Liver pathology is the study of liver disease.
What is Liver Failure?
Liver failure is the loss of liver function
Examples of liver failure include:
- Acute liver failure
- Acute on chronic liver failure
- Chronic liver failure is the loss of liver function due to cirrhosis
What is Acute Liver Failure?
Acute liver failure is the loss of liver function in weeks or days.
What is the Pathology of Acute Liver Failure?
The pathology of acute liver failure is:
-Etiology: The cause of acute liver failure may be acetaminophen overdose, nonacetaminophen drug-induced liver injury, and acute hepatotropic viral infection.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to acute liver failure hepatocellular necrosis beginning in the centrical distribution and progressing towards portal tracts.
-Histology: The histology associated with acute liver failure shows panacinar hepatic necrosis with the collapse of the reticulin framework.
How does Acute Liver Failure Present?
Patients with acute liver failure typically affect female present at the age range of 40-55 years-old. The symptoms, features, and clinical findings associated with acute liver failure include jaundice, ascites, malaise, nausea, vomiting, and pain in the upper right abdomen.
How is Acute Liver Failure Diagnosed?
Acute liver failure is diagnosed with a biopsy, CT scan, and MRI. Blood reports are also helpful.
How is Acute Liver Failure Treated?
Acute liver failure may be treated by doing a liver transplant or auxiliary partial orthotopic liver transplant.
What is the Prognosis of Acute Liver Failure?
The prognosis of acute liver failure is poor with a mortality of 65% to 85%.
What is Acute on Chronic Liver Failure?
Acute on chronic liver failure is worsening of clinical conditions in patients with cirrhosis or chronic liver disease.
What is the Pathology of Acute on Chronic Liver Failure?
The pathology of acute on chronic liver failure is:
-Etiology: The cause of acute on chronic liver failure is sepsis, active alcoholism, and relapse of chronic viral hepatitis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to acute on chronic liver failure shows intense systemic inflammation sustained by circulating pathogen-associated molecular patterns and damage-associated molecular patterns.
-Histology: The histology associated with acute on chronic liver failure shows microscopic features of cirrhosis.
How does Acute on Chronic Liver Failure Present?
Patients with acute on chronic liver failure typically affects male present at the age range of 40-55 years. The symptoms, features, and clinical findings associated with acute on chronic liver failure include jaundice, malaise, ascites, nausea, vomiting, disorientation, and buildup of the fluid in the abdomen.
How is Acute on Chronic Liver Failure Diagnosed?
Acute on chronic liver failure is diagnosed using blood tests, CT and MRI.
How is Acute on Chronic Liver Failure Treated?
Acute on chronic liver failure is treated with liver transplant and supportive treatment of organ failures.
What is the Prognosis of Acute on Chronic Liver Failure?
The prognosis of acute on chronic liver failure is fair with a life expectancy of 10 years.
What is Chronic Liver Failure?
Chronic liver failure is the loss of liver function due to cirrhosis.
What is the Pathology of Chronic Liver Failure?
The pathology of chronic liver failure is:
-Etiology: The cause of chronic liver failure is cirrhosis hepatitis A, hepatitis B, alcoholic liver disease, and Primary biliary cholangitis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to chronic liver failure includes inflammation (chronic hepatitis), liver cirrhosis, and hepatocellular carcinoma.
-Histology: The histology associated with chronic liver failure shows regenerative nodules of hepatocytes surrounded by fibrous bands without central veins.
How does Chronic Liver Failure Present?
Patients with chronic liver failure typically affect males present at the age range of 35-55 years. The symptoms, features, and clinical findings associated with chronic liver failure include gynecomastia, testicular atrophy, and anaemia.
How is Chronic Liver Failure Diagnosed?
Chronic liver failure is diagnosed using blood tests, ultrasound, and biopsy of the liver.
How is Chronic Liver Failure Treated?
Chronic liver failure is treated with corticosteroids, interferon, antivirals, bile acids, or liver transplant.
What is the Prognosis of Chronic Liver Failure?
The prognosis of chronic liver failure with compensation is good with a survival rate of 15 years.
What is Cirrhosis?
Cirrhosis is a condition where the liver is severely scarred and permanently damaged.
What is the Pathology of Cirrhosis?
The pathology of cirrhosis is:
-Etiology: There are multiple cause of cirrhosis which include chronic alcohol abuse, viral hepatitis, diabetes, obesity, hemochromatosis, nonalcoholic fatty liver disease, and cystic fibrosis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to cirrhosis involves inflammation, hepatic stellate cell activation, angiogenesis, and fibrogenesis.
-Histology: The histology associated with cirrhosis shows vascularized fibrotic septa that link portal tracts with each other and with central veins, leading to hepatocyte islands that are surrounded by fibrotic septa and which are devoid of a central vein.
How does Cirrhosis Present?
Patients with cirrhosis typically affect males present at the age range of 35-55. The symptoms, features, and clinical findings associated with cirrhosis include bruising and bleeding, jaundice, edema, itchy skin, nausea, vomiting, ascites, confusion, difficulty thinking, menopause, and gynecomastia.
How is Cirrhosis Diagnosed?
Cirrhosis is diagnosed by doing a physical examination, blood test, biopsy and CT, MRI.
How is Cirrhosis Treated?
Cirrhosis is treated with Actigall, Urso, and diuretics. Liver transplants may be necessary.
What is the Prognosis of Cirrhosis?
The prognosis of cirrhosis is poor with the risk of mortality up to 70%.
What is Portal Hypertension?
Portal hypertension is elevated pressure in the portal venous system.
What is the Pathology of Portal Hypertension?
The pathology of portal hypertension is:
-Etiology: The cause of portal hypertension is cirrhosis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to portal hypertension includes the formation of an extensive network of portosystemic collaterals that divert a large fraction of portal blood to the systemic circulation, bypassing the liver.
-Histology: The histology associated with portal hypertension shows nodular regenerative hyperplasia and criss-crossing fibrous strands.
How does Portal Hypertension Present?
Patients with portal hypertension typically affect males present at the age range of 35-55 years. The symptoms, features, and clinical findings associated with portal hypertension include encephalopathy, gastrointestinal bleeding, ascites, and decreased platelet count.
How is Portal Hypertension Diagnosed?
Portal hypertension is diagnosed by doing endoscopic examination, X-ray studies, and the laboratory testing.
How is Portal Hypertension Treated?
Portal hypertension is treated with sclerotherapy, beta-blockers, and nitrates.
What is the Prognosis of Portal Hypertension?
The prognosis of portal hypertension is poor with a mortality rate of up to 70%.
What are Infectious Disorders of the Liver?
Infectious disorders of the liver are the disorders caused by microbial pathogens on the liver.
Infectious disorders of the liver include:
- Viral hepatitis
- Bacterial liver infections
- Helminthic liver infections
- Parasitic liver infections
What is Viral Hepatitis?
Viral hepatitis is an infection that causes liver inflammation and damage
Examples of viral hepatitis include:
- Hepatitis A virus
- Hepatitis B virus
- Hepatitis C virus
- Hepatitis D virus
- Hepatitis E virus
What is Hepatitis A Virus?
Hepatitis A virus is an inflammation transmitted through ingestion of contaminated food and water or direct contact with an infectious person.
What is Hepatitis B Virus?
Hepatitis B virus is a vaccine-preventable liver infection spread when blood, semen, or other body fluids from a person infected with the virus enters the body of someone who is not infected.
What is Hepatitis C Virus?
