Male genital system pathology is any disease or disorder that affects the male genital system, either structurally or functionally.
What are Congenital Anomalies of the Penis?
Congenital anomalies of the penis are the abnormal conditions of the penis that develop during the embryological development stage.
Congenital anomalies of the penis include:
- Epispadias
- Hypospadias
- Phimosis
What is Epispadias?
Epispadias is a birth defect with a consequential urethral opening at the dorsal surface of the penis.
What is the Pathology of Epispadias?
The pathology of epispadias is:
-Etiology: The cause of epispadias is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to epispadias still is unknown.
-Morphology: The morphology associated with epispadias shows glandular, penile, and penopubic forms depending on the position of the meatus.
How does Epispadias Present?
Patients with epispadias are typically young males. The symptoms, features, and clinical findings associated with epispadias include urinary incontinence, and abnormal position of urethral opening on examination.
How is Epispadias Diagnosed?
Epispadias is diagnosed through physical examination.
How is Epispadias Treated?
Epispadias is treated by surgical intervention.
What is the Prognosis of Epispadias?
The prognosis of epispadias is good with surgical intervention, although nocturnal incontinence may persist.
What is Hypospadias?
Hypospadias is a birth defect where the urethra opens onto the ventral aspect of the penile shaft
What is the Pathology of Hypospadias?
The pathology of hypospadias is:
-Etiology: The cause of hypospadias is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to hypospadias is a ventral curvature chordee of the penis that is allied with the anomaly, believed to result from developmental discrepancy amid the usual dorsal muscle of the corporal bodies and the weakened ventral urethra and related muscles.
-Morphology: The morphology associated with hypospadias shows a urethra that opens onto the ventral aspect of the penile shaft.
How does Hypospadias Present?
Patients with hypospadias are typically young male infants. The symptoms, features, and clinical findings associated with hypospadias include the abnormal position of the urethral orifice on male genital examination.
How is Hypospadias Diagnosed?
Hypospadias is diagnosed through physical examination.
How is Hypospadias Treated?
Hypospadias is treated by surgical repair.
What is the Prognosis of Hypospadias?
The prognosis of hypospadias is good.
What is Phimosis?
Phimosis is a condition in which the prepuce is too small and tight to permit its usual retraction over the glans
What is the Pathology of Phimosis?
The pathology of phimosis is:
-Etiology: The cause of phimosis is congenital or acquired through inflammation, trauma, or edema of the prepuce.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to phimosis is a buried penis caused by a developmental irregularity in which dartos fascia does not develop into the typical elastic outline.
-Morphology: The morphology associated with phimosis shows an unelastic foreskin.
How does Phimosis Present?
Patients with phimosis are typically young males. The symptoms, features, and clinical findings associated with phimosis include failure to retract the prepuce.
How is Phimosis Diagnosed?
Phimosis is diagnosed through a medical history and physical examination
How is Phimosis Treated?
Phimosis is treated through surgical intervention, which may include an emergent circumcision in case of paraphimosis.
What is the Prognosis of Phimosis?
The prognosis of phimosis is good with proper surgical care.
What is Inflammation of the Penis?
Inflammation of the penis is a condition of the penis prepuce or glans characterized by redness, heat, pain swelling secondary to specific and nonspecific infections including trauma.
What is Balanoposthitis?
Balanoposthitis is a condition of non-specific inflammation of the inner surface of the prepuce and the nearby surface of the glans.
What is the Pathology of Balanoposthitis?
The pathology of balanoposthitis is:
-Etiology: The cause of balanoposthitis is a microorganisms that include bacteria, gardnerella, and candida albicans.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to balanoposthitis include moisture trapped inside the preputial environment, that encourages microbial proliferation. This triggers an inflammatory response.
-Morphology: The morphology associated with balanoposthitis shows inflammation.
-Histology: The histology associated with balanoposthitis shows microorganisms and immune cells.
How does Balanoposthitis Present?
Patients with balanoposthitis are typically males. The symptoms, features, and clinical findings associated with balanoposthitis include red, humid macular lesions on examination of the prepuce and the glans. Penile discomfort, pruritus, discharge, ulceration, and deep erosion in case of the advanced condition.
How is Balanoposthitis Diagnosed?
Balanoposthitis is diagnosed through history, physical examination, lesion cultures, swab (nucleic acid amplification test (NAAT)) to check gonorrhea and chlamydia presence.
How is Balanoposthitis Treated?
Balanoposthitis is treated through, supportive care (hygiene care), and medical care.
What is the Prognosis of Balanoposthitis?
The prognosis of balanoposthitis is good with effective support and treatment.
What are Tumors of the Penis?
Tumors of the penis are neoplasms lesions on the penis that are malignant or benign in origin.
Examples of tumors of the penis include:
- Condyloma acuminatum
- Peyronie disease
- Carcinoma in situ of the penis
- Bowen disease of the penis
- Bowenoid papulosis of the penis
- Squamous cell carcinoma of the penis
What is Condyloma Acuminatum?
Condyloma acuminatum is a benign tumor caused by human papillomavirus (HPV) types 6 and 11.
What is the Pathology of Condyloma Acuminatum?
The pathology of condyloma acuminatum is:
-Etiology: The cause of condyloma acuminatum is human papillomavirus types 6 and 11.
-Genes involved: p63
-Pathogenesis: The sequence of events that lead to condyloma acuminatum invading of the basal epidermal cells layer by HPV. These cause mucosal microabrasions. No signs and symptoms at the latent viral phase. The making of viral DNA, particles, and capsids begin. Epidermal cells infected and mature the morphologic uncharacteristic koilocytosis of condyloma acuminatum.
-Morphology: The morphology associated with condyloma acuminatum shows single or numerous stalkless or pedunculated, red papillary carbuncles varying from 1 mm to several millimeters in diameter.
-Histology: The histology associated with condyloma acuminatum shows papillary villi with connective tissue stroma enclosed by squamous epithelium that displays hyperkeratosis, parakeratosis, and hyperplasia of the prickle cell layer.
How does Condyloma Acuminatum Present?
Patients with condyloma acuminatum typically affect both genders present at an age range of 20-24 years. The symptoms, features, and clinical findings associated with condyloma acuminatum include pruritus, painless bumps, discharge, or multiple lesions.
How is Condyloma Acuminatum Diagnosed?
Condyloma acuminatum is diagnosed through laboratory studies, physical exam, and biopsy. Pap smears may check for papillomatosis, and acetowhitening will show a shiny white snowy appearance.
How is Condyloma Acuminatum Treated?
Condyloma acuminatum is treated through treatment routines and follow-up care. Cryotherapy, Curettage, Surgical excision. Carbon dioxide laser action for widespread and recurring condyloma acuminatum.
What is the Prognosis of Condyloma Acuminatum?
The prognosis of condyloma acuminatum is poor as it either fail to respond to management or reappears after a response.
What is Peyronie Disease?
Peyronie disease is the condition of the penis characterized by curvature on the penile shaft.
What is the Pathology of Peyronie Disease?
