Ocular pathology deals with the varieties and nature of diseases affecting the eye and the surrounding structures. Anatomical regions of the eye include the orbit, eyelid, conjunctiva, sclera, cornea, anterior segment, uvea, retina, vitreous, and optic nerve.
What is Orbit Pathology?
Orbit pathology involves the various ophthalmic diseases affecting the orbit as an anatomical region of the eyes. The orbit comprises a number of tissues that are vulnerable to a plethora of pathologies. Examples of orbit pathology include Grave’s disease (thyroid ophthalmopathy) and other inflammatory conditions.
What is Graves Disease?
Graves disease is an autoimmune disorder of the thyroid gland associated with the swelling of the neck, and protrusion of the eyes called exophthalmos.
What is the Pathology of Graves Disease?
The pathology of Graves disease is production of IgG directed against the thyrotropin receptor, stimulation of the receptor causes the autonomous production of thyroid hormone.
How does Graves Disease Present?
Graves disease presents with a goiter, weight loss, heat intolerance, tachycardia, sleep disorder
How is Graves Disease Diagnosed?
Graves disease is diagnosed by physical examination, thyroid function test, radioactive iodine uptake test, ultrasound, and blood tests.
How is Graves Disease Treated?
Graves disease is treated with radioactive iodine therapy, beta blocker medications, anti-thyroid medications, and vitamin D rich foods.
What is the Prognosis of Graves Disease?
The prognosis of Graves disease is good with proper treatment.
What are other inflammatory conditions of the orbit?
Idiopathic orbital inflammation aka orbital inflammatory pseudotumor
Sclerosing dacryoadenitis
Orbital myositis
Posterior scleritis
What is Proptosis?
Proptosis is the bulging of the eyes causing a positional shift of the eyes in the socket.
What is Wegener Granulomatosis?
Wegener Granulomatosis is a disease condition that causes the inflammation of the blood vessels.
What is the Pathology of Wegener Granulomatosis?
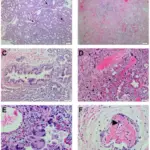
The pathology of Wegener granulomatosis is staphylococcus aureus was hypothesized as the initiating factor of the autoimmune disorder found in patients. Microscopically, inflammation of blood vessels with poorly formed granulomas.
How does Wegener Granulomatosis Present?
Wegener granulomatosis presents with irritation and inflammation of the nose, scleritis, conjunctivitis, glomerulonephritis, hearing loss, arthritis, and subglottic stenosis.
How is Wegener Granulomatosis Diagnosed?
Wegener granulomatosis is diagnosed by Upper respiratory tract tissue biopsy, kidney biopsy, antineutrophil cytoplasmic antibody test (ANCA).
How is Wegener Granulomatosis Treated?
Wegener granulomatosis is treated with Plasmapheresis, administration of rituximab, cyclophosphamide.
What is the Prognosis of Wegener Granulomatosis?
The prognosis of Wegener granulomatosis is with the ancient treatment, life expectancy was less than 5yrs, with modern treatment, patients can live 20+ years after treatment.
What are Neoplasms of the Orbit?
Neoplasms of the orbit include: abnormal growth and proliferation of the surrounding tissues of the eye. Neoplasms or tumors of the orbit can either be benign or malignant. Neoplasms of the orbit include the following:
- Capillary hemangioma
- Encapsulated cavernous hemangioma
- Lymphangioma
What are Capillary Hemangiomas?
Capillary hemangiomas are an overgrowth of capillary blood vessels seen commonly in the skin.
What is the Pathology of Capillary Hemangiomas?
The pathology of capillary hemangiomas is abnormal proliferation of normal tissue in a normal position.
How do Capillary Hemangiomas Present?
Capillary hemangiomas present with cutaneous lesion, subcutaneous lesion, orbital lesion.
How are Capillary Hemangiomas Diagnosed?
Capillary hemangiomas are diagnosed by ultrasound, CT scan, and MRI.
How are Capillary Hemangiomas Treated?
Capillary hemangiomas are treated with beta-blocker, radiation therapy, surgical excision, laser photocoagulation.
What is the Prognosis of Capillary Hemangiomas?
The prognosis of capillary hemangiomas is Most hemangiomas disappear later by undergoing spontaneous regression.
What are Encapsulated Cavernous Hemangiomas?
Encapsulated cavernous hemangiomas medical conditions involving dilated endothelial lined vascular channels filled with slowly flowing fluid.
What is the Pathology of Encapsulated Capillary Hemangiomas?
The pathology of encapsulated capillary hemangiomas is Encapsulated nodular mass of inflamed vascular tissue. Tumor growth is a result of budding of the vascular channels into the surrounding soft tissues.
How do Encapsulated Capillary Hemangiomas Present?
Encapsulated capillary hemangiomas present with osseous lesion, unilateral lesion, solitary lesions.
How are Encapsulated Capillary Hemangiomas Diagnosed?
Encapsulated capillary hemangiomas are diagnosed by physical examination, family history, X-ray, orbital echography, tonometry, and susceptibility weighted imaging.
How is Encapsulated Capillary Hemangiomas Treated?