Hepatitis C virus is a liver infection spread through contact with blood from an infected person.
What is Hepatitis D Virus?
Hepatitis D virus is an infection that causes the liver to become inflamed.
What is Hepatitis E Virus?
Hepatitis E virus is a liver infection spread mainly through the fecal-oral transmission route.
What is the Pathology of Viral Hepatitis?
The pathology of viral hepatitis is:
-Etiology: The cause of viral hepatitis a viral infection.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to viral hepatitis as follows:
- Hepatitis A: Unknown.
- Hepatitis B: Interaction of the virus and the host immune system.
- Hepatitis C: Host immunity and metabolic changes including oxidative stress, insulin resistance, and hepatic steatosis.
- Hepatitis D: Interferon-α signaling inhibition, HDV-specific T-lymphocyte activation, and cytokine responses, and tumor necrosis factor-alpha and nuclear factor kappa B signaling.
- Hepatitis E: poorly understood and unspecific.
-Histology: The histology associated with viral hepatitis may show confluent necrosis, bridging necrosis, necrosis of entire lobules, and periportal necrosis.
How does Viral Hepatitis Present?
Patients with viral hepatitis typically affect males present in the age range of 35-55. The symptoms, features, and clinical findings associated with acute HAV infection are marked by several weeks of malaise, anorexia, nausea, vomiting, and elevated aminotransferase levels. HBV and HCV are asymptomatic, however, the chronic HBV and HCV show fatigue. The HDV and HEV show the same clinical feature too.
How is Viral Hepatitis Diagnosed?
Viral hepatitis is diagnosed through a blood test.
How is Viral HepatitisTreated?
Viral hepatitis is treated by resting, resolving symptoms (pegylated interferon and ribavirin), and maintaining an adequate intake of fluids.
What is the Prognosis of Viral Hepatitis?
The prognosis of viral hepatitis A is good with an overall mortality of 0.02%, HBV is good as patients recover fully, HCV is fair with the clear virus within 6 months, HDV and HEV are good and patients recover fully.
| Viral Hepatitis | Hepatitis A | Hepatitis B | Hepatitis C | Hepatitis D | Hepatitis E |
| Transmission | Fecal-oral | blood | blood | blood | Fecal-oral |
| Incubation | 15-45 days | 45-160 days | 15-150 days | 30-60 days | 15-60 days |
| Treatment | No specific treatment | Antiviral medications | Antivirals, Combination drugs | No known treatments | No specific antiviral therapy |
| Prognosis | Good | Good | Fair | Good | Good |
What are Syndromes of Viral Hepatitis?
Syndromes of viral hepatitis are the collective medical sign and symptoms associated with the viral hepatitis.
What is Autoimmune Hepatitis?
Autoimmune hepatitis is liver inflammation that occurs when the body’s immune system turns against liver cells.
What is the Pathology of Autoimmune Hepatitis?
The pathology of autoimmune hepatitis is:
-Etiology: The cause of autoimmune hepatitis is related to autoimmune factors.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to autoimmune hepatitis includes genetic predisposition, molecular mimicry, and/or impairment of regulatory T-cells are involved in the initiation and perpetuation of the autoimmune liver attack.
-Histology: The histology associated with autoimmune hepatitis shows a chronic hepatitis pattern of injury with portal inflammation and interface activity, the predominance of plasma cells in the portal infiltrate, emperipolesis, and hepatocellular rosette formation.
How does Autoimmune Hepatitis Present?
Patients with autoimmune hepatitis typically affect females present in the age range of the 50s. The symptoms, features, and clinical findings associated with autoimmune hepatitis include anorexia, arthralgias, maculopapular rash, fatigue, and also acute hepatitis manifestations.
How is Autoimmune Hepatitis Diagnosed?
Autoimmune hepatitis is diagnosed based on a combination of characteristic clinical features and typical laboratory abnormalities.
How is Autoimmune Hepatitis Treated?
Autoimmune hepatitis is treated with corticosteroid therapy and liver transplantation.
What is the Prognosis of Autoimmune hepatitis?
The prognosis of autoimmune hepatitis is good with a 10-year survival rate.
What is Liver Injury?
Liver injury is a form of trauma sustained to the liver.
Liver injury may include:
- Drug-induced liver injury
- Toxin induced liver injury
- Drug-induced liver injury is the liver injury caused by certain drugs
- Toxin induced liver Injury is chemical-driven liver damage
What is the Pathology of Drug or Toxin Induced Liver Injury?
The pathology of drug and toxin-induced liver injury is:
-Etiology: The cause of drug and toxin-induced liver injury includes medications, herbal medications, dietary supplements, or other xenobiotics.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to drug-induced liver injury usually involves the participation of a toxic drug or metabolite that either elicits an immune response or directly affects the biochemistry of the cell.
-Histology: The histology associated with drug-induced liver injury shows lobular disarray, rosette formation, and hemorrhage.
How does Drug-Induced Liver Injury Present?
Patients with drug-induced liver injury typically affect females present at the age range of 35-55. The symptoms, features, and clinical findings associated with the drug-induced liver injury include jaundice, belly pain, nausea, vomiting, lack of appetite, dark urine, and pale-colored stool.
How is Drug-Induced Liver Injury Diagnosed?
Drug-induced liver injury is diagnosed using liver biopsy.
How is Drug-Induced Liver Injury Treated?
Drug-induced liver injury is treated by stopping the medication which is causing it.
What is the Prognosis of Drug-Induced Liver Injury?
The prognosis of drug-induced liver injury is good with usually reversible and benign.
What is Liver Disease?
Liver disease is any disease that negatively affects the normal, healthy performance of the liver.
Examples of liver disease include:
- Alcoholic liver disease
- Metabolic liver disease
- Alpha-1-antitrypsin deficiency
- Hemochromatosis
- Nonalcoholic fatty liver disease
- Wilson disease
What is Alcoholic Liver Disease?
Alcoholic liver disease is a result of over-consuming alcohol that damages the liver, leading to a buildup of fats, inflammation, and scarring.
What is the Pathology of Alcoholic Liver Disease?
The pathology of alcoholic liver disease is:
-Etiology: The cause of the alcoholic liver disease is overconsuming alcohol.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to an alcoholic liver disease involves secretion of pro-inflammatory, oxidative stress, lipid peroxidation, and acetaldehyde toxicity. These factors cause inflammation, apoptosis, and eventually fibrosis of liver cells.
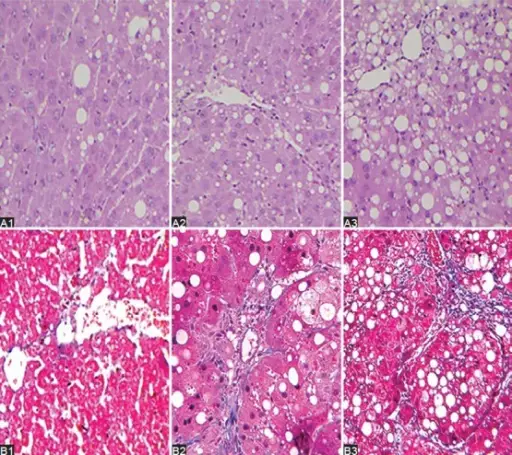
-Histology: The histology associated with alcoholic liver disease shows macrovesicular steatosis, neutrophilic lobular inflammation, ballooning degeneration, Mallory-Denk bodies, portal, and fibrosis that is pericellular.
