Myotonic dystrophy is a type of muscular dystrophy, a group of genetic disorders that cause progressive muscle loss and weakness.
What is the Pathology of Myotonic Dystrophy?
The pathology of myotonic dystrophy is:
-Etiology: The microsatellite expansion responsible for DM1 is of cytosine-thymine-guanine (CTG) triplet repeats.
-Genes involved: DMPK gene in myotonic dystrophy type 1 on the long arm of chromosome 19, CNBP gene on chromosome 3 in myotonic dystrophy type 1.
-Pathogenesis: The sequence of events that lead to Myotonic dystrophy involves unusually long messenger RNA that forms clumps inside the cell that interfere with the production of many other proteins. These changes prevent muscle cells and cells in other tissues from functioning normally.
How does Myotonic Dystrophy Present?
Patients with myotonic dystrophy typically affects either male or female present at age range of 20s to 30s. The symptoms, features, and clinical findings associated with myotonic dystrophy include muscle weakness, early onset of cataracts, and myotonia, which is delayed relaxation of muscles after contraction. Other organs affected include the heart, lungs, gastrointestinal tract, skin, and brain. Insulin resistance may also occur.
How is Myotonic Dystrophy Diagnosed?
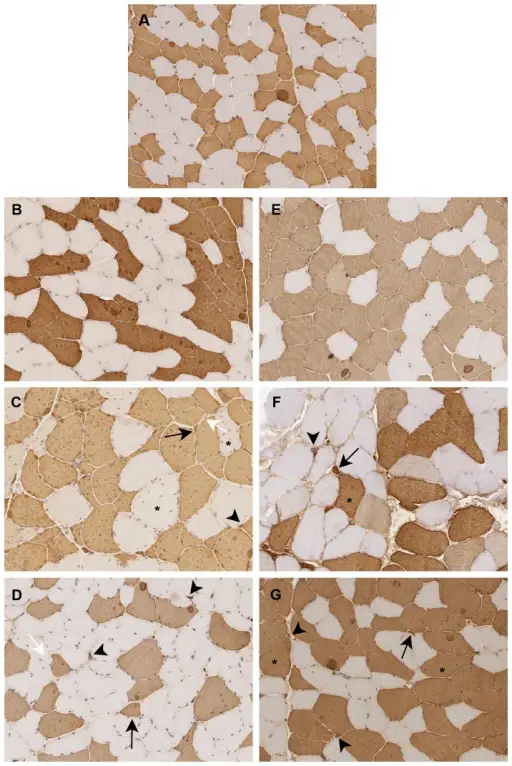
Myotonic dystrophy is diagnosed by doing a physical exam. Laboratory tests for muscle enzymes can be used to clarify the clinical diagnosis of myotonic dystrophy. Electromyography may also be beneficial. Muscle biopsy and molecular testing are confirmatory.
How is Myotonic Dystrophy Treated?
Myotonic dystrophy is treated with mexiletine or carbamazepine which can help relax muscles. NSAIDs, braces, and wheelchairs may be needed as the disease progresses.
What is the Prognosis of Myotonic Dystrophy?
The prognosis of myotonic dystrophy is poor. Life expectancy in non-congenital late-onset or adult onset DM1 is in the early 50s, with pulmonary complications being the leading cause of death, followed by cardiac complications.