Muscle pathology is a disorder related to muscles.
What are Diseases of the Skeletal Muscle System?
Diseases of the skeletal muscle system are diseases that affect the skeletal muscles.
Diseases of the skeletal muscle system include:
- Skeletal muscle atrophy
- Neurogenic and myopathic changes in skeletal muscle
- Inflammatory myopathies
- Toxic myopathies
- Inherited disease of skeletal muscle
What is Skeletal Muscle Atrophy?
Skeletal muscle atrophy is a change that occurs in the muscles of an individual as a result of the conditions of disuse.
What is the Pathology of Skeletal Muscle Atrophy?
The pathology of skeletal muscle atrophy is:
-Etiology: The cause of skeletal muscle atrophy is lack of use.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to skeletal muscle atrophy includes protein degradation exceeding protein synthesis, leading to a reduction of the cross-sectional area of myofibers and decreased muscle strength.
-Morphology: The morphology associated with skeletal muscle atrophy shows a decreased cross-sectional area of muscle fibers, concomitant reduced whole muscle volume, and mass, but no decrease in the number of fibers.
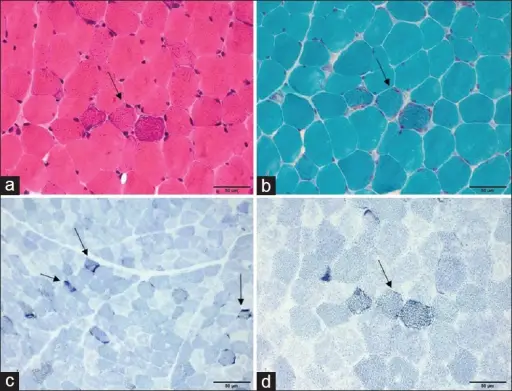
-Histology: The histology associated with skeletal muscle atrophy shows the reduction in myofiber diameter.
How does Skeletal Muscle Atrophy Present?
Patients with skeletal muscle atrophy typically affect males and females both present at the age range of 40-80 years. The symptoms, features, and clinical findings associated with skeletal muscle atrophy include balance problems, difficulty walking, and falls, difficulty with speaking and swallowing, facial weakness, gradual difficulty walking and speaking, memory loss, tingling or weakness of extremities, impaired balance, and coordination.
How is Skeletal Muscle Atrophy Diagnosed?
Skeletal muscle atrophy is diagnosed using physical exam, blood tests, and electromyogram.
How is Skeletal Muscle Atrophy Treated?
Skeletal muscle atrophy is treated with exercise, physical therapy, and ultrasonic therapy.
What is the Prognosis of Skeletal Muscle Atrophy?
The prognosis of skeletal muscle atrophy is typically good with a normal life expectancy.
What are Neurogenic and Myopathic Changes in Skeletal Muscle?
Neurogenic and myopathic changes in skeletal muscle are the disorders of skeletal muscles. Myopathic disorders are those that affect primarily the muscle while neurogenic disorders are caused by damage or disease of the motor neurons or peripheral nerves.
What are Inflammatory Myopathies?
Inflammatory myopathies are a group of diseases, with no known cause, that involves chronic muscle inflammation accompanied by muscle weakness.
What are Toxic Myopathies?
Toxic myopathies are a diverse group of muscle disorders caused by a variety of medications and toxins.
What is the Inherited Disease of Skeletal Muscle?
Inherited disease of skeletal muscle is progressive muscle disorder resulting from defects in one or more genes needed for normal muscle structure and function.
What are Skeletal Muscle Tumors?
Skeletal muscle tumors are the tumors that arise from the skeletal muscle.
Skeletal muscle tumors may be benign or malignant.
What are Benign Skeletal Muscle Tumors?
Benign skeletal muscle tumors are those tumors that stay in their primary location without invading other sites of the body.
Examples of benign skeletal muscle tumors include:
- Rhabdomyoma
What is Rhabdomyoma?
Rhabdomyoma is a benign tumor of striated muscle.
What is the Pathology of Rhabdomyoma?
The pathology of rhabdomyoma is:
-Etiology: The cause of rhabdomyoma is genetic modification during the development of striated muscle.
-Genes involved: TSC1, TSC2.
-Pathogenesis: The sequence of events that lead to rhabdomyoma involves mutations in the TSC1 and TSC2 genes.
-Morphology: The morphology associated with rhabdomyoma shows the presence of a mixture of spindle-shaped cells with indistinct cytoplasm and muscle fibers, which resemble striated muscle tissue.
-Histology: The histology associated with rhabdomyoma shows well-circumscribed, not encapsulated, sheets of large, well-differentiated skeletal muscle cells.
How does Rhabdomyoma Present?