The pathology of Peyronie disease is:
-Etiology: The cause of Peyronie disease is associated with beta-blocking agents, lack of vitamin E, and increased serotonin levels.
-Genes involved: HLA-B7 surface antigen.
-Pathogenesis: The sequence of events that lead to Peyronie disease include trauma which results in ventral and dorsal delamination damage to the tunica albuginea. Augmented collagen is deposition at tunica albuginea, resulting in fibrosis.
-Morphology: The morphology associated with Peyronie disease shows penile shaft curvature.
-Histology: The histology associated with Peyronie disease shows collagen deposition and abnormal elastic fibers.
How does Peyronie Disease Present?
Patients with Peyronie disease are typically older males. The symptoms, features, and clinical findings associated with Peyronie disease include palpable plaque, indented shaft, penile pain, and erectile dysfunction.
How is Peyronie Disease Diagnosed?
Peyronie disease is diagnosed through physical exam, imaging such as penile ultrasonography, corpus cavernosography, and MRI.
How is Peyronie Disease Treated?
Peyronie disease is treated through surgical repair.
What is the Prognosis of Peyronie Disease?
The prognosis of Peyronie disease is good surgical intervention and postoperative care.
What is Carcinoma in Situ of the Penis?
Carcinoma in situ of the penis is an epithelial lesion of the penis where the cytologic deviations of malignancy are only confined to the penis epithelium, with no indication of distant metastases.
What is the Pathology of Carcinoma in Situ of The Penis?
The pathology of carcinoma in situ of the penis is:
-Etiology: The cause of carcinoma in situ of the penis includes HPV.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to carcinoma in situ of the penis, trivial grazes on the prepuce or glans, progressively grow slowly edgewise along the surface, covering the full glans and prepuce, and finally invading the penile corpora and shaft.
-Morphology: The morphology associated with carcinoma in situ of the penis shows that it starts on the glans or else the inner prepuce surface close the coronal sulcus.
-Histology: The histology associated with carcinoma in situ of the penis shows the formation of keratinized, epithelial pearl, and degrees of mitotic action.
How does Carcinoma In Situ Of The Penis Present?
Patients with carcinoma in situ of the penis are typically infrequent in circumcised males, present at an age range of 60 years and above. The symptoms, features, and clinical findings associated with carcinoma in situ of the penis include grazing that has failed to restore, delicate sclerosis of skin, minor carbuncle, papule, a boil, a wartlike growth, large exophytic growing, or inflamed glans.
How is Carcinoma In situ Of The Penis Diagnosed?
Carcinoma in situ of the penis is diagnosed by physical examination and biopsy. Ultrasonography for local cancer staging, and CT scanning may be needed to assess retroperitoneal and pelvic lymph nodes.
How is Carcinoma In Situ Of The Penis Treated?
Carcinoma in situ of the penis is treated through local excision.
What is the Prognosis of Carcinoma In Situ Of The Penis?
The prognosis of carcinoma in situ of the penis is good with early diagnosis and treatment, the survival rate for a precise stage of penile cancer is about 65% in 5 years.
What is Bowen Disease of the Penis?
Bowen disease of the penis is penile in situ squamous cell carcinoma.
What is the Pathology of Bowen Disease of The Penis?
The pathology of Bowen disease of the penis is:
-Etiology: The cause of Bowen disease of the penis is may be related to uncircumcised, immunosuppression, balanitis, smoking, HPV 8 and 16, lichen planus.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to Bowen disease of the penis trivial grazes on the prepuce or glans, progressively grow slowly edgewise along the surface, covering the full glans, and finally may invade the penile corpora and shaft.
-Morphology: The morphology associated with Bowen disease of the penis shows red papules and plaques glans.
-Histology: The histology associated with Bowen disease of the penis shows parakeratosis, dyskeratosis, epidermal acanthosis, and epidermal atypia.
How does Bowen Disease of The Penis Present?
Patients with Bowen disease of the penis typically males that present at an age range of 20-80 years. The symptoms, features, and clinical findings associated with Bowen disease of the penis include pain, scaling, dysuria, itching, ulceration, bleeding, red papules, and plaques.
How is Bowen Disease of The Penis Diagnosed?
Bowen disease of the penis is diagnosed through biopsy and histological examination.
How is Bowen Disease of The Penis Treated?
Bowen disease of the penis is treated topical imiquimod of 5-fluorouracil.
What is the Prognosis of Bowen Disease of The Penis?
The prognosis of Bowen disease of the penis is fair if acknowledged and managed early.
What is Bowenoid papulosis of the penis?
Bowenoid papulosis of the penis is a lesion established as papules, established as papules with and establish distinctive histopathology
What is the Pathology of Bowenoid Papulosis of The Penis?
The pathology of Bowenoid papulosis of the penis is:
-Etiology: The cause of Bowenoid papulosis of the penis is human papillomavirus (HPV) type 16.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to Bowenoid papulosis of the penis usually appear as a papule or multiple papules after asymptomatic pivotal epidermal dysplasia and hyperplasia persuaded by HPV contagion.
-Morphology: The morphology associated with Bowenoid papulosis of the penis shows penile intraepithelial neoplasia.
-Histology: The histology associated with Bowenoid papulosis of the penis shows full-thickness epidermal atypia, dyskeratotic cells, and atypical mitoses.
How does Bowenoid Papulosis of The Penis Present?
Patients with Bowenoid papulosis of the penis typically affect both genders equally, present at an age range of 31 years. The symptoms, features, and clinical findings associated with Bowenoid papulosis of the penis include inflamed pruritic lesions.
How is Bowenoid Papulosis of The Penis Diagnosed?
Bowenoid papulosis of the penis is diagnosed through biopsy. HPV subtyping may be needed.
How is Bowenoid Papulosis of The Penis Treated?
Bowenoid papulosis of the penis is treated through destructive or ablative therapies, 5 fluorouracil (5FU), carbon dioxide laser vaporization, electrocoagulation, cryotherapy, 5-aminolevulinic acid-mediated photodynamic therapy (ALA-PDT), and excisional surgery.
What is Squamous Cell Carcinoma of the Penis?
Squamous cell carcinoma of the penis is a lesion that usually begins on the glans or inner surface of the prepuce near the coronal sulcus.
What is the Pathology of Squamous Cell Carcinoma of the Penis?
The pathology of squamous cell carcinoma of the penis is:
-Etiology: The cause of squamous cell carcinoma of the penis is malignant keratinocytes.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to squamous cell carcinoma of the penis involves growth of malignant keratinocytes.
-Morphology: The morphology associated with squamous cell carcinoma of the penis shows a squamous lesion.
-Histology: The histology associated with squamous cell carcinoma of the penis shows dyskeratosis, epidermal acanthosis, parakeratosis, and epidermal atypia.
How does Squamous Cell Carcinoma Of The Penis Present?
Patients with squamous cell carcinoma of the penis typically have nodular lesions. The symptoms, features, and clinical findings associated with squamous cell carcinoma of the penis include visible skin lesions.