Encapsulated capillary hemangiomas are treated with craniotomy, stereotactically assisted craniotomy, and stereotactic radiosurgery.
What is the Prognosis of Encapsulated Capillary Hemangiomas?
The prognosis of encapsulated capillary hemangiomas is excellent vision prognosis in a case of surgical excision although hyperopia may persist as a result of mass effect against the posterior globe. Recurrence may occur in the case of incomplete excision.
What are Lymphangiomas?
Lymphangiomas are multi cystic, localized malformation of the lymphatic system.
What is the pathology of Lymphangiomas?
The pathology of lymphangiomas is collection of lymphatic cisterns in the deep subcutaneous plane. Cisterns get separated from the normal lymphatic network but communicate with the superficial lymph vesicles through dilated lymph nodes.
How do Lymphangiomas Present?
Lymphangiomas present with tiny reddish or blue dots, small clusters of vesicles, subcutaneous nodules with rubbery consistency.
How are Lymphangiomas Diagnosed?
Lymphangiomas are diagnosed by CT scan, and MRI.
How are Lymphangiomas Treated?
Lymphangiomas is treated with sodium tetradecyl sulfate, surgical incision, cryotherapy, sclerotherapy, radiofrequency therapy, and simple electrodessication.
What is the Prognosis of Lymphangiomas?
The prognosis of lymphangiomas is excellent prognosis, patients expected to live a full healthy life with no risk of malignant transformation.
What is Eyelid Pathology?
Eyelid pathology deals with the various diseases that affect the eyelid. Most eyelid pathologies are due to clogged ducts resulting in inflammation.
What are Eyelid Neoplasms?
Eyelid neoplasms are abnormal tissue growth of the eyelid by cellular proliferation that either be benign or malignant. Basal cell carcinoma is the most common malignancy of the eye.
Other neoplasms of the eyelid include sebaceous carcinoma and Kaposi sarcoma.
What is Basal Cell Carcinoma?
Basal cell carcinoma is a malignant epidermal tumor that affects the basement membrane of epithelial cells.
What is the Pathology of Basal Cell Carcinoma?
The pathology of basal cell carcinoma is Forms strands, cords and island of tumor appearing similar to the normal epithelial basal layer.
How does Basal Cell Carcinoma Present?
Basal cell carcinoma presents with Pearly appearance, crusting, telangiectasia, erosion or ulceration.
How is Basal Cell Carcinoma Diagnosed?
Basal cell carcinoma is diagnosed by assessment of ocular motility, assessment for proptosis, assessment of madarosis, assessment of eyelid malposition, incisional or excisional tissue biopsy.
How is Basal Cell Carcinoma Treated?
Basal cell carcinoma is treated with administration of Vismodegib, topical imiquimod 5% cream, surgical excision, sonidegib, intron-A, efudex, tazarotene, PD1-inhibitor.
What is the Prognosis of Basal Cell Carcinoma?
The prognosis of basal cell carcinoma is a 5 years cure rate. Prognosis gets worse with deeply invasive tumors, inadequate treatment, long-standing lesions, lesions greater than 3 cm.
What is Sebaceous Carcinoma?
Sebaceous carcinoma is a rare malignant tumor of the skin mostly common to the eyelid.
What is the Pathology of Sebaceous Carcinoma?
The pathology of sebaceous carcinoma arises from the adnexal epithelium of sebaceous glands commonly the meibomian glands or glands of Zeis.
How does Sebaceous Carcinoma Present?
Sebaceous carcinoma presents with yellow, hard, painless subcutaneous nodule, red and yellow or red and brown ulcerated papules, may also appear as nonmelanoma skin cancer.
How is Sebaceous Carcinoma Diagnosed?
Sebaceous carcinoma is diagnosed by conjunctiva biopsy, and sentinel lymph node biopsy.
How is Sebaceous Carcinoma Treated?
Sebaceous carcinoma is treated with targeted therapy as (retinoid receptor ligands, anti-androgen), chemotherapy, immunotherapy, Mohs micrographic surgery, and wide local excision.
What is the Prognosis of Sebaceous Carcinoma?
The prognosis of sebaceous carcinoma is fair.
What is Kaposi Sarcoma?
Kaposi sarcoma is an indolent angio proliferative spindle cell tumor derived from endothelial and immune cells infected with human herpes virus type 8.
What is the Pathology of Kaposi Sarcoma?
The pathology of Kaposi sarcoma arises as a cancer of lymphatic endothelium and forms vascular channels that fill with blood cells.
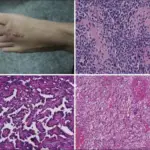
How does Kaposi Sarcoma Present?
Kaposi sarcoma presents with cutaneous lesions especially on the lower extremities, head and neck, non pruritic palpable lesions, brown, red or pink colored lesions.
How is Kaposi Sarcoma Diagnosed?
Kaposi sarcoma is diagnosed by microscopic examination of tissue biopsy, and medical imaging.
How is Kaposi Sarcoma Treated?
Kaposi sarcoma is treated with radiation therapy, cryosurgery, chemotherapy, and