognosis of Renal Artery Stenosis?
The prognosis of renal artery stenosis is fair. Consequences of renal artery stenosis are hypertension.
What are Thrombotic Microangiopathies Involving the Kidney?
Thrombotic microangiopathies involving the kidney is the thrombosis in renal capillaries and arterioles
What is the Pathology of Thrombotic Microangiopathies Involving the Kidney?
The pathology of thrombotic microangiopathies involving the kidney is:
-Etiology: The cause of thrombotic microangiopathies involving the kidney is conditions such as hemolytic uremic syndrome, disseminated intravascular coagulation, and malignant hypertension.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to thrombotic microangiopathies involving the kidney follows endothelial injury and activation and platelet aggregation causing vascular obstruction and vasoconstriction leading to ischemia.
-Morphology: The morphology associated with thrombotic microangiopathies involving the kidney shows patchy or diffuse renal cortical necrosis.
-Histology: The histology associated with thrombotic microangiopathies involving the kidney shows glomeruli thickening and splitting of capillary walls.
How do Thrombotic Microangiopathies Involve the Kidney Present?
Patients with thrombotic microangiopathies involving the kidney typically have no gender preference reported present at the age range of old age. The symptoms, features, and clinical findings associated with thrombotic microangiopathies involving the kidney include blood stain urine, UTI, high blood pressure, decreased urine, and fever.
How are Thrombotic Microangiopathies Involving the Kidney Diagnosed?
Thrombotic microangiopathies involving the kidney are diagnosed through laboratory studies such as kidney function test, urinalysis. Imaging studies such as ultrasonography, radionuclide scanning, spiral CT angiography.
How are Thrombotic Microangiopathies Involving the Kidney Treated?
Thrombotic microangiopathies involving the kidney are treated by symptomatic management, and managing the underlying cause.
What is the Prognosis of Thrombotic Microangiopathies Involving the Kidney?
The prognosis of thrombotic microangiopathies involving the kidney is good. With proper management, the patient recovers in weeks.
What is Atheroembolic Renal Disease?
Atheroembolic renal disease is a renal condition that occurs after a piece of plaque from the large arteries breaks off, travels, and blocking small arteries such as the renal arteries
What is the Pathology of Atheroembolic Renal Disease?
The pathology of atheroembolic renal disease is:
-Etiology: The cause of atheroembolic renal disease is atherosclerotic vascular disease
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to atheroembolic renal disease result after a piece of plaque from the large arteries breaks off, travels, and blocks small arteries such as the renal arteries. Emboli typically lodge in the arcuate and interlobar arteries.
-Morphology: The morphology associated with atheroembolic renal disease shows obliteration of blood vessels.
-Histology: The histology associated with atheroembolic renal disease shows lengthened biconvex transparent needle-shaped clefts.
How does Atheroembolic Renal Disease Present?
Patients with atheroembolic renal disease typically common in males present at the age range of old age. The symptoms, features, and clinical findings associated with atheroembolic renal disease include proteinuria, hematuria, accelerated hypertension, and acute renal failure.
How is Atheroembolic Renal Disease Diagnosed?
Atheroembolic renal disease is diagnosed through imaging- duplex doppler ultrasound, CT angiogram, MRI, catheter angiogram of the kidney.
How is Atheroembolic Renal Disease Treated?
Atheroembolic renal disease is treated by symptomatic and supportive management and dialysis.
What is the Prognosis of Atheroembolic Renal Disease?
The prognosis of atheroembolic renal disease is poorly linked with permanent organ damage.
What is Atherosclerotic Ischemic Renal Disease?
Atherosclerotic ischemic renal disease is a renal inadequacy associated with main renal artery stenosis and/or occlusion.
What is the Pathology of Atherosclerotic Ischemic Renal Disease?
The pathology of atherosclerotic ischemic renal disease is:
-Etiology: The cause of atherosclerotic ischemic renal disease is renal arterial stenosis
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to atherosclerotic ischemic renal disease follows bilateral renal arterial stenosis.
-Morphology: The morphology associated with atherosclerotic ischemic renal disease shows necrotized renal tissue.
-Histology: Thickened, muscular arteries that may be calcified.
How does Atherosclerotic Ischemic Renal Disease Present?
Patients with atherosclerotic ischemic renal disease typically more common in males present at the age range of old age. The symptoms, features, and clinical findings associated with atherosclerotic ischemic renal disease include hematuria, proteinuria, accelerated hypertension, and renal failure, and end stage renal failure symptoms.
How is Atherosclerotic Ischemic Renal Disease Diagnosed?
Atherosclerotic ischemic renal disease is diagnosed through arteriographic studies.
How is Atherosclerotic Ischemic Renal Disease Treated?
Atherosclerotic ischemic renal disease is treated by medical care such as beta blockers, ARBs, ACE inhibitors. Dialysis, surgical care such as revascularization, and transplant.