Patients with rhabdomyoma typically affect males present at the age range of over 60 years. The symptoms, features, and clinical findings associated with rhabdomyoma include mass in the region of the neck, hoarseness, difficulty breathing, difficulty swallowing, or a combination.
How is Rhabdomyoma Diagnosed?
Rhabdomyoma is diagnosed using echocardiography.
How is Rhabdomyoma Treated?
Rhabdomyoma is treated with excision. Excision is curative but may recur if incompletely excised.
What is the Prognosis of Rhabdomyoma?
The prognosis of rhabdomyoma is good if there is no complication.
What are Malignant Skeletal Muscle Tumors?
Malignant skeletal muscle tumors are those tumors that grow uncontrollably and spread locally and/or to distant sites.
Malignant skeletal muscle tumors include:
- Rhabdomyosarcoma
What is Rhabdomyosarcoma?
Rhabdomyosarcoma is a mesenchymal aggressive malignant tumor of skeletal muscle differentiation. There are different types of rhabdomyosarcomas which include alveolar, embryonal, and pleomorphic.
What is the Pathology of Rhabdomyosarcoma?
The pathology of rhabdomyosarcoma is:
-Etiology: The cause of rhabdomyosarcoma is disruption of skeletal muscle progenitor cell growth and related differentiation.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to rhabdomyosarcoma is unclear.
-Morphology: The morphology associated with rhabdomyosarcoma shows small, round tumor cells with hyperchromatic nuclei and large, polygonal-shaped tumor cells with abundant eosinophilic cytoplasm, which often contains diagnostic cross striations.
-Histology: The histology associated with rhabdomyosarcoma shows sheets of small, round cells clustered with variable amounts of fibrous septa; may contain scattered giant cells (alveolar rhabdomyosarcoma.
How does Rhabdomyosarcoma Present?
Patients with rhabdomyosarcoma typically affect males present at the age range of 25 or less. The symptoms, features, and clinical findings associated with rhabdomyosarcoma include a persistent lump or swelling in the part of the body, bulging of the eye or a swollen eyelid, headache and nausea, trouble urinating or having bowel movements, blood in the urine, bleeding from the nose, throat, vagina, or rectum.
How is Rhabdomyosarcoma Diagnosed?
Rhabdomyosarcoma is diagnosed using ultrasound imaging.
How is Rhabdomyosarcoma Treated?
Rhabdomyosarcoma is treated with wide excision without axillary dissection, adjuvant or neoadjuvant radiation.
What is the Prognosis of Rhabdomyosarcoma?
The prognosis of rhabdomyosarcoma is poor.
What are Smooth Muscle Tumors?
Smooth muscle tumors are the tumors that arise from smooth muscles.
What are Benign Smooth Muscle Tumors?
Benign smooth muscle tumors are those tumors that stay in their primary location without invading other sites of the body.
Examples of benign smooth muscle tumors include:
- Leiomyoma
What is Leiomyoma?
Leiomyoma is the bland smooth muscle tumor without mitotic figures.
What is the Pathology of Leiomyoma?
The pathology of leiomyoma is:
-Etiology: The cause of leiomyoma is ischemia or hormonal stimulation.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to leiomyoma is not well understood.
-Morphology: The morphology associated with leiomyoma shows monotonous spindle cells with indistinct borders arranged in intersecting fascicles.
-Histology: The histology associated with leiomyoma shows bundles or fascicles of spindled cells with eosinophilic and possibly fibrillary cytoplasm.
How does Leiomyoma Present?
Patients with leiomyoma typically affect women present in the age range of 40 and above (postmenopausal). The symptoms, features, and clinical findings associated with leiomyoma include menorrhagia, pelvic pain, pelvic pressure, frequent urination, heavy menstrual bleeding, and difficulty emptying the bladder.
How is Leiomyoma Diagnosed?
Leiomyoma is diagnosed using ultrasound and MRI.
How is Leiomyoma Treated?
Leiomyoma is treated with hysterectomy or myomectomy.
What is the Prognosis of Leiomyoma?
The prognosis of leiomyoma is excellent as the patient remains asymptomatic for many years or indefinitely.
What are Malignant Smooth Muscle Tumors?
Malignant smooth muscle tumors are those tumors that grow uncontrollably and spread locally and/or to distant sites.
Examples of malignant muscle tumors include:
- Leiomyosarcoma
What is a Leiomyosarcoma?
Leiomyosarcoma is a rare tumor derived from smooth muscles. It has three types, conventional, epithelioid, and myxoid.
What is the Pathology of Leiomyosarcoma?
The pathology of leiomyosarcoma is:
-Etiology: The cause of leiomyosarcoma is unknown. However, genetic is considered one of the causes.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to leiomyosarcoma includes cytogenetic and molecular changes.