How is Squamous Cell Carcinoma Of The Penis Diagnosed?
Squamous cell carcinoma of the penis is diagnosed by physical exam and biopsy.
How is Squamous Cell Carcinoma Of The Penis Treated?
Squamous cell carcinoma of the penis is treated through medical therapy, radiation therapy, and surgery, and laser therapy.
What is the Prognosis of Squamous Cell Carcinoma of the Penis?
The prognosis of squamous cell carcinoma of the penis is fair depending on staging and management.
What are Congenital Anomalies of the Testis or Epididymis?
Congenital anomalies of the testis or epididymis include:
- Cryptorchidism
What is Cryptorchidism?
Cryptorchidism is an anomaly with undescended testes.
What is the Pathology of Cryptorchidism?
The pathology of cryptorchidism:
-Etiology: The cause of cryptorchidism is multifactorial, premature birth, familiar history, endocrine-disrupting chemical exposure, abnormalities in the gubernaculum.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to cryptorchidism. Descending process incomplete, in the situation of true undescended testis, trails to an anomalous position in ectopic testis, androgen insensitivity disorder/hormonal causes in bilateral cryptorchidism.
-Morphology: The morphology associated with cryptorchidism shows it is unilateral in most cases, bilateral in 25% of patients.
-Histology: The histology associated with testicular atrophy shows marked hyalinization and thickening of the basement membrane of the spermatic tubules.
How does Cryptorchidism Present?
Patients with cryptorchidism typically affect male infants present at an age range of 2 years and below. The symptoms, features, and clinical findings associated with cryptorchidism include no palpable testis/empty scrotum on examination. Palpable testes may be undescended, retractile, or ectopic.
How is Cryptorchidism Diagnosed?
Cryptorchidism is diagnosed through physical examination and imaging studies.
How is Cryptorchidism Treated?
Cryptorchidism is treated through hormonal therapy, and orchidopexy.
What is the Prognosis of Cryptorchidism?
The prognosis of cryptorchidism is good following treatment.
What are Regressive Changes of the Testis or Epididymis?
Regressive changes of the testis or epididymis are abnormal development to the testis or epididymis, congenital or acquired.
Regressive changes of the testis or epididymis include:
- Testicular atrophy
- Decreased fertility
What is Testicular Atrophy?
Testicular atrophy is a regressive alteration affecting the scrotal testis, shrinking of the testis.
What is the Pathology of Testicular Atrophy?
The pathology of testicular atrophy is the gross and microscopic study of the structure and functional changes in testicular atrophy.
-Etiology: The cause of testicular atrophy is multifactorial including hypopituitarism, atherosclerotic tapering of the blood supply, cachexia, exhaustion atrophy, orchitis.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to testicular atrophy are of multifactorial origin, inflammations, diet, underlying disease, congenital anomalies among others.
-Morphology: The morphology associated with testicular atrophy shows it is unilateral in most cases, bilateral in 25% of patients.
-Histology: The histology associated with testicular atrophy shows marked hyalinization and thickening of the basement membrane of the spermatic tubules.
How does Testicular Atrophy Present?
Patients with testicular atrophy typically affect males present at age range of 45 years. The symptoms, features, and clinical findings associated with testicular atrophy include smaller than normal testis, Leydig cell hyperplasia, history or presence of cryptorchidism.
How is Testicular Atrophy Diagnosed?
Testicular atrophy is diagnosed through physical examination. Imaging study may show abdominal, pelvic ultrasonography.
How is Testicular Atrophy Treated?
Testicular atrophy is treated by hormonal therapy.
What is the Prognosis of Testicular Atrophy?
The prognosis of testicular atrophy is fair with proper management..
What is Decreased Fertility?
Decreased fertility is a condition characterized by reduced reproduction ability.
What is the Pathology of Decreased Fertility?
The pathology of decreased fertility is:
-Etiology: The cause of decreased fertility is categorized into three groups which include pre-testicular causes, testicular causes, and post-testicular causes.
-Genes involved: CFTR.
-Pathogenesis: The sequence of events that lead to decreased fertility are testicular causes, total absence of the testes, cryptorchidism related issues, failure of spermatogenesis, Klinefelter’s syndrome, and mumps.
-Morphology: The morphology associated with decreased fertility shows atrophy of testis.
-Histology: The histology associated with decreased fertility shows marked hyalinization and thickening of the basement membrane of the spermatic tubules.
How does Decreased Fertility Present?
Patients with decreased fertility have trouble procreating, i.e fertilizing an egg. The symptoms, features, and clinical findings associated with decreased fertility include history of inability to sire in male, erectile dysfunction, and low sperm count.
How is Decreased Fertility Diagnosed?
Decreased fertility is diagnosed through medical history and physical examination. Laboratory studies such as semen analysis, and hormonal analysis may be useful. Imaging studies such as transrectal ultrasonography, scrotal ultrasonography, vasography to determine ductal system patency may help determine the underlying cause.
How is Decreased Fertility Treated?
Decreased fertility is treated with psychological and medical care that may include hormonal replacement and semen processing. Lifestyle changes and dietary supplements may be helpful.
What is the Prognosis of Decreased Fertility?
The prognosis of decreased fertility is fair with proper management.
What is Inflammation of the Testis or Epididymis?
Inflammation of the testis or epididymis is a medical condition characterized by pain, swelling, redness and hotness, and sometimes loss of function of the testis.
Examples of inflammation of the testis or epididymis includes:
- Inflammation of the testis or epididymis due to gonorrhea
- Inflammation of the testis or epididymis due to syphilis
- Inflammation of the testis or epididymis due to mumps
- Inflammation of the testis or epididymis due to tuberculosis
- Autoimmune orchitis aka granulomatous orchitis
- Nonspecific epididymitis
- Nonspecific orchitis
| Type of inflammation &Cause | Presentation | Diagnosis | Treatment | Prognosis |
| Gonorrhea | Development of frank abscesses in the epididymis, resulting in extensive destruction of this organ | Inflammation of the Testis or Epididymis diagnosed through medical history and examination. Laboratory studies-complete blood count, Imaging studies- scrotal ultrasonography | Inflammation of the Testis or Epididymis treated through medical care treating underlying causes, Surgical incision | Inflammation of the Testis or Epididymis prognosis is good with proper treatment of the underlying cause. |
| Syphilis | The morphologic pattern takes two forms: a diffuse interstitial inflammation branded by edema, and plasma cell and lymphocytic penetration with the typical hallmark of all syphilitic contagions | |||
| Mumps | Interstitial orchitis progresses 1 week after start of swelling to the parotid glands | |||
| Tuberculosis | Raises the classic morphological responses of caseating granulomatous inflammation that are distinctive of tuberculosis illness. | |||
| Autoimmune Orchitis aka Granulomatous Orchitis | A painless testicular mass imitating a testicular tumor. Histologically, the orchitis is illustrious by granulomas seen confined in spermatic tubules. | |||
| Nonspecific Epididymitis & Nonspecific Orchitis caused by sexually transmitted pathogens Chlamydia trachomatis and Neisseria gonorrhoeae | Infection limited to the interstitial connective tissue, extends involving the tubules and progress to free abscess formation or whole suppurative necrosis of the epididymis. The infection extends into the testis |
What are Vascular Disorders of the Testis or Epididymis?