How does Alcoholic Liver Disease Present?
Patients with the alcoholic liver disease typically affect females present in the age range of 25-34. The symptoms, features, and clinical findings associated with alcoholic liver disease include abdominal pain and tenderness, dry mouth and increased thirst, fatigue, jaundice, portal hypertension, enlarged spleen, ascites, and kidney failure.
How is Alcoholic Liver Disease Diagnosed?
Alcoholic liver disease is diagnosed by blood tests, liver biopsy, CT scan, and ultrasound.
How is Alcoholic Liver Disease Treated?
Alcoholic liver disease is treated medical and lifestyle management.
What is the Prognosis of Alcoholic Liver Disease?
The prognosis of alcoholic liver disease is fair with a survival rate of 60%.
What is Metabolic Liver Disease?
Metabolic liver disease disorder in which abnormal chemical reactions in the body disrupt metabolism
What is the Pathology of Metabolic Liver Disease?
The pathology of metabolic liver disease is:
-Etiology: The cause of the metabolic liver disease is genetic.
-Genes involved: PiZZ.
-Pathogenesis: The sequence of events that lead to metabolic liver disease shows necrosis of hepatocytes stimulates immune cells to release cytokines, growth factors, and various unknown chemicals.
-Histology: The histology associated with metabolic liver disease shows hepatocellular rosette formation.
How does Metabolic Liver Disease Present?
Patients with metabolic liver disease typically affect males present at the age range of 35-55. The symptoms, features, and clinical findings associated with metabolic liver disease include itching, jaundice, difficulty gaining weight, low blood sugar level, fat-soluble vitamin deficiencies, liver scarring, and fatigue.
How is Metabolic Liver Disease Diagnosed?
Metabolic liver disease is diagnosed using a blood test and urine analysis.
How is Metabolic Liver Disease Treated?
Metabolic liver disease is treated using therapeutic phlebotomy.
What is the Prognosis of Metabolic Liver Disease?
The prognosis of metabolic liver disease is fair with a life expectancy of up to 10 years.
What is Alpha-1-Antitrypsin Deficiency?
Alpha-1-antitrypsin deficiency is a genetic disorder that may result in lung disease or liver disease.
What is the Pathology of Alpha-1-Antitrypsin Deficiency?
The pathology of alpha-1-antitrypsin deficiency is:
-Etiology: The cause of alpha-1-antitrypsin deficiency is changing (pathogenic variants, also known as mutations ) in the SERPINA1 gene.
-Genes involved: SERPINA1
-Pathogenesis: The sequence of events that lead to alpha-1-antitrypsin deficiency includes a mutation in the SERPINA1 gene
-Histology: The histology associated with alpha-1-antitrypsin deficiency shows periportal red hyaline globules with periodic acid-Schiff (PAS) stain
How does Alpha-1-Antitrypsin Deficiency Present?
Patients with alpha-1-antitrypsin deficiency typically affect males and females present at an age range of 30-50 years old. The symptoms, features, and clinical findings associated with alpha-1-antitrypsin deficiency include Shortness of breath and wheezing, repeated lung infections, tiredness, rapid heartbeat upon standing, vision problems, and weight loss
How is Alpha-1-Antitrypsin Deficiency Diagnosed?
Alpha-1-antitrypsin deficiency is diagnosed using blood tests and liver biopsy.
How is Alpha-1-Antitrypsin Deficiency Treated?
Alpha-1-antitrypsin deficiency is treated with bronchodilators, inhaled steroids, antibiotics, and intravenous infusions
What is the Prognosis of Alpha-1-Antitrypsin Deficiency?
The prognosis of alpha-1-antitrypsin deficiency is good with a normal life expectancy.
What is Hemochromatosis?
Hemochromatosis or iron overload is a condition in which the body stores too much iron.
What is the Pathology of Hemochromatosis?
The pathology of hemochromatosis is:
-Etiology: The cause of hemochromatosis is the mutations in iron metabolism genes, such as HFE
-Genes involved: HFE.
-Pathogenesis: The sequence of events that lead to hemochromatosis involves iron to be absorbed by duodenal enterocytes via divalent metal transporter 1 (DMT1).
-Histology: The histology associated with hemochromatosis shows a pericanalicular pattern with iron appearing as a dark brown granular pigment, predominantly within hepatocytes.
How does Hemochromatosis Present?
Patients with hemochromatosis typically affect male present at age range of 40-60. The symptoms, features, and clinical findings associated with hemochromatosis include liver cirrhosis, diabetes mellitus, bronzing of the skin, joint pain, fatigue, and abdominal pain.
How is Hemochromatosis Diagnosed?
Hemochromatosis is diagnosed using liver biopsy, MRI, and blood tests.
How is Hemochromatosis Treated?
Hemochromatosis is treated with therapeutic phlebotomy/venesection or chelation therapy.
What is the Prognosis of Hemochromatosis?
The prognosis of hemochromatosis is good though, but poor after the development of cirrhosis, hepatocellular carcinoma, diabetes, or cardiomyopathy.
What is Nonalcoholic Fatty Liver Disease?
Nonalcoholic fatty liver disease is the liver conditions affecting people who drink little to no alcohol that results in fat abnormal deposition in the liver.
What is the Pathology of Nonalcoholic Fatty Liver Disease?
The pathology of nonalcoholic fatty liver disease is:
-Etiology: The cause of the nonalcoholic fatty liver disease is unknown
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to nonalcoholic fatty liver disease includes insulin resistance as the key mechanism leading to hepatic steatosis, and perhaps also to steatohepatitis.
-Histology: The histology associated with nonalcoholic fatty liver disease shows macrovesicular steatosis, but may be composed of a mixture of large and small vacuoles
How does Nonalcoholic Fatty Liver Disease Present?
Patients with the nonalcoholic fatty liver disease typically affects male present at the age range of 40-49 years. The symptoms, features, and clinical findings associated with nonalcoholic fatty liver disease include fatigue, pain or discomfort in the upper right abdomen, jaundice, ascites, enlarged spleen, and red palms.
How is Nonalcoholic Fatty Liver Disease Diagnosed?
Nonalcoholic fatty liver disease is diagnosed using CT, MRI, and biopsy.
How is Nonalcoholic Fatty Liver Disease Treated?
Nonalcoholic fatty liver disease is treated by lifestyle management.
What is the Prognosis of Nonalcoholic Fatty Liver Disease?
The prognosis of nonalcoholic fatty liver disease is good.
What is Wilson Disease?
Wilson disease is an autosomal recessive disorder causing accumulation of toxic levels.
What is the Pathology of Wilson Disease?
The pathology of Wilson disease is:
-Etiology: The cause of wilson disease is mutations in the ATP7B gene.
-Genes involved: ATP7B gene.
-Pathogenesis: The sequence of events that lead to wilson disease includes free copper dissociates and is transferred to hepatocytes, where it is incorporated into an alpha2 globulin to form ceruloplasmin and resecreted into plasma.
-Histology: The histology associated with wilson disease shows fatty change with vacuolated nucleus (due to glycogen or water), and focal hepatocyte necrosis.
How does Wilson Disease Present?
Patients with wilson disease typically affects male and female present at the age range of 40s. The symptoms, features, and clinical findings associated with wilson disease include acute or chronic liver disease, hemolytic anemia, deposition in putamen with frank psychosis or Parkinsonian symptoms, deposition in cornea called Kayser Fleischer rings.
How is Wilson Disease Diagnosed?
