Nelson syndrome is a hypothetically life-threatening ailment describing a range of signs associated with bilateral resection of the adrenal gland.
What is the Pathology of Nelson Syndrome?
The pathology of Nelson syndrome is:
-Etiology: The cause of Nelson syndrome is bilateral adrenalectomy, hypopituitarism.
-Genes involved: Unknown.
-Pathogenesis: The sequence of events that lead to Nelson syndrome; following bilateral adrenalectomy, cortisol absence, hypothalamus increase CRH production. Corticotropic cells in the pituitary gland respond to CRH by secretion of ACTH in huge quantities owing to feedback inhibition absence. The upsurge in CRH yields an effect on the corticotropic cells, which hypertrophy creates new growth or increases the original tumor. Surges in proopiomelanocortin production results from CRH elevation.
-Morphology: The morphology associated with Nelson syndrome shows the absence of bilateral adrenal, tumors are inclined to grow bigger.
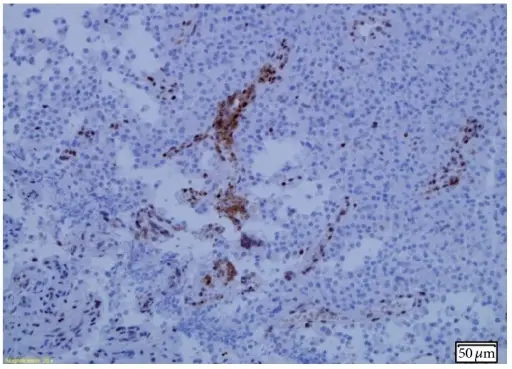
-Histology: The histology associated with Nelson syndrome shows basophilic stain, episodic acidic-Schiff positivity.
How does Nelson Syndrome Present?
Patients with Nelson syndrome are typically females that present at the age range of up to 24 years old following initial bilateral adrenalectomy. The symptoms, features, and clinical findings associated with Nelson syndrome include hyperpigmentation, visual loss, bitemporal hemianopia, headache, fatigue, and weakness.
How is Nelson Syndrome Diagnosed?
Nelson syndrome is diagnosed through laboratory studies which include ACTH fasting plasma levels and brain MRI indicate a pituitary tumor.
How is Nelson Syndrome Treated?
Nelson syndrome is treated through surgical resection of the growth, stereotactic radiosurgery, fractionated radiotherapy, hormonal replacement therapy. Medical care, somatostatin-analogs, dopamine agonists, temozolomide, and sodium valproate.
What is the Prognosis of Nelson Syndrome?
The prognosis of Nelson syndrome is good if surgically treated.