Vascular disorders of the testis or epididymis are pathologies of the vessels supplying and draining blood to and from the testis or epididymis.
Examples of vascular disorders of the testis or epididymis include:
- Neonatal testicular torsion
- Testicular torsion
What is Neonatal Testicular Torsion?
Neonatal testicular torsion is an acute vascular occasion where the spermatic cord is twisted on its axis with substantial tenderness and swelling of an earlier normal testicle either in utero or shortly after birth.
What is the Pathology of Neonatal Testicular Torsion?
The pathology of neonatal testicular torsion is:
-Etiology: The cause of neonatal testicular torsion is not reliably identified. Factors associated with neonatal testicular torsion include anatomic abnormalities and adhesions.
-Genes involved: NA
-Pathogenesis: The sequence of events that lead to neonatal testicular torsion, tunica vaginalis, and epididymis twist on the spermatic cord, ischemic fluctuations swelling, infarction, and necrosis may occur. This may progress to gangrene to the testis.
-Morphology: The morphology associated with neonatal testicular torsion shows ranges from strong congestion to extensive eructation of blood into the interstitial tissue of the epididymis and testis in general and hemorrhagic infarction.
-Histology: The histology associated with neonatal testicular torsion show necrotic or ischemic tissue.
How does Neonatal Testicular Torsion Present?
Patients with neonatal testicular torsion are typically male neonates. The symptoms, features, and clinical findings associated with neonatal testicular torsion include neonate irritability, firm, non-tender testis, scrotal edema, and swelling.
How is Neonatal Testicular Torsion Diagnosed?
Neonatal testicular torsion is diagnosed through examination, and doppler ultrasonography.
How is Neonatal Testicular Torsion Treated?
Neonatal testicular torsion is treated through manual detorsion, or emergency surgical intervention if need be.
What is the Prognosis of Neonatal Testicular Torsion?
The prognosis of neonatal testicular torsion is fair depending on the age and time-lapsed.
What is Testicular Torsion?
Testicular torsion is the winding of the spermatic cord that results in decreased venous drainage and arterial blood supply to the testis.
What is the Pathology of Testicular Torsion?
The pathology of testicular torsion is:
-Etiology: The cause of testicular torsion may include anatomic defects, or spinning of the spermatic cord.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to testicular torsioninvolves twisting of the spermatic cord. This may lead to ischemic fluctuations, swelling, infarction, and necrosis, or eventually gangrene.
-Morphology: The morphology associated with testicular torsion shows ranges from strong congestion to extensive eructation of blood into the interstitial tissue of the epididymis and testis in general, and hemorrhagic infarction.
-Histology: The histology associated with testicular torsion shows signs of ischemia and or necrosis.
How does Testicular Torsion Present?
Patients with testicular torsion are typically male present at an age range of 13-21 years old. The symptoms, features, and clinical findings associated with testicular torsion include painful urination, nausea and vomiting firm, non-tender testis in neonates, scrotal edema, testicular swelling, pain, and crotal discoloration.
How is Testicular Torsion Diagnosed?
Testicular torsion is diagnosed through examination, and doppler ultrasonography.
How is Testicular Torsion Treated?
Testicular torsion is treated by urgent manual detorsion or surgical methods.
What is the Prognosis of Testicular Torsion?
The prognosis of testicular torsion is fair depending on the age and time-lapsed.
What are Spermatic Cord and Paratesticular Tumors?
Spermatic cord and paratesticular tumors are urologic tumors that affect spermatic cord and testicular tissues.
Examples of spermatic cord and paratesticular tumors include:
- Lipomas
- Adenomatoid tumors
What are Lipomas?
Lipomas are slow-growing, benign fatty growths.
What is the Pathology of Lipomas?
The pathology of lipomas is:
-Etiology: The cause of lipomas is unclear, nonetheless may imitate growth of local pluripotent cells into adipocyte lines.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to lipomas involve adipocyte cell overproduction.
-Morphology: The morphology associated with lipomas shows fatty lesion on spermatic cord in this instance.
-Histology: The histology associated with lipomas shows benign adipose tissue comprising the entirety of the lesion.
How do Lipomas Present?
Patients with lipomas typically present at age range of 18 years and above. The symptoms, features, and clinical findings associated with lipomas include pain tender, and soft bulging mass.
How are Lipomas Diagnosed?
Lipomas is diagnosed through clinical examination, imaging studies, and biopsy.
How are Lipomas Treated?
Lipomas are treated by surgical intervention.
What is the Prognosis of Lipomas?
The prognosis of lipomas is fair after surgical interventions.
What are Adenomatoid Tumors?
Adenomatoid tumors are neoplasm benign of mesothelial sources found more frequently in the male adnexa.
What is the Pathology of Adenomatoid Tumors?
The pathology of adenomatoid tumors is:
-Etiology: The cause of adenomatoid tumors is neoplastic mesothelial cells.
-Genes involved: TRAF7 gene
-Pathogenesis: The sequence of events that lead to adenomatoid tumors not well identified.
-Morphology: The morphology associated with adenomatoid tumors shows trivial, solid, hard, grayish-white, and poorly to well-bounded masses.
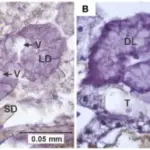
-Histology: The histology associated with adenomatoid tumors shows eosinophilic mesothelial cells at the cords and tubules looking like endothelium in origin.
How does Adenomatoid Tumors Present?
Patients with adenomatoid tumors are typically males that present in the age range of 30 to 50 years old. The symptoms, features, and clinical findings associated with adenomatoid tumors include painful palpable masses.
How are Adenomatoid Tumors Diagnosed?
Adenomatoid tumors are diagnosed through serum tumor markers and biopsy. Imaging studies such as ultrasonography may be helpful to visualize the lesion.
How are Adenomatoid Tumors Treated?
Adenomatoid tumors are treated through surgical excision.
What is the Prognosis of Adenomatoid Tumors?
The prognosis of adenomatoid tumors is good. The tumor is not known to recur or show malignant deterioration.
What are Testicular Tumors?
Testicular tumors are lesions of testis divided into two major classes: germ cell tumors and nongerminal tumors.
Examples of testicular tumors include:
- Testicular lymphoma
- Gonadoblastoma
- Tumors of sex cord-gonadal stroma
- Germ cell tumors
What is Testicular Lymphoma?
Testicular lymphoma is a rare and lethal type of non-Hodgkin lymphoma that accounts for approximately 5% of testicular tumors. These are not thought to originate from the testes, but rather are hematopoietic in origin. For more information refer to lymphomas.
What is Gonadoblastoma?
Gonadoblastoma is a rare neoplasm comprising a blend of gonadal stromal and germ cells elements, that arise in dysgenetic gonads.