Wilson disease is diagnosed with the serum ceruloplasmin < 20 mg/dl, increased liver copper using rhodamine stain, urinary copper excretion > 50 mcg/24 hours.
How is Wilson Disease Treated?
Wilson disease is treated with longterm copper chelation therapy with D-penicillamine and liver transplantation.
What is the Prognosis of Wilson Disease?
The prognosis of wilson disease is is good.
What is Cholestatic Disease?
Cholestatic diseases is due to the defective bile acid transport from the liver to the intestine
What is the Pathology of Cholestatic Diseases?
The pathology of cholestatic diseases is:
-Etiology: The cause of cholestatic diseases is the primary damage to the biliary epithelium
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to cholestatic diseases includes genetic defects, mechanical aberrations, toxins, or dysregulations in the immune system that damage the bile ducts and cause accumulation of bile and liver tissue damage.
-Histology: The histology associated with cholestatic diseases shows hepatic parenchyma with abnormal bile.
How does Cholestatic Diseases Present?
Patients with cholestatic diseases typically affects male and female present at the age range of 40-50. The symptoms, features, and clinical findings associated with cholestatic diseases include jaundice, ascites, light colored stool, dark urine, nausea, and excessive itching.
How is Cholestatic Diseases Diagnosed?
Cholestatic diseases is diagnosed using ultrasound and CT scan.
How is Cholestatic Diseases Treated?
Cholestatic diseases is treated with ursodeoxycholic acid and obeticholic acid
What is the Prognosis of Cholestatic Diseases?
The prognosis of cholestatic diseases is fair if treated at on early stage.
How are Bile and Bilirubin Formed?
Bile and bilirubin are formed by the liver.
What is Cholestasis?
Cholestasis is defined as a decrease in bile flow due to impaired secretion by hepatocytes or to obstruction of bile flow through intra-or extrahepatic bile ducts.
What is Cholestasis of Sepsis?
Cholestasis of sepsis is a form of hepatocellular cholestasis that arises during or following a septic process and results from impairment in bile transport.
What is Jaundice?
Jaundice is the condition in which the skin, whites of the eyes, and mucous membranes turn yellow because of a high level of bilirubin.
Causes of jaundice include:
- Bile duct obstruction
- Neonatal cholestasis
- Biliary atresia
- Primary hepatolithiasis
What is Bile Duct Obstruction?
Bile duct obstruction is a condition when one of the ducts that carry bile from the liver to the intestine via the gallbladder becomes blocked.
What is the Pathology of Bile Duct Obstruction?
The pathology of bile duct obstruction is:
-Etiology: The cause of bile duct obstruction is gallstones
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to bile duct obstruction might include pancreatitis or an injury to the abdomen.
-Histology: The histology associated with bile duct obstruction shows centrilobular canalicular cholestasis, followed shortly by portal tract edema, ductular reaction, and mild chronic inflammation.
How does Bile Duct Obstruction Present?
Patients with bile duct obstruction typically affect females present at the age range of 30-40. The symptoms, features, and clinical findings associated with bile duct obstruction include jaundice, nausea, vomiting, abdominal pain, fever. Without treatment, bile duct obstruction may progress to fibrosis and cirrhosis with duct loss.
How is Bile Duct Obstruction Diagnosed?
Bile duct obstruction is diagnosed typically by clinical presentation and radiologic findings.
How is Bile Duct Obstruction Treated?
Bile duct obstruction is treated with cholecystectomy and an ERCP.
What is the Prognosis of Bile Duct Obstruction?
The prognosis of bile duct obstruction is poor causing life-threatening infections.
What is Neonatal Cholestasis?
Neonatal cholestasis is prolonged jaundice beyond 2 weeks of age.
What is the Pathology of Neonatal Cholestasis?
The pathology of neonatal cholestasis is:
-Etiology: The cause of neonatal cholestasis is intrahepatic neonatal cholestasis.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to neonatal cholestasis includes elevated conjugated bilirubin levels in the newborn period.
-Histology: The histology associated with neonatal cholestasis shows lobular changes: giant cell transformation (hepatocytes containing 4 – 10 nuclei), variable lobular inflammatory infiltrate and necrosis (spotty, confluent to bridging), canalicular ± hepatocellular bilirubinostasis, extramedullary hematopoiesis.
How does Neonatal Cholestasis Present?
Patients with neonatal cholestasis typically affect newborns. The symptoms, features, and clinical findings associated with neonatal cholestasis include jaundice, cirrhosis, hepatomegaly, ascites, and itching.
How is Neonatal Cholestasis Diagnosed?
Neonatal cholestasis is diagnosed through ultrasonography, and hepatobiliary.
How is Neonatal Cholestasis Treated?
Neonatal cholestasis has no specific treatment, only symptomatic relief is provided
What is the Prognosis of Neonatal Cholestasis?
The prognosis of neonatal cholestasis is fair depending upon the severity of the disease.
What is Biliary Atresia?
Biliary atresia is a condition in infants in which the bile ducts outside and inside the liver are scarred and blocked.
What is the Pathology of Biliary Atresia?
The pathology of biliary atresia is:
-Etiology: The cause of biliary atresia is not clear, but could be due to inflammation of and scarring caused by problems with the immune system.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to biliary atresia includes obliteration or discontinuity of the extrahepatic biliary system, resulting in obstruction of bile flow.
-Histology: The histology associated with biliary atresia shows lobular cholestasis, portal neutrophilic infiltrate, bile ductular proliferation (peaks at 200 days), with elongated and angulated ductules and occasional bile plugs.
How does Biliary Atresia Present?
Patients with biliary atresia typically affect females (girls) present at the age range of 2-15. The symptoms, features, and clinical findings associated with biliary atresia include light beige stools, dark brown urine, swollen belly, difficulty gaining weight, ascites, and liver failure after several months if the biliary atresia is not treated.
How is Biliary Atresia Diagnosed?
Biliary atresia is diagnosed using CBC, liver biopsy, and ultrasound.
How is Biliary Atresia Treated?
Biliary atresia is treated using the Kasai surgical procedure.
What is the Prognosis of Biliary Atresia?
The prognosis of biliary atresia is fair.
What is Primary Hepatolithiasis?
Primary hepatolithiasis is the presence of gallstones in the biliary ducts of the liver.
What is the Pathology of Primary Hepatolithiasis?
The pathology of primary hepatolithiasis is:
-Etiology: The cause of primary hepatolithiasis is not clear, however, thought to be genetics, diets, and environmental causes.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to primary hepatolithiasis includes pigmented calcium bilirubin stones within dilated intrahepatic bile ducts featuring chronic inflammation, mural fibrosis, and proliferation of peribiliary glands, without extrahepatic biliary obstruction.
-Histology: The histology associated with primary hepatolithiasis shows the presence of calculi in the intrahepatic biliary tree and accompanying inflammation.
How does Primary Hepatolithiasis Present?
Patients with primary hepatolithiasis typically affect males and females present at the age range of 50-70. The symptoms, features, and clinical findings associated with primary hepatolithiasis include abdominal pain, jaundice, and fever.
How is Primary Hepatolithiasis Diagnosed?
Primary hepatolithiasis is diagnosed using abdominal imaging.
How is Primary Hepatolithiasis Treated?
Primary hepatolithiasis is treated by doing surgery.
What is the Prognosis of Primary Hepatolithiasis?
The prognosis of primary hepatolithiasis is fair depending upon the cause.
What are Autoimmune Cholangiopathies?