-Morphology: The morphology associated with leiomyosarcoma shows bulky, fleshy tumor invading into a myometrial wall or polypoid tumor projecting into the lumen.
-Histology: The histology associated with leiomyosarcoma shows severe atypia, increased mitoses, and tumor cell necrosis.
How does Leiomyosarcoma Present?
Patients with leiomyosarcoma typically affect females present at the age range of 40-69 years. The symptoms, features, and clinical findings associated with leiomyosarcoma include abnormal vaginal bleeding, lump or swelling under the skin, bloating and abdominal swelling.
How is Leiomyosarcoma Diagnosed?
Leiomyosarcoma is diagnosed using MRI and CT scans.
How is Leiomyosarcoma Treated?
Leiomyosarcoma is treated with total abdominal hysterectomy, bilateral salpingo-oophorectomy for postmenopausal females and those with metastatic disease.
What is the Prognosis of Leiomyosarcoma?
The prognosis of leiomyosarcoma is poor as therapeutic options are limited.
What are Tumors of Uncertain Origin?
Tumors of uncertain origin are the tumors that lack a specific-lineage differentiation.
Examples of tumors of uncertain origin include:
- Synovial sarcoma
- Undifferentiated pleomorphic sarcoma
What is Synovial Sarcoma?
Synovial sarcoma is a malignant soft tissue tumor of uncertain histogenesis with variable epithelial differentiation. Synovial sarcoma has a characteristic chromosomal translocation of t(X;18), SS18-SSX1, -SSX2, -SSX4.
What is the Pathology of Synovial Sarcoma?
The pathology of synovial sarcoma is:
-Etiology: The cause of synovial sarcoma is poorly understood, however, genetic is considered one of the factors.
-Genes involved: SS18, SSX1, SSX2, SSX4.
-Pathogenesis: The sequence of events that lead to synovial sarcoma is driven by the chromosomal translocation t(X;18)(p11;q11) involving genes SS18 and either SSX1, SSX2 or SSX4.
-Morphology: The morphology associated with synovial sarcoma shows monophasic spindle cell, biphasic, poorly differentiated, myxoid, ossifying, and monophasic epithelial like.
-Histology: The histology associated with synovial sarcoma shows the glandular formation of epithelioid tumor cells with sparse luminal microvilli.
How does Synovial Sarcoma Present?
Patients with synovial sarcoma typically affect males of no specific age group. The symptoms, features, and clinical findings associated with synovial sarcoma include no noticeable signs and symptoms.
How is Synovial Sarcoma Diagnosed?
Synovial sarcoma is diagnosed using biopsy and molecular or cytogenetic testing for SS18-SSX fusion.
How is Synovial Sarcoma Treated?
Synovial sarcoma is treated with surgery, radiotherapy, and adjuvant chemotherapy.
What is the Prognosis of Synovial Sarcoma?
The prognosis of synovial sarcoma is fair with survival rates of 50-60% at 5 years and 40-50% at 10 years.
What is Undifferentiated Pleomorphic Sarcoma?
Undifferentiated pleomorphic sarcoma is malignant mesenchymal tumors with pleomorphic cells that are high grade that does not meet the criteria of other classes of soft tissue tumors.
What is the Pathology of Undifferentiated Pleomorphic Sarcoma?
The pathology of undifferentiated pleomorphic sarcoma is:
-Etiology: The cause of undifferentiated pleomorphic sarcoma is unknown.
-Genes involved: None.
-Pathogenesis: The sequence of events that lead to undifferentiated pleomorphic sarcoma is poorly understood.
-Morphology: The morphology associated with undifferentiated pleomorphic sarcoma shows spindle, round/epithelioid, or pleomorphic, demonstrating marked cytologic atypia.
-Histology: The histology associated with undifferentiated pleomorphic sarcoma shows single or clustered spindled cells with nuclear pleomorphism.
How does Undifferentiated Pleomorphic Sarcoma Present?
Patients with undifferentiated pleomorphic sarcoma typically affect males present at the age range of 15-85 years. The symptoms, features, and clinical findings associated with undifferentiated pleomorphic sarcoma present as rapidly enlarging palpable mass but can be incidental findings at screening.
How is Undifferentiated Pleomorphic Sarcoma Diagnosed?
Undifferentiated pleomorphic sarcoma is diagnosed using a biopsy.
How is Undifferentiated Pleomorphic Sarcoma Treated?
Undifferentiated pleomorphic sarcoma is treated using surgical resection.
What is the Prognosis of Undifferentiated Pleomorphic Sarcoma?
The prognosis of undifferentiated pleomorphic sarcoma is poor with a 5-year overall survival rate of 50%.