What is the Pathology of Gonadoblastoma?
The pathology of gonadoblastoma is:
-Etiology: The cause of gonadoblastoma is dysgenetic gonads, undescended testis, and genetic mutations.
-Genes: Testis-specific protein Y-encoded (TSPY)
-Pathogenesis: The sequence of events that lead to gonadoblastoma include dysgenesisthat results in germinal factor.
-Morphology: The morphology associated with gonadoblastoma shows the variable size, yellowish-white and soft.
-Histology: The histology associated with gonadoblastoma shows two principal cell types large germ cells resembling seminoma cells, and small cells resembling immature sertoli, leydig, and granulosa cells.
How does Gonadoblastoma Present?
Patients with gonadoblastoma are typically young males. The symptoms, features, and clinical findings associated with gonadoblastoma include the history of the atypical genitourinary structure, palpable abdominal mass, and undescended testis.
How is Gonadoblastoma Diagnosed?
Gonadoblastoma is diagnosed through serum electrolyte panel, endocrinologic evaluation, biopsy, and chromosome analysis.
How is Gonadoblastoma Treated?
Gonadoblastoma is treated through surgical interventions.
What is the Prognosis of Gonadoblastoma?
The prognosis of gonadoblastoma is good if the lesion is removed before the alteration to a malignant type.
What are Tumors of Sex Cord-Gonadal Stroma?
Tumors of sex cord-gonadal stroma are an assorted group of malignant or benign neoplasms, subclassified based on their presumed histogenesis and differentiation.
Tumors of sex cord-gonadal stroma include:
- Leydig cell tumors
- Sertoli cell tumors
What are Leydig Cell Tumors?
Leydig cell tumors are rare testicular growths of the gonadal interstitium that are hormonally active.
What is the Pathology of Leydig Cell Tumors?
The pathology of Leydig cell tumors is:
-Etiology: The cause of Leydig cell tumors is unknown.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to Leydig cell tumors is unknown though believed endocrine role donates the progress of these tumors.
-Morphology: The morphology associated with Leydig cell tumors shows small, well-demarcated, and lobulated nodules.
-Histology: The histology associated with Leydig cell tumors shows abundant eosinophilic cytoplasm and Reinke’s crystals.
How does Leydig Cell Tumors Present?
Patients with Leydig cell tumors are typically males that present within an age range of 20 to 50 years old. The symptoms, features, and clinical findings associated with Leydig cell tumors include non-tender profound testicular nodule, gynecomastia, erectile dysfunction, and infertility.
How are Leydig Cell Tumors Diagnosed?
Leydig cell tumors are diagnosed through urine studies, serum studies, and endocrinological tests. Biopsy is confirmatory.
How are Leydig Cell Tumors Treated?
Leydig cell tumors are treated through medical care, chemotherapy, and surgical resection.
What is the Prognosis of Leydig Cell Tumors?
The prognosis of Leydig cell tumors is good for those with benign types, and poor for those with malignant types.
What are Sertoli Cell Tumors?
Sertoli cell tumors are rare tumor derivatives of Sertoli cells, situated in seminiferous tubules, that support spermatogenesis.
What is the Pathology of Sertoli Cell Tumors?
The pathology of Sertoli cell tumors is:
-Etiology: The cause of Sertoli cell tumors is unknown
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to Sertoli cell tumors unknown
-Morphology: The morphology associated with Sertoli cell tumors shows firm, small nodules with a standardized gray-white to the yellow cut surface.
-Histology: The histology associated with Sertoli cell tumors shows lesion cells are arranged in typical trabeculae with an inclination to form cordlike structures like undeveloped seminiferous tubules.
How does Sertoli Cell Tumors Present?
Patients with Sertoli cell tumors are typically males that present within an age range of 16 to 45 years old. The symptoms, features, and clinical findings associated with Sertoli cell tumors include testicular mass, impotence, and gynecomastia.
How is Sertoli Cell Tumors Diagnosed?
Sertoli cell tumors is diagnosed by laboratory testing and biopsy.
How is Sertoli Cell Tumors Treated?
Sertoli cell tumors is treated, through medical care, chemotherapy, and surgical resection.
What is the Prognosis of Sertoli Cell Tumors?
The prognosis of Sertoli cell tumors is good when diagnosed and treated while still benign.
What are Germ Cell Tumors?
Germ cell tumors are lesions of the testis that often produce enzymes and polypeptide hormones easily detected in the blood through sensitive assays.
Germ cell tumors include:
- Seminomas
- Spermatocytic seminoma
- Embryonal carcinoma
- Yolk sac tumors
- Choriocarcinoma
- Teratomas
- Mixed germ cell tumors
What are Seminomas?
Seminomas are malignancies accounting for around a 1/3 of all germ cell tumors.
What is the Pathology of Seminomas?
The pathology of seminomas is:
-Etiology: The cause of seminomas is not well identified, but seems to be associated with cryptorchidism.
-Genes involved: KIT
-Pathogenesis: The sequence of events that lead to seminomas originates from the germinal epithelium. Trapped gonocyte maturation results in the propagation of undeveloped spermatogonia. This causes increased genomic volatility.
-Morphology: The morphology associated with seminomas shows testis enlarged with normal contour, smaller tumor looks like circumscribed mass in the testis.
-Histology: The histology associated with seminomas shows tumor cells fairly even in size with clear cytoplasm and well-defined cell borders.
How does Seminomas Present?
Patients with seminomas typically affect middle-aged men between 30 to 50 years old. The symptoms, features, and clinical findings associated with seminomas include enlarged painless testis. Upsurge in hCG levels, and gynecomastia.
How are Seminomas Diagnosed?
Seminomas are diagnosed through laboratory studies such as AFP, B-HCG, and LDH. Imaging studies such as testicular ultrasonography, abdominal and pelvis CT scans may be useful. Biopsy is confirmatory.
How are Seminomas Treated?
Seminomas are treated through radical orchiectomy, radiation therapy, and chemotherapy.
What is the Prognosis of Seminomas?
The prognosis of seminomas is good with a survival rate >95% if diagnosed early while still confined in the testis.
What is Spermatocytic Seminoma?
Spermatocytic seminoma is a rare testicular germ cell tumor affecting mostly old men.
What is the Pathology of Spermatocytic Seminoma?
The pathology of spermatocytic seminoma is:
-Etiology: The cause of spermatocytic seminoma is unknown
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to spermatocytic seminoma is not well known,
-Morphology: The morphology associated with spermatocytic seminoma shows homogeneous, higher, softer, and more yellow in color and gelatinous than the classic seminoma
-Histology: The histology associated with spermatocytic seminoma shows a significantly in size from lymphocyte-like to huge mononucleate or multinucleate giant cells. Malignant cells contain eosinophilic cytoplasm that lacks glycogen.
How does Spermatocytic Seminoma Present?
Patients with spermatocytic seminoma typically affect old males present at an age range of 50 to 70 years. The symptoms, features, and clinical findings associated with spermatocytic seminoma include unilateral, painless and gradually widening testicular mass.