Autoimmune cholangiopathies are those with the overlapping features of primary biliary cirrhosis and autoimmune hepatitis
Examples of autoimmune cholangiopathies include:
- Primary biliary cirrhosis (PBC)
- Primary sclerosing cholangitis (PSC)
What is Primary Biliary Cirrhosis?
Primary biliary cirrhosis is autoimmune in nature, that leads to progressive cholestasis and often end-stage liver disease.
What is the Pathology of Primary Biliary Cirrhosis?
The pathology of primary biliary cirrhosis is:
-Etiology: The cause of primary biliary cirrhosis is not clear.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to primary biliary cirrhosis includes a breakdown of immune tolerance to mitochondrial and nuclear antigens, causing injury to the biliary epithelial cells (BEC) lining the small intrahepatic bile ducts.
-Histology: The histology associated with primary biliary cirrhosis shows dense lymphocytic infiltrate in portal tracts with granulomatous destruction and loss of medium-sized interlobular bile ducts, focal and variable within the liver.
How does Primary Biliary Cirrhosis Present?
Patients with primary biliary cirrhosis typically affect females present at the age range of 35-60 The symptoms, features, and clinical findings associated with primary biliary cirrhosis include dry eyes and mouth, pain in the upper right abdomen, splenomegaly, musculoskeletal pain, edema, and ascites.
How is Primary Biliary Cirrhosis Diagnosed?
Primary biliary cirrhosis is diagnosed using a blood test (AMA) and ultrasound.
How is Primary Biliary Cirrhosis Treated?
Primary biliary cirrhosis is treated with ursodeoxycholic acid
What is the Prognosis of Primary Biliary Cirrhosis?
The prognosis of primary biliary cirrhosis is good with the symptoms free life up to 10 years.
What is Primary Sclerosing Cholangitis?
Primary sclerosing cholangitis is a disease of bile ducts.
What is the Pathology of Primary Sclerosing Cholangitis?
The pathology of primary sclerosing cholangitis is:
-Etiology: The cause of primary sclerosing cholangitis is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to primary sclerosing cholangitis includes progressive inflammation, fibrosis, and structuring of the intrahepatic and extrahepatic bile ducts.
-Histology: The histology associated with primary sclerosing cholangitis shows classic finding is “onion skin” fibrosis around affected medium-sized bile ducts; smaller ducts are rarely affected.
How does Primary Sclerosing Cholangitis Present?
Patients with primary sclerosing cholangitis typically affect males present at the age range of 20-60. The symptoms, features, and clinical findings associated with primary sclerosing cholangitis include fatigue, pruritus, jaundice, right upper quadrant pain/tenderness.
How is Primary Sclerosing Cholangitis Diagnosed?
Primary sclerosing cholangitis is diagnosed with liver biopsy, CT scan, and MRI.
How is Primary Sclerosing Cholangitis Treated?
Primary sclerosing cholangitis is treated using ursodeoxycholic acid or liver transplantation.
What is the Prognosis of Primary Sclerosing Cholangitis?
The prognosis of primary sclerosing cholangitis is poor with a median length of survival from diagnosis to death being approximately 12 years.
What are Structural Anomalies of the Biliary Tree?
Structural anomalies of the biliary tree are the anomalies of the pancreatic or bile duct.
Examples of structural anomalies of the biliary tree include:
- Choledochal cysts
- Fibropolycystic disease
What are Choledochal Cysts?
Choledochal cysts are rare congenital dilations that carry bile from the liver to the small intestine for digestion.
What is the Pathology of Choledochal Cysts?
The pathology of choledochal cysts is:
-Etiology: The cause of choledochal cysts is the abnormal intersection between the bile duct and pancreatic duct.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to choledochal cysts includes defects in epithelialization and recanalization of the developing bile ducts and congenital weakness of the ductal wall.
-Histology: The histology associated with choledochal cysts shows focal columnar epithelium, walls composed of dense fibrous tissue, scattered smooth muscle, and elastic fibers.
How does Choledochal Cysts Present?
Patients with choledochal cysts typically affect children (girls) and are usually congenital. The symptoms, features, and clinical findings associated with choledochal cysts include abdominal mass, pain in the right upper belly, jaundice, nausea and vomiting.
How is Choledochal Cysts Diagnosed?
Choledochal cysts is diagnosed using ultrasound, CT scan, and cholangiography.
How is Choledochal Cysts Treated?
Choledochal cysts is treated with bile duct surgery with total cyst removal.
What is the Prognosis of Choledochal Cysts?
The prognosis of choledochal cysts is good with early total resection and reconstruction.
What is Fibropolycystic Disease?
Fibropolycystic disease is the collective term for a group of congenital liver and biliary abnormalities resulting from abnormal development of the ductal plates.
What is the Pathology of Fibropolycystic Disease?
The pathology of fibropolycystic disease is:
-Etiology: The cause of fibropolycystic disease is unknown, however, it is believed that estrogen is the main cause.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to fibropolycystic disease includes abnormal development of the embryonic ductal plates.
-Histology: The histology associated with fibropolycystic disease shows periportal fibrosis and irregularly shaped proliferating bile ducts.
How does Fibropolycystic Disease Present?
Patients with fibropolycystic disease typically affect females present at the age range of 25-45. The symptoms, features, and clinical findings associated with fibropolycystic disease include vauge abdominal symptoms.
How is Fibropolycystic Disease Diagnosed?
Fibropolycystic disease is diagnosed through a mammogram, ultrasound, and MRIs.
How is Fibropolycystic Disease Treated?
Fibropolycystic disease is treated with surgical excision and over-the-counter medications.
What is the Prognosis of Fibropolycystic Disease?
The prognosis of fibropolycystic disease is good if treated timely.
What are Circulatory Disorders of the Liver?
Circulatory disorders of the liver are the disorders with obstruction to hepatic vascular inflow, obstruction to blood flow through the liver, and obstruction to hepatic vascular outflow.
Circulatory disorders of the liver include:
- Hepatic venous outflow obstruction
- Impaired blood flow into the liver
- Impaired blood flow through the liver
- Passive congestion and centrilobular necrosis
What is Hepatic Venous Outflow Obstruction?
Hepatic venous outflow obstruction is the condition where there is partial or complete obstruction of the hepatic veins.
Examples of hepatic venous outflow obstruction include:
- Hepatic vein thrombosis
- Sinusoidal obstruction syndrome
What is Hepatic Vein Thrombosis?
Hepatic vein thrombosis is an obstruction in the hepatic veins of the liver.
What is the Pathology of Hepatic Vein Thrombosis?
The pathology of hepatic vein thrombosis is:
-Etiology: The cause of hepatic vein thrombosis is blood clot/thrombosis.
-Genes involved: Potentially clotting abnormalities.
-Pathogenesis: The sequence of events that lead to hepatic vein thrombosis includes outflow obstruction, patients often have decreased portal perfusion with an eventual compensatory increase in arterial inflow.
-Histology: The histology associated with hepatic vein thrombosis shows severe centrilobular congestion/necrosis, progressing to centrilobular fibrosis.
How does Hepatic Vein Thrombosis Present?
Patients with hepatic vein thrombosis typically affect males present at the age range of 35-55. The symptoms, features, and clinical findings associated with hepatic vein thrombosis include the buildup of fluid in the abdomen, enlarged liver, nausea, and vomiting, vomiting blood, unexplained weight loss, enlarged spleen, swelling of lower limbs, abdominal pain, and jaundice.