What is the Prognosis of Atherosclerotic Ischemic Renal Disease?
The prognosis of atherosclerotic ischemic renal disease is poor, associated with ESRD.
What is Diffuse Cortical Necrosis?
Diffuse cortical necrosis is an infrequent patchy necrosis of the renal cortex condition occurring most often after an obstetric emergency.
What is the Pathology of Diffuse Cortical Necrosis?
The pathology of diffuse cortical necrosis is:
-Etiology: The cause of diffuse cortical necrosis is obstetric emergency
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to diffuse cortical necrosis follows obstetric emergencies resulting in cortical destruction, with features of necrosis. arteriolar and glomerular microthrombi contribute to the necrosis and renal damage.
-Morphology: The morphology associated with diffuse cortical necrosis shows cortex necrosis, glomeruli, hemorrhage.
-Histology: The histology associated with diffuse cortical necrosis shows fibrin lumps in the glomerular capillaries.
How does Diffuse Cortical Necrosis Present?
Patients with diffuse cortical necrosis are typically more common in females present at the age range of childbearing age. The symptoms, features, and clinical findings associated with diffuse cortical necrosis include oliguria, hematuria, costovertebral tenderness, flank pain, palpable, and tender kidneys.
How is Diffuse Cortical Necrosis Diagnosed?
Diffuse cortical necrosis is diagnosed by laboratory studies such as complete blood count (CBC), serum electrolytes, coagulation studies, and urinalysis. Imaging studies such as Radiography, ultrasonography and renal scanning, and kidney biopsy.
How is Diffuse Cortical Necrosis Treated?
Diffuse cortical necrosis is treated by medical care intensive care- IV crystalloids, colloids, blood products, and dialysis. Dietary measures such as low-potassium, low-phosphorus.
What is the Prognosis of Diffuse Cortical Necrosis?
The prognosis of diffuse cortical necrosis is poor when bilateral and symmetric, fair when patchy cortical necrosis which may permit survival.
What are Renal Infarcts?
Renal infarcts are kidney syndrome resulting from disruption of the typical blood supply to a portion of, or to the entire kidney.
What is the Pathology of Renal Infarcts?
The pathology of renal infarcts is:
-Etiology: The cause of renal infarctions is embolism, aortic dissection, renal artery dissection, malignant hypertension, and renal vein occlusion.
-Pathogenesis: The sequence of events that lead to renal infarcts is unclear, following the event of embolism.
-Genes involved: Unknown.
-Morphology: The morphology associated with renal infarcts show solitary, multiple pales, yellow-white infarcts lesions, small irregular foci of hemorrhagic discoloration.
-Histology: The histology associated with renal infarcts shows fibrous scarring.
How does Renal Infarcts Present?
Patients with renal infarcts are typically more common in females present at the age range of 45 to 65 years. The symptoms, features, and clinical findings associated with renal infarcts include asymptomatic, acute flank pain, tenderness to the costovertebral angle, and hypertension.
How are Renal Infarcts Diagnosed?
Renal infarcts are diagnosed by radiological studies such as CT angiogram visualizes occluded vessels. Ultrasound shows wedge-shaped regions of nonperfusion.
How are Renal Infarcts Treated?
Renal infarcts are treated by supportive management, and revascularization of the kidney.
What is the Prognosis of Renal Infarcts?
The prognosis of renal infarcts is fair with prompt diagnosis and management.
What is Sickle Cell Nephropathy?
Sickle cell nephropathy is the kidney manifestation of the complication of sickle cell disease.
What is the Pathology of Sickle Cell Nephropathy?
The pathology of sickle cell nephropathy is:
-Etiology: The cause of Sickle cell nephropathy is occluded vessels (vasa recta) in sickle cell disease.
-Genes involved: SCD.
-Pathogenesis: The sequence of events that lead to sickle cell nephropathy results from occluded vessels due to sickle red blood cells.
-Morphology: The morphology associated with sickle cell nephropathy shows glomerular hypertrophy, papillary necrosis.
-Histology: The histology associated with sickle cell nephropathy shows abundant hemosiderin granules in proximal tubular epithelial cells.
How does Sickle Cell Nephropathy Present?
Patients with sickle cell nephropathy typically have more females present at the age range of any age. The symptoms, features, and clinical findings associated with Sickle cell nephropathy include proteinuria, painful gross hematuria, glomerular hyperfiltration, abdominal pain, nausea, vomiting, and fevers.
How is Sickle Cell Nephropathy Diagnosed?
Sickle cell nephropathy is diagnosed by clinical presentation, laboratory works including CBC count, urinalysis, basic metabolic panel. Imaging studies such as renal ultrasound, CT scan, and renal biopsy.
How is Sickle Cell Nephropathy Treated?