How is Spermatocytic Seminoma Diagnosed?
Spermatocytic seminoma is diagnosed through imaging studies such as testicular ultrasonography, and biopsy.
How is Spermatocytic Seminoma Treated?
Spermatocytic seminoma is treated through radical orchiectomy
What is the Prognosis of Spermatocytic Seminoma?
The prognosis of spermatocytic seminoma is good if treated while confined to the testes.
What is Embryonal Carcinoma?
Embryonal carcinoma is a germ cell neoplasm categorized with primitive epithelial cells with patent pleomorphism and several histologic patterns.
What is the Pathology of Embryonal Carcinoma?
The pathology of embryonal carcinoma is:
-Etiology: The cause of embryonal carcinoma is genetic, environmental factors, and idiopathic.
-Genes involved: embryonal carcinoma-specific gene DNMT3B.
-Pathogenesis: The sequence of events that lead to embryonal carcinoma unknown.
-Morphology: The morphology associated with embryonal carcinoma shows smaller tumor does not replace the whole testis, mass pied, are poorly demarcated at the margins, and scattered by hemorrhage and necrosis.
-Histology: The histology associated with embryonal carcinoma shows basally located nuclei and apical cytoplasm in teratomas, epithelial appearance, and are large and anaplastic neoplastic cells.
How does Embryonal Carcinoma Present?
Patients with embryonal carcinoma are typically males between 20 to 30 years old. The symptoms, features, and clinical findings associated with embryonal carcinoma include a painless palpable mass on the testis.
How is Embryonal Carcinoma Diagnosed?
Embryonal carcinoma is diagnosed through imaging studies, and biopsy.
How is Embryonal Carcinoma Treated?
Embryonal carcinoma is treated through surgical interventions and chemotherapy.
What is the Prognosis of Embryonal Carcinoma?
The prognosis of embryonal carcinoma is fair.
What are Yolk Sac Tumors?
Yolk sac tumors are common testicular tumors affecting infants and young children.
What is the Pathology of Yolk Sac Tumors?
The pathology of yolk sac tumors is:
-Etiology: The cause of yolk sac tumors is unknown.
-Genes involved: RUNX3 gene and GATA-4.
-Pathogenesis: The sequence of events that lead to yolk sac tumors is unknown.
-Morphology: The morphology associated with yolk sac tumors shows a soft mass that is generally yellow-white, with mucoid areas and areas of necrosis and hemorrhages.
-Histology: The histology associated with yolk sac tumors shows Schiller-duvall bodies.
How does Yolk Sac Tumors Present?
Patients with yolk sac tumors are typically young males. The symptoms, features, and clinical findings associated with yolk sac tumors include painless testicular lumps.
How are Yolk Sac Tumors Diagnosed?
Yolk sac tumors are diagnosed through laboratory studies such as AFP, B-HCG, and LDH. Biopsy is confirmatory.
How is Yolk Sac Tumors Treated?
Yolk sac tumors are treated through surgical treatment and adjuvant chemotherapy.
What is the Prognosis of Yolk Sac Tumors?
The prognosis of yolk sac tumors is good, with a survival rate greater than 90%.
What is Choriocarcinoma?
Choriocarcinoma is a histologic category of non-seminomatous germ cell lesions, together with testicular seminoma establishes deuce major histologic clusters of testicular tumors.
What is the Pathology of Choriocarcinoma?
The pathology of choriocarcinoma is:
-Etiology: The cause of choriocarcinoma is genetic changes, exposure to maternal estrogen, testicular trauma, and mumps.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to choriocarcinoma include a history of cryptorchidism. Genetic disparities in form of amplification and deletions are allied to the invasive advance of seminomas and nonseminomas.
-Morphology: The morphology associated with choriocarcinoma shows a small soft hemorrhagic necrotic mass.
-Histology: The histology associated with choriocarcinoma shows tumors containing two cell types, the syncytiotrophoblastic cell, and cytotrophoblastic cells.
How does Choriocarcinoma Present?
Patients with choriocarcinoma typically affect males and present at the age range of 15-35 years. The symptoms, features, and clinical findings associated with choriocarcinoma include testicular pain, scrotal swelling, and a palpable testicular lump.
How is Choriocarcinoma Diagnosed?
Choriocarcinoma is diagnosed through laboratory studies alpha-fetoprotein test, beta-hCG test. Biopsy is confirmatory.
How is Choriocarcinoma Treated?
Choriocarcinoma is treated through chemotherapy, orchidectomy, and retroperitoneal lymph node dissection.
What is the Prognosis of Choriocarcinoma?
The prognosis of choriocarcinoma is poor due to it’s tendency to spread throught the blood stream.
What are Teratomas?
Teratomas are complex tumors having several cellular or organoid components suggestive of normal derivatives from more than one germ layer.
What is the Pathology of Teratomas?
The pathology of teratomas is:
-Etiology: The cause of teratomas is associated with prenatal risk factors such as low birth weight, cryptorchidism, and genetic predisposition.
-Genes involved: metalloproteinase MMP7 gene, anti-apoptotic EGR1 gene.
-Pathogenesis: The sequence of events that lead to teratomas; metamorphoses in the genes linked to membrane-membrane interface, matrix establishment, and remodeling enzymes.
-Morphology: The morphology associated with teratomas shows characteristic presence of hair, bones, teeth, cartilage, and cystic spaces.
-Histology: The histology associated with teratomas shows a heterogeneous, collection of distinguished cells or organoid structures.
How does Teratomas Present?
Patients with teratomas typically found in male children and young adults, present at an age range of 20 to 35 years. The symptoms, features, and clinical findings associated with teratomas include palpable masses.
How are Teratomas Diagnosed?
Teratomas are diagnosed through laboratory studies serological tests, serum tumor makers. Imaging studies retroperitoneal/abdominal ultrasound and CT scan, X-rays, and biopsies.
How is Teratomas Treated?
Teratomas are treated through medical care- cisplatin chemotherapy.
What is the Prognosis of Teratomas?
The prognosis of teratomas is fairly grounded on classification with a mortality rate of 10% of good, 30% of intermediate, and 60% of poor.
What are Mixed Germ Cell Tumors?
Mixed germ cell tumors are lesions containing more than one pure pattern.
What is the Pathology of Mixed Germ Cell Tumors?
The pathology of mixed germ cell tumors is:
-Etiology: The cause of mixed germ cell tumors is genetic, environmental factors, prenatal factors, idiopathic causes.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to mixed germ cell tumors, grows when a germ cell neoplasia in situ or a seminoma cell turns mutated.
-Morphology: The morphology associated with mixed germ cell tumors shows pied, areas of necrosis, and hemorrhage.
-Histology: The histology associated with mixed germ cell tumors shows histologic of other germ cell tumors.
How does Mixed Germ Cell Tumors Present?
Patients with mixed germ cell tumors typically affect males present at an age range of 20 to 60 years. The symptoms, features, and clinical findings associated with mixed germ cell tumors include those of germ cell tumors.