How is Hepatic Vein Thrombosis Diagnosed?
Hepatic vein thrombosis is diagnosed using ultrasound, CT scan, or biopsy.
How is Hepatic Vein Thrombosis Treated?
Hepatic vein thrombosis is treated with fibrinolytic drugs.
What is the Prognosis of Hepatic Vein Thrombosis?
The prognosis of hepatic vein thrombosis is good with the current 10-year survival rate to be 75%.
What is Sinusoidal Obstruction Syndrome?
Sinusoidal obstruction syndrome is the blockage of the very small (microscopic) veins in the liver.
What is the Pathology of Sinusoidal Obstruction Syndrome?
The pathology of sinusoidal obstruction syndrome is:
-Etiology: The cause of sinusoidal obstruction syndrome is the ingestion of pyrrolizidine alkaloids
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to sinusoidal obstruction syndrome includes a toxic agent which damages sinusoidal endothelial cells, likely via depletion of glutathione and nitric oxide.
-Histology: The histology associated with sinusoidal obstruction syndrome shows acutely, hemorrhage into markedly dilated sinusoids with hepatocyte atrophy; sinusoids are denuded, though this may be difficult to see clearly. Later, some regions of the liver heal while others show collapse; constriction/obliteration of small central veins by subendothelial swelling/fibrosis can be seen.
How does Sinusoidal Obstruction Syndrome Present?
Patients with sinusoidal obstruction syndrome typically affect females present at the age range of 35-55. The symptoms, features, and clinical findings associated with sinusoidal obstruction syndrome include marked weight gain, tender hepatomegaly, ascites and jaundice, portal hypertension, and in rare cases cirrhosis.
How is Sinusoidal Obstruction Syndrome Diagnosed?
Sinusoidal obstruction syndrome is diagnosed using doppler and ultrasound.
How is Sinusoidal Obstruction Syndrome Treated?
Sinusoidal obstruction syndrome is treated with defibrotide sodium or mild diuretics.
What is the Prognosis of Sinusoidal Obstruction Syndrome?
The prognosis of sinusoidal obstruction syndrome is poor with an increased mortality rate.
What is Impaired Blood Flow Into The Liver?
Impaired blood flow into the liver is the inadequate blood flow towards the liver.
Examples of impaired blood flow into the liver include:
- Hepatic artery compromise
- Portal vein obstruction
- Portal vein thrombosis
What is Hepatic Artery Compromise?
Hepatic artery compromise is the blockage in blood flow to the liver.
What is the Pathology of Hepatic Artery Compromise?
The pathology of hepatic artery compromise is:
-Etiology: The cause of hepatic artery compromise is drugs or medication.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to hepatic artery compromise may include thrombosis, emboli, intragenic cause, vasculitis, and structural arterial abnormalization.
-Histology: The histology associated with hepatic artery compromise shows hepatic parenchymal necrosis.
How does Hepatic Artery Compromise Present?
Patients with hepatic artery compromise typically affect males and females present at the age range of 30-50. The symptoms, features, and clinical findings associated with hepatic artery compromise include may be asymptomatic or cause right upper quadrant pain, fever, nausea, vomiting, and jaundice. Leukocytosis and a high aminotransferase level are common.
How is Hepatic Artery Compromise Diagnosed?
Hepatic artery compromise is diagnosed using vascular imagining.
How is Hepatic Artery Compromise Treated?
Hepatic artery compromise is treated using anticoagulant medications, and fibrinolytic therapies.
What is the Prognosis of Hepatic Artery Compromise?
The prognosis of hepatic artery compromise is fair depending upon the cause.
What is Portal Vein Obstruction?
Portal vein obstruction is the blockage or narrowing of the portal vein by a blood clot.
What is the Pathology of Portal Vein Obstruction?
The pathology of portal vein obstruction is:
-Etiology: The cause of portal vein obstruction is prothrombotic disorders, tumor thrombus, cirrhosis, pancreatitis, various infections
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to portal vein obstruction hepatic artery buffer response allows for increased arterial flow to the liver when the portal vein is obstructed.
-Histology: The histology associated with portal vein obstruction no bridging fibrosis, can mimic cirrhosis.
How does Portal Vein Obstruction Present?
Patients with portal vein obstruction typically affect males present at the age range of 35-55. The symptoms, features, and clinical findings associated with portal vein obstruction include abdominal pain, ascites (massive, intractable), portal hypertension, and bowel infarction.
How is Portal Vein Obstruction Diagnosed?
Portal vein obstruction is diagnosed via CT scan.
How is Portal Vein Obstruction Treated?
Portal vein obstruction is treated with anticoagulation medicine if caused by acute portal vein thrombosis.
What is the Prognosis of Portal Vein Obstruction?
The prognosis of portal vein obstruction is fair depending upon the cause.
What is Portal Vein Thrombosis?
Portal Vein Thrombosis is the blockage or narrowing of the portal vein by a blood clot
What is the Pathology of Portal Vein Thrombosis?
The pathology of portal vein thrombosis is:
-Etiology: The cause of portal vein thrombosis is prothrombotic disorders, tumor thrombus, cirrhosis, pancreatitis, various infections
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to portal vein thrombosis includes hepatic artery buffer response allows for increased arterial flow to the liver when the portal vein is obstructed.
-Histology: The histology associated with portal vein thrombosis shows no bridging fibrosis, can mimic cirrhosis.
How does Portal Vein Thrombosis Present?
Patients with portal vein thrombosis typically affect males present in the age range of 35-55. The symptoms, features, and clinical findings associated with portal vein thrombosis include abdominal pain, ascites (massive, intractable), portal hypertension, and bowel infarction.
How is Portal Vein Thrombosis Diagnosed?
Portal vein thrombosis is diagnosed via CT scan.
How is Portal Vein Thrombosis Treated?
Portal vein thrombosis is treated with anticoagulation medicine if caused by acute portal vein thrombosis.
What is the Prognosis of Portal Vein Thrombosis?
The prognosis of portal vein thrombosis is fair depending upon the cause.
What is Impaired Blood Flow Through The Liver?
Impaired Blood Flow Through The Liver is the inadequate blood flow towards the liver.
What is the Pathology of Impaired Blood Flow Through The Liver?
The pathology of impaired blood flow through the liver is:
-Etiology: The cause of impaired blood flow through the liver is impairment of the portal vein.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to impaired blood flow through the liver includes impairment in the portal vein, leading to portal hypertension.
-Histology: The histology associated with impaired blood flow through the liver shows collapsed portal veins.
How does Impaired Blood Flow Through The Liver Present?
Patients with impaired blood flow through the liver typically affects male and female present at the age range of 25-55. The symptoms, features, and clinical findings associated with impaired blood flow through the liver include nausea, vomiting, ascites, jaundice, inflammation, congestion, itchy skin, dark-colored urine, and fatigue.
How is Impaired Blood Flow Through The Liver Diagnosed?
Impaired blood flow through the liver is diagnosed CT scan, ultrasound, and MRI.
How is Impaired Blood Flow Through The Liver Treated?
Impaired blood flow through the liver is treated using beta-blockers.
What is the Prognosis of Impaired Blood Flow Through The Liver?
The prognosis of impaired blood flow through the liver is poor.
What is Passive Congestion of the Liver?
Passive congestion of the liver is the acute liver injury due to a sudden, profound reduction in systemic blood flow.
What is the Pathology of Passive Congestion of the Liver?