Sickle cell nephropathy is treated symptomatic medical management and surgical care kidney transplant.
What is the Prognosis of Sickle Cell Nephropathy?
The prognosis of sickle cell nephropathy is good, with proper management of the underlying cause.
What is Urinary Tract Obstruction?
Urinary tract obstruction is the impediment of the normal urine flow predisposing to infection and to stone formation. Urinary tract obstruction may be due to urolithiasis.
What is Urolithiasis?
Urolithiasis is the formation of the renal calculi, kidney stones in the kidney but may also arise at any level of the urinary collecting system.
What is the Pathology of Urolithiasis?
The pathology of urolithiasis is:
-Etiology: The cause of urolithiasis is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to urolithiasis is obscure. The probable involvement are the predisposing conditions, including the concentration of the solute, variations in urine pH, and bacterial infections.
-Morphology: The morphology associated with urolithiasis shows small and smooth or jagged stone, and staghorn calculi.
-Histology: Not applicable.
How does Urolithiasis Present?
Patients with urolithiasis are typically common in males present at the age range of 70 years. The symptoms, features, and clinical findings associated with urolithiasis include asymptomatic, ureteral colic, urine obstruction, hematuria, and UTI.
How is Urolithiasis Diagnosed?
Urolithiasis is diagnosed radiologically.
How is Urolithiasis Treated?
Urolithiasis is treated by medical care such as alkalinizing agents and diuretics. Surgical interventions, and dietary measures.
What is the Prognosis of Urolithiasis?
The prognosis of urolithiasis is good, with prompt diagnosis and treatment.
What are Neoplasms of the Kidney?
Neoplasms of the kidney are benign or malignant growth affecting the structure and functionality of the renal system.
Examples of neoplasms of the kidney include:
- Benign kidney neoplasms
- Malignant kidney neoplasms
What are Benign Kidney Neoplasms?
Benign kidney neoplasms are renal tumor lesions that are primarily located in the kidney without the capability to invade other sites of the body.
Examples of benign kidney neoplasms include:
- Angiomyolipoma
- Oncocytoma
- Renal papillary adenoma
What is Angiomyolipoma?
Angiomyolipoma is a benign renal neoplasm consisting of fat, vascular components, and smooth muscle.
What is the Pathology of Angiomyolipoma?
The pathology of angiomyolipoma is:
-Etiology: The cause of tuberous sclerosis is unknown.
-Genes involved: TSC2.
-Pathogenesis: The sequence of events that lead to angiomyolipoma unclear
-Morphology: Not applicable.
-Histology: Vascular, muscle, and fat cells in the kidney.
How does Angiomyolipoma Present?
Patients with angiomyolipoma typically have higher preference in females present at the age range of 40 to 60 years. The symptoms, features, and clinical findings associated with angiomyolipoma include palpable abdominal mass, flank pain, hematuria, shock, and acute abdomen.
How is Angiomyolipoma Diagnosed?
Angiomyolipoma is diagnosed by clinical presentation. Imaging studies such as ultrasound shows a hyperechoic lesion, CT scan, and MRI, and percutaneous biopsy.
How is Angiomyolipoma Treated?
Angiomyolipoma is treated by selective renal artery embolization, complete nephrectomy, nephron-sparing surgery, cryo- and radiofrequency ablation, and management with mTOR inhibitors.
What is the Prognosis of Angiomyolipoma?
The prognosis of angiomyolipoma is good, with prompt management.
What is Oncocytoma?
Oncocytoma is rare benign tumors made up of oncocytes, epithelial cells and characterized by the lacking complex I enzyme activity of the oxidative phosphorylation system instigated by mitochondrial DNA (mtDNA) mutations.
What is the Pathology of Oncocytoma?
The pathology of oncocytoma is:
-Etiology: The cause of oncocytoma is genetic changes.
-Genes CCND1.
-Pathogenesis: The sequence of events that lead to oncocytoma is unclear.
-Morphology: The morphology associated with oncocytoma shows tan color tumor.
-Histology: The histology associated with oncocytoma shows a plethora of mitochondria, finely granular eosinophilic cytoplasm.
How does Oncocytoma Present?
Patients with oncocytoma are typically more common in males present at the age range of 60 years. The symptoms, features, and clinical findings associated with oncocytoma include hematuria, flank pain, and a palpable mass.
How is Oncocytoma Diagnosed?
Oncocytoma is diagnosed by radiological imaging studies, and renal biopsy.
How is Oncocytoma Treated?
Oncocytoma is treated conservatively with partial nephrectomy.
What is the Prognosis of Oncocytoma?
The prognosis of oncocytoma is good. The condition rarely metastasizes.
What is Renal Papillary Adenoma?
Renal papillary adenoma is benign renal tumors rising from the renal tubular epithelium usually situated within the cortex.