How are Mixed Germ Cell Tumors Diagnosed?
Mixed germ cell tumors are diagnosed through Laboratory studies such as detecting elevated β HCG, LDH, α fetoprotein, and biopsy.
How are Mixed Germ Cell Tumors Treated?
Mixed germ cell tumors are treated through surgery intervention and medical chemotherapy.
What is the Prognosis of Mixed Germ Cell Tumors?
The prognosis of mixed germ cell tumors is poor.
What are Lesions of Tunica Vaginalis?
Lesions of tunica vaginalis are lesions that develop as a result of/or being involved in tumors of the testis or epididymis.
An example of a lesion of tunica vaginalis includes:
- Hematocele
What is a Hematocele?
Hematocele is a condition characterized by the collection of blood in the tunica vaginalis.
What is the Pathology of Hematocele?
The pathology of hematocele is:
-Etiology: The cause of hematocele is associated with trauma to the testis, torsions, scrotal, bleeding diathesis, and rarely idiopathic issues.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to hematocele involves the collection of fluid (blood) in the tunica vaginalis typically after trauma.
-Morphology: The morphology associated with hematocele shows a blood-filled cavity, which may be calcified with time.
-Histology: The histology associated with hematocele shows unifying hemorrhage and fibrous capsule with or without calcifications.
How does Hematocele Present?
Patients with hematocele typically affect males present at the age range of 10 to 30 years old. The symptoms, features, and clinical findings associated with hematocele include acute onset of scrotal pain, firm, scrotal mass. Hematoceles may also be painless in idiopathic cases.
How is Hematocele Diagnosed?
Hematocele is diagnosed through history and examination. MRI or scrotal ultrasound may be useful.
How is Hematocele Treated?
Hematocele is treated through supportive care, medical care treating underlying causes, analgesics, antibiotics, and surgical interventions.
What is the Prognosis of Hematocele?
The prognosis of hematocele is good with early diagnosis and testis salvage from necrotizing.
What is Inflammation of the Prostate?
Inflammation of the prostate is a clinical condition known as prostatitis characterized by pain, swelling, and appearance of red in color of the prostate secondary to an infection.
Examples of inflammation of the prostate includes:
- Acute bacterial prostatitis
- Chronic bacterial prostatitis
- Chronic a-bacterial prostatitis
- Granulomatous prostatitis
What is Acute Bacterial Prostatitis?
Acute bacterial prostatitis is the sudden onset of inflammation of the prostate secondary to bacteria that cause urinary tract infections.
What is the Pathology of Acute Bacterial Prostatitis?
The pathology of acute bacterial prostatitis is:
-Etiology: The cause of acute bacterial prostatitis is the infection with gram-negative members Enterobacteriaceae.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to acute bacterial prostatitis organism reaching the prostate via lymphohematogenous routes, or infected urine flows into the prostatic and ejaculatory ducts, the organisms implants themselves in the prostate, attracts macrophages initiating inflammatory process.
-Morphology: The morphology associated with acute bacterial prostatitis shows swollen tense, and enlarged prostate. numerous abscesses and foci of necrosis on cut section.
-Histology: The histology associated with acute bacterial prostatitis shows diffuse acute inflammatory infiltrate, prostatic acini filled with neutrophilic exudate.
How does Acute Bacterial Prostatitis Present?
Patients with acute bacterial prostatitis are typically older males. The symptoms, features, and clinical findings associated with acute bacterial prostatitis include fever, chills, malaise, dysuria, perineal pain, urinary frequency, perineal tenderness, and urinary retention.
How is Acute Bacterial Prostatitis Diagnosed?
Acute bacterial prostatitis is diagnosed in laboratory studies which include urinalysis that shows leukocytes, positive urine culture, increased erum prostate-specific antigen levels (PSA). A biopsy may be obtained.
How is Acute Bacterial Prostatitis Treated?
Acute bacterial prostatitis is treated through medical care that includes antibiotic therapy. Surgical intervention for perineal aspiration of abscess may be indicated.
What is the Prognosis of Acute Bacterial Prostatitis?
The prognosis of acute bacterial prostatitis is good if treated early.
What is Chronic Bacterial Prostatitis?
Chronic bacterial prostatitis is the inflammation of the prostate due to recurrent attacks of acute bacterial prostatitis.
What is the Pathology of Chronic Bacterial Prostatitis?
The pathology of chronic bacterial prostatitis is:
-Etiology: The cause of chronic bacterial prostatitis is the recurrent urinary tract infections.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to chronic bacterial prostatitis follows that recurrent acute prostatitis.
-Morphology: The morphology associated with chronic bacterial prostatitis shows enlarged, fibrosis, and shrunken prostate.
-Histology: The histology associated with chronic bacterial prostatitis shows foci of lymphocytes, plasma cells, macrophages, and neutrophils within the prostatic substance.
How does Chronic Bacterial Prostatitis Present?
Patients with chronic bacterial prostatitis typically affect males present at the age range of 30 to 50 years old. The symptoms, features, and clinical findings associated with chronic bacterial prostatitis include hematuria, dysuria, malodorous urine, urinary retention, and urethral discharge.
How is Chronic Bacterial Prostatitis Diagnosed?
Chronic bacterial prostatitis is diagnosed with a history and physical examination.
How is Chronic Bacterial Prostatitis Treated?
Chronic bacterial prostatitis is treated through medical care which include antimicrobial therapy, alpha-blockers, and pain medication.
What is the Prognosis of Chronic Bacterial Prostatitis?
The prognosis of chronic bacterial prostatitis is fair.
What is Chronic Abacterial Prostatitis?
Chronic abacterial prostatitis is the inflammation of the prostate due to recurrent attacks of acute bacterial prostatitis with no history of urinary tract infections.
What is the Pathology of Chronic Abacterial Prostatitis?
The pathology of chronic abacterial prostatitis is:
-Etiology: The cause of chronic abacterial prostatitis is pathogens such as chlamydia trachomatis and ureaplasma urealyticum
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to chronic abacterial prostatitis is unknown.
-Morphology: The morphology associated with chronic abacterial prostatitis shows enlarged, fibrosis, and shrunken prostate.
-Histology: The histology associated with chronic abacterial prostatitis shows foci of lymphocytes, plasma cells, macrophages, and neutrophils within the prostatic substance.
How does Chronic ABacterial Prostatitis Present?
Patients with chronic abacterial prostatitis are typically older males. The symptoms, features, and clinical findings associated with chronic abacterial prostatitis include; hematuria, dysuria, malodorous urine, urinary urgency/ frequency, urinary retention, and urethral discharge.
How is Chronic Abacterial Prostatitis Diagnosed?
Chronic abacterial prostatitis is diagnosed through history and physical examination. Laboratory studies such as urinalysis may be useful to rule out oother conditions. .
How is Chronic Abacterial Prostatitis Treated?
Chronic abacterial prostatitis is treated through medical care- antimicrobial therapy, alpha-blockers, and pain medication. Surgical intervention- transurethral resection of the prostate and transurethral vaporization of the prostate.