The pathology of passive congestion of the liver is:
-Etiology: The cause of passive congestion of the liver is congestive heart failure, restrictive cardiomyopathy, constrictive pericarditis, a right sided valvular disease involving the tricuspid or pulmonary valves, severe hypovolemia, septic shock, massive pulmonary embolism, hyperpyrexia, heat stroke
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to passive congestion of the liver includes stasis of blood in the hepatic parenchyma, due to impaired hepatic venous drainage, leads to the dilation of central hepatic veins and hepatomegaly; elevated hepatic venous pressure, and decrease in hepatic venous flow causes hypoxic injury to hepatocytes and eventual diffuse hepatocyte death and fibrosis.
-Histology: The histology associated with passive congestion of the liver shows centrilobular ischemic necrosis and hepatic infarction.
How does Passive Congestion of the Liver Present?
Patients with passive congestion of the liver typically affect males present at the age range of 25-50. The symptoms, features, and clinical findings associated with passive congestion of the liver include mild right upper quadrant abdominal pain, and right-sided heart failure.
How is Passive Congestion of the Liver Diagnosed?
Passive congestion of the liver is diagnosed using a CT scan, MRI, ultrasound, and biopsy.
How is Passive Congestion of the Liver Treated?
Passive congestion of the liver is treated with surgical excision.
What is the Prognosis of Passive Congestion of the Liver?
The prognosis of passive congestion of the liver is poor with a higher mortality rate.
What is Centrilobular Necrosis of the Liver?
Centrilobular necrosis of the liver is the necrosis of the centrilobular tissue of the hepatic lobule.
What is the Pathology of Centrilobular Necrosis of the Liver?
The pathology of centrilobular necrosis of the liver is:
-Etiology: The cause of centrilobular necrosis of the liver is hepatotoxins
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to centrilobular necrosis of the liver includes ischemia, drugs, venous outflow impairment, preservation/reperfusion injury, and alcoholic hepatitis.
-Histology: The histology associated with centrilobular necrosis of the liver shows ischemic necrosis characterized by coagulative hepatocyte necrosis, pyknotic or karyorrhectic nuclei, sharply demarcated with apoptotic bodies at the interface of healthy and necrotic hepatocytes; sinusoidal dilation and congestion can be prominent if a component of right-sided heart failure is present.
How does Centrilobular Necrosis of the Liver Present?
Patients with centrilobular necrosis of the liver typically affect males present at the age range of 20-45 years. The symptoms, features, and clinical findings associated with centrilobular necrosis of the liver include abrupt onset of nausea, weakness, fatigue, abdominal pain, and vomiting.
How is Centrilobular Necrosis of the Liver Diagnosed?
Centrilobular necrosis of the liver is diagnosed using LFT, ALT levels, CT scan, and MRI.
How is Centrilobular Necrosis of the Liver Treated?
Centrilobular necrosis of the liver is treated with surgical resection.
What is the Prognosis of Centrilobular Necrosis of the Liver?
The prognosis of centrilobular necrosis of the liver is poor with an increased mortality rate.
What is Liver Disease Associated with Pregnancy?
Liver disease associated with pregnancy is a pregnancy-related liver disease.
Liver disease associated with pregnancy includes:
- Acute fatty liver of pregnancy
- Eclampsia
- Preeclampsia
- Intrahepatic cholestasis of pregnancy
What is Acute Fatty Liver of Pregnancy?
Acute fatty liver of pregnancy is an obstetric emergency characterized by maternal liver dysfunction and/or failure that can lead to maternal and fetal complications, including death.
What is Eclampsia?
Eclampsia is most commonly defined as the new onset of convulsions and/or coma during pregnancy or in the immediate postpartum period in the presence of preeclampsia.
What is the Pathology of Eclampsia?
The pathology of eclampsia is:
-Etiology: The cause of eclampsia is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to eclampsia includes acute hypertension leads to cytotoxic edema formation, regional hypoperfusion, and ischemic damage causing cerebral arteries to undergo vasospasm.
-Histology: The histology associated with eclampsia show placenta with villous ischemia (increased syncytial knots, thickening of trophoblastic basement membrane, villous hypervascularity, villous agglutination, and infarction), fibrinoid necrosis of uterine vessels and acute atherosis; more tortuous or densely distributed spiral and basal arteries than normal.
How does Eclampsia Present?
Patients with eclampsia typically affect females present at the age range of less than 20. The symptoms, features, and clinical findings associated with eclampsia include convulsions, seizures, changes in mental status, frontal and/or occipital headaches, nausea, and/or visual changes.
How is Eclampsia Diagnosed?
Eclampsia is diagnosed with high blood pressure in 3rd trimester.
How is Eclampsia Treated?
Eclampsia is treated by establishing a patent airway and ensuring maternal oxygenation, prophylaxis, and BP management by labetalol.
What is the Prognosis of Eclampsia?
The prognosis of eclampsia is good with full recovery in a few days or months.
What is Preeclampsia?
Preeclampsia is a condition with high blood pressure in pregnant women.
What is the Pathology of Preeclampsia?
The pathology of preeclampsia is:
-Etiology: The cause of preeclampsia is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to preeclampsia include defective spiral artery remodeling.
-Histology: The histology associated with preeclampsia shows placenta with villous ischemia (increased syncytial knots, thickening of trophoblastic basement membrane, villous hypovascularity, villous agglutination, and infarction), fibrinoid necrosis of uterine vessels and acute atherosis; more tortuous or densely distributed spiral and basal arteries than normal.
How does Preeclampsia Present?
Patients with preeclampsia typically affect females present at the age range of less than 20. The symptoms, features, and clinical findings associated with preeclampsia include protein in the urine, swelling in the legs, feet, and hands, weight gain, shoulder pain, belly pain, trouble breathing, and vision changes.
How is Preeclampsia Diagnosed?
Preeclampsia is diagnosed by high blood pressure and also proteinuria, low platelet count, pulmonary edema.
How is Preeclampsia Treated?
Preeclampsia is treated by establishing a patent airway and ensuring maternal oxygenation, prophylaxis, and BP management by labetalol.
What is the Prognosis of Preeclampsia?
The prognosis of preeclampsia is good with full recovery in a few days or months.
What is Intrahepatic Cholestasis of Pregnancy?
Intrahepatic cholestasis of pregnancy is the condition that disturbs the normal flow of bile.
What is the Pathology of Intrahepatic Cholestasis of Pregnancy?
The pathology of intrahepatic cholestasis of pregnancy is:
-Etiology: The cause of intrahepatic cholestasis of pregnancy is bile.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to intrahepatic cholestasis of pregnancy includes a defect in excretion of bile salts, which leads to increased serum bile acids.
-Histology: The histology associated with intrahepatic cholestasis of pregnancy shows microvesicular steatosis in zones 2 or 3 (vacuoles may be very small).
How does Intrahepatic Cholestasis of Pregnancy Present?
Patients with intrahepatic cholestasis of pregnancy typically affect females present at the age range of 20 and above. The symptoms, features, and clinical findings associated with intrahepatic cholestasis of pregnancy include severe itching, dark urine or light-colored bowel movements, jaundice, loss of appetite, and nausea.
How is Intrahepatic Cholestasis of Pregnancy Diagnosed?
Intrahepatic cholestasis of pregnancy is diagnosed using physical examination and blood tests.
How is Intrahepatic Cholestasis of Pregnancy Treated?
Intrahepatic cholestasis of pregnancy is treated with ursodeoxycholic acid or to terminate the pregnancy.