What is the Pathology of Renal Papillary Adenoma?
The pathology of renal papillary adenoma is:
-Etiology: The cause of renal papillary adenoma is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to renal papillary adenoma unknown.
-Morphology: The morphology associated with renal papillary adenoma shows small, pale yellow-gray, discrete, well-circumscribed nodules.
-Histology: The histology associated with renal papillary adenoma shows complex, branching, papillomatous structure. Cuboidal to polygonal shaped cells with regular, small central nuclei, scanty cytoplasm, and no atypia may be seen.
How does Renal Papillary Adenoma Present?
Patients with renal papillary adenoma typically have no gender preference present at the age range of 70 years. The symptoms, features, and clinical findings associated with renal papillary adenoma include, most are asymptomatic.
How is Renal Papillary Adenoma Diagnosed?
Renal papillary adenoma is diagnosed through kidney biopsy and CT scan imaging.
How is Renal Papillary Adenoma Treated?
Renal papillary adenoma is treated through observation and cryoablation.
What is the Prognosis of Renal Papillary Adenoma?
The prognosis of renal papillary adenoma is good. Have no metastatic potential.
What are Malignant Kidney Neoplasms?
Malignant kidney neoplasms are renal tumors that are aggressive and have the capability to metastasize.
Examples of malignant kidney neoplasms include:
- Renal cell carcinoma
- Urothelial carcinoma of the renal pelvis
What is Renal Cell Carcinoma?
Renal cell carcinoma is a carcinoma derivative of the renal tubular epithelium located predominantly in the cortex and has the capability to invade the surrounding structures.
What is the Pathology of Renal Cell Carcinoma?
The pathology of renal cell carcinoma is:
-Etiology: The cause of renal cell carcinoma is sporadic and genetic factors.
-Genes involved: MET gene.
-Pathogenesis: The sequence of events that lead to renal cell carcinoma is multifactorial.
-Morphology: The morphology associated with renal cell carcinoma shows varying size, bright yellow-gray-white tissue spherical masses.
-Histology: The histology associated with renal cell carcinoma shows clear or granular cytoplasm.
How does Renal Cell Carcinoma Present?
Patients with renal cell carcinoma typically have a male preponderance ratio of 2 to 3. The symptoms, features, and clinical findings associated with renal cell carcinoma include costovertebral pain, palpable mass, fever, malaise, weakness, weight loss and hematuria.
How is Renal Cell Carcinoma Diagnosed?
Renal cell carcinoma is diagnosed through the classical features; costovertebral pain, palpable mass, and hematuria. Imaging- CT of the abdomen, preferably with pelvic CT, MRI, ultrasonography, renal arteriography, and venography.
How is Renal Cell Carcinoma Treated?
Renal cell carcinoma is treated by surgery, thermal ablation, active surveillance, radiation therapy, immunotherapy, and molecular-targeted therapy.
What is the Prognosis of Renal Cell Carcinoma?
The prognosis of renal cell carcinoma is fair with a 5-year survival rate of about 45%.
What is Urothelial Carcinoma of the Renal Pelvis?
Urothelial carcinoma of the renal pelvis is a tumor originating from the urothelium of the renal pelvis, ranging from benign papillomas to invasive urothelial carcinomas.
What is the Pathology of Urothelial Carcinoma of the Renal Pelvis?
The pathology of urothelial carcinoma of the renal pelvis is:
-Etiology: The cause of urothelial carcinoma of the renal pelvis is environmental factors, tobacco smoking, chronic infections and heredity.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to urothelial carcinoma of the renal pelvis result from multifactorial processes.
-Morphology: The morphology associated with urothelial carcinoma of the renal pelvis shows nodular irregular growth.
-Histology: Malignant urothelial cells.
How does Urothelial Carcinoma of the Renal Pelvis Present?
Patients with urothelial carcinoma of the renal pelvis typically have a male-to-female ratio of 3:1. present at the age range of 70 to 80 years. The symptoms, features, and clinical findings associated with urothelial carcinoma of the renal pelvis include hematuria, flank pain dysuria, irritative voiding, weight loss, anorexia, and flank mass.
How is Urothelial Carcinoma of the Renal Pelvis Diagnosed?
Urothelial carcinoma of the renal pelvis is diagnosed through laboratory studies such as urinalysis, basic metabolic panel, LFTs, and CBC count. Imaging studies such as excretory urography.
How is Urothelial Carcinoma of the Renal Pelvis Treated?
Urothelial carcinoma of the renal pelvis is treated by medical therapy- chemotherapeutic agents, radiation therapy, and surgical therapy- nephroureterectomy.
What is the Prognosis of Urothelial Carcinoma of the Renal Pelvis?
The prognosis of urothelial carcinoma of the renal pelvis is fair. Five-year survival rates vary from 50% to 70%