What is the Prognosis of Chronic Abacterial Prostatitis?
The prognosis of chronic abacterial prostatitis is fair with treatment success rates of about 40%-75%. Common to relapses.
What is Granulomatous Prostatitis?
Granulomatous prostatitis is an inflammatory ailment of the prostate having granulomas presence as histologic features.
What is the Pathology of Granulomatous Prostatitis?
The pathology of granulomatous prostatitis is:
-Etiology: The cause of granulomatous prostatitis is microbes such as fungi bacteria, viruses, and parasites. obstruction to prostatic ducts and stillness of secretions, or BCG for treatment of bladder cancer.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to granulomatous prostatitis, blockage ducts, and stillness of secretions results in epithelial distraction leading to the seepage of bacterial toxins, cellular debris, and prostatic secretions, such as corpora amylacea, and semen, to the stroma.
-Morphology: The morphology associated with granulomatous prostatitis shows firm to the hard gland.
-Histology: The histology associated with granulomatous prostatitis shows the presence of macrophages, lymphocytes, plasma cells, and some multinucleate giant cells.
How does Granulomatous Prostatitis Present?
Patients with granulomatous prostatitis are typically males within the age range of 18 to 86 years old. The symptoms, features, and clinical findings associated with granulomatous prostatitis include a history of UTI, urinary frequency, TB infection, mild hematuria, and fever.
How is Granulomatous Prostatitis Diagnosed?
Granulomatous prostatitis is diagnosed through history and physical examination.
How is Granulomatous Prostatitis Treated?
Granulomatous prostatitis is treated through mainly supportive, temporary catheterization hot sitz baths, and fluids therapy. Treatment of concurrent infection when indicated.
What is Benign Enlargement of the Prostate?
Benign enlargement of the prostate is a non-neoplastic tumor like enlargement of the prostate common disorder in males and considered sometimes as a regular aging course.
Examples of benign enlargement of the prostate include:
- Benign prostatic hyperplasia
What is Benign Prostatic Hyperplasia?
Benign prostatic hyperplasia is an ailment of the prostate gland categorized by the propagation of the cellular essentials of the prostate, causing enlargement of the gland.
What is the Pathology of Benign Prostatic Hyperplasia?
The pathology of benign prostatic hyperplasia is:
-Etiology: The cause of benign prostatic hyperplasia is not fully established, though, factors such as endocrinologic, racial, inflammation, and arteriosclerosis are associated.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to benign prostatic hyperplasia related to the action of androgens such as dihydrotestosterone (DHT).
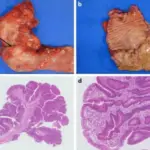
-Morphology: The morphology associated with benign prostatic hyperplasia shows nodular, smooth, and firm nodules.
-Histology: The histology associated with benign prostatic hyperplasia shows hyperplasia of glandular, fibrous, and muscular in varying proportions.
How does Benign Prostatic Hyperplasia Present?
Patients with benign prostatic hyperplasia typically affects older males. The symptoms, features, and clinical findings associated with benign prostatic hyperplasia include urinary tract symptoms, and hematuria.
How is Benign Prostatic Hyperplasia Diagnosed?
Benign prostatic hyperplasia is diagnosed through laboratory studies, dipstick, renal function tests, urinalysis, and prostate-specific antigen (PSA) tests.
How is Benign Prostatic Hyperplasia Treated?
Benign prostatic hyperplasia is treated through medical care which may include alpha-blockers, 5-alpha-reductase Inhibitors, combination therapy, and anticholinergic agents. Some cases may benefit from surgical intervention such as a transurethral resection of the prostate.
What is the Prognosis of Benign Prostatic Hyperplasia?
The prognosis of benign prostatic hyperplasia is good.
What are Tumors of the Prostate?
Tumors of the prostate are benign or malignant lesions on the prostate glands.
Examples of tumors of the prostate include:
- Prostate adenocarcinoma
- Ductal adenocarcinomas
What is Prostate Adenocarcinoma?
Prostate adenocarcinoma is epithelial cancer originating from prostate glandular tissue with excretory properties.
What is the Pathology of Prostate Adenocarcinoma?
The pathology of prostate adenocarcinoma is:
-Etiology: The cause of prostate adenocarcinoma is, family history, age, hormone level, race, and environmental factors
-Genes involved: PTEN gene deletion and ERG gene.
-Pathogenesis: The sequence of events that lead to prostate adenocarcinoma; Androgen acting in paracrine manner diffuse into neighboring epithelial cells, binds to nuclear androgen receptors, and motions transcription of mitogenic growth factors to the stromal cells and epithelial cells.
-Morphology: The morphology associated with prostate adenocarcinoma shows solid gray-white/ yellow areas, tumor grossly indiscernible.
-Histology: The histology associated with prostate adenocarcinoma shows large nuclei with prominent nucleoli, vague eosinophilic secretions, cytoplasmic tincture, crystalloids, and blue mucin lumen.
How does Prostate Adenocarcinoma Present?
Patients with prostate adenocarcinoma are typically older men. The symptoms, features, and clinical findings associated with prostate adenocarcinoma include urinary tract symptoms, and hematuria.
How is Prostate Adenocarcinoma Diagnosed?
Prostate adenocarcinoma is diagnosed through laboratory studies which may include prostate specific antigen test, and biopsy.
How is Prostate Adenocarcinoma Treated?
Prostate adenocarcinoma is treated by medical care and prostatectomy.
What is the Prognosis of Prostate Adenocarcinoma?
The prognosis of prostate adenocarcinoma is poor especially with Gleason score 6 and above, and stage III or high
What is Ductal Adenocarcinomas?
Ductal Adenocarcinomas is rare prostatic carcinoma constituting of pseudostratified columnar cells glands lining similar to endometrioid epithelium
What is the Pathology of Ductal Adenocarcinomas?
The pathology of ductal adenocarcinomas is The study of the structure and functional changes of the prostate ducts in presence of prostatic carcinoma constituting of pseudostratified columnar cells glands lining similar to the endometrioid epithelium.
-Etiology: The cause of ductal adenocarcinomas is unknown
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to ductal adenocarcinomas is unknown.
-Morphology: The morphology associated with ductal adenocarcinomas shows prostate enlargement and nodules.
-Histology: The histology associated with ductal adenocarcinomas shows abnormal prostatic glands that lose the characteristic two cell lining.
How does Ductal Adenocarcinomas Present?
Patients with ductal adenocarcinomas are typically older males. The symptoms, features, and clinical findings associated with ductal adenocarcinomas include urinary tract symptoms, and hematuria.
How are Ductal Adenocarcinomas Diagnosed?
Ductal adenocarcinomas are diagnosed through laboratory studies and biopsy.
How are Ductal Adenocarcinomas Treated?
Ductal adenocarcinomas are treated through radiation therapy, hormonal therapy, and surgery.
What is the Prognosis of Ductal Adenocarcinomas?
The prognosis of ductal adenocarcinomas is poor especially with Gleason score 6 and above, and stage III or high.