What is the Prognosis of Intrahepatic Cholestasis of Pregnancy?
The prognosis of intrahepatic cholestasis of pregnancy is poor with most leading to pregnancy termination.
What are Tumors of the Liver?
Tumors of the liver are malignancies that originate or metastasize to the liver.
Tumors of the liver include:
- Nodular hyperplasias
- Hepatocellular adenomas
- Cholangiocarcinoma
- Hepatoblastoma
- Hepatocellular carcinoma
- Metastasis
What are Nodular Hyperplasias of the Liver?
Nodular hyperplasias of the liver are the benign tumors of the liver.
What is the Pathology of Nodular Hyperplasias of the Liver?
The pathology of nodular hyperplasias of the liver is:
-Etiology: The cause of nodular hyperplasias of the liver is the increased hepatocyte number caused by hypoperfusion or hyperperfusion from anomalous arteries within the hepatic lobule.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to nodular hyperplasias of the liver is unknown, however, it is characterized by a well-circumscribed region of hyperplastic liver parenchyma containing a stellate fibrous scar.
-Histology: The histology associated with nodular hyperplasias of the liver shows hyperplastic hepatocytes.
How does Nodular Hyperplasias of the Liver Present?
Patients with nodular hyperplasias of the liver typically affect young women present at the age range of 20-35. The symptoms, features, and clinical findings associated with nodular hyperplasias of the liver include a lump or pain in the stomach. However, most are asymptomatic.
How is Nodular Hyperplasias of the Liver Diagnosed?
Nodular hyperplasias of the liver is diagnosed through CT scan, MRI, tumor markers, and biopsy.
How is Nodular Hyperplasias of the Liver Treated?
Nodular hyperplasias of the liver is treated through surgical resection or hepatectomy.
What is the Prognosis of Nodular Hyperplasias of the Liver?
The prognosis of nodular hyperplasias of the liver is good if treated early and promptly.
What are Hepatocellular Adenomas?
Hepatocellular Adenomas are the benign neoplasm of hepatocellular origin arising in the noncirrhotic liver
What is the Pathology of Hepatocellular Adenomas?
The pathology of hepatocellular adenomas is:
-Etiology: The cause of hepatocellular adenomas is the use of estrogen-based oral contraceptive pills
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to hepatocellular adenomas include generalized vascular ectasia that develops due to exposure of the vasculature of the liver to oral contraceptives and related synthetic steroids.
-Histology: The histology associated with hepatocellular adenomas shows a well-defined border between the lesion and background liver, composed of hepatocytes with no significant cytologic atypia.
How does Hepatocellular Adenomas Present?
Patients with hepatocellular adenomas typically affect female present at the age range of 31-47 years. The symptoms, features, and clinical findings associated with hepatocellular adenomas include sudden abdominal pain, low blood pressure, and internal bleeding.
How is Hepatocellular Adenomas Diagnosed?
Hepatocellular adenomas is diagnosed through ultrasound, MRI, CT scan.
How is Hepatocellular Adenomas Treated?
Hepatocellular adenomas is treated using surgical excision and suspension of oral contraceptive pills.
What is the Prognosis of Hepatocellular Adenomas?
The prognosis of hepatocellular adenomas is good with mortality in elective cases being less than 1%.
What is Cholangiocarcinoma?
Cholangiocarcinoma is a type of cancer that forms in the slender tubes (bile ducts) that carry the digestive fluid bile.
What is the Pathology of Cholangiocarcinoma?
The pathology of cholangiocarcinoma is:
-Etiology: The cause of cholangiocarcinoma is scarring of the liver or chronic liver disease.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to cholangiocarcinoma arises from the malignant transformation of the epithelial cells of the intrahepatic or extrahepatic bile ducts.
-Histology: The histology associated with cholangiocarcinoma shows desmoplastic stroma-rich adenocarcinoma with cholangiocyte differentiation.
How does Cholangiocarcinoma Present?
Patients with cholangiocarcinoma typically affect older males. The symptoms, features, and clinical findings associated with cholangiocarcinoma include jaundice, intensely itchy skin, white-colored stools, fever, and weight loss.
How is Cholangiocarcinoma Diagnosed?
Cholangiocarcinoma is diagnosed through liver function tests, tumor markers, CT, MRI, ultrasound, and biopsy.
How is Cholangiocarcinoma Treated?
Cholangiocarcinoma is treated through surgical excision, liver transplant, targeted drug therapy, and chemotherapy.
What is the Prognosis of Cholangiocarcinoma?
The prognosis of cholangiocarcinoma is fair.
What is Hepatoblastoma?
Hepatoblastoma is a rare type of childhood cancer that occurs in the liver
What is the Pathology of Hepatoblastoma?
The pathology of hepatoblastoma is:
-Etiology: The cause of hepatoblastoma is sporadic
-Genes involved: (if any just mention the genes here)
-Pathogenesis: The sequence of events that lead to hepatoblastoma arises from primary hepatoblasts or multipotent hepatic progenitor cells
-Histology: The histology associated with hepatoblastoma shows solid nests or glandular/acinar morphology, with papillae and pseudorosettes
How does Hepatoblastoma Present?
Patients with hepatoblastoma typically affect children( male) present at the age range of 5 months to 6 years old. The symptoms, features, and clinical findings associated with hepatoblastoma include abdominal enlargement, mass or pain, jaundice, anorexia, and weight loss.
How is Hepatoblastoma Diagnosed?
Hepatoblastoma is diagnosed using fine needle aspiration and biopsy.
How is Hepatoblastoma Treated?
Hepatoblastoma is treated with chemotherapy and surgical intervention. Liver transplantation may needed in some cases.
What is the Prognosis of Hepatoblastoma?
The prognosis of hepatoblastoma is good with the survival rate be around 90%.
What is Hepatocellular Carcinoma?
Hepatocellular carcinoma is the primary malignancy of the liver with hepatocellular differentiation.
What is the Pathology of Hepatocellular Carcinoma?
The pathology of hepatocellular carcinoma is:
-Etiology: The cause of hepatocellular carcinoma may be cirrhosis, infections, hepatitis B & C, and metabolic disorders.
-Genes involved: HFE.
-Pathogenesis: The sequence of events that lead to hepatocellular carcinoma include low grade dysplasia that progresses to carcinoma.
-Histology: The histology associated with hepatocellular carcinoma shows a well-circumscribed mass that appears tan-yellow to green.
How does Hepatocellular Carcinoma Present?
Patients with hepatocellular carcinoma typically affect males present at the age range of 28-65 years. The symptoms, features, and clinical findings associated with hepatocellular carcinoma include abdominal pain, weight loss, hepatomegaly and splenomegaly, jaundice, ascites.
How is Hepatocellular Carcinoma Diagnosed?
Hepatocellular carcinoma is diagnosed using ultrasound, CT, and MRI, fine needle aspiration, and biopsy.
How is Hepatocellular Carcinoma Treated?
Hepatocellular carcinoma is treated using surgical intervention, ablation therapy, and systemic therapy.
What is the Prognosis of Hepatocellular Carcinoma?
The prognosis of hepatocellular carcinoma is poor with a 5-year survival rate of 20%.
What are Metastasis to the Liver?
Metastasis to the liver are malignancies that originate from a different part pf the body that somehow travel and grow in the liver. Common malignancies that metastasis to the liver include colorectal cancer, melanoma, breast cancers, esophageal cancers, and stomach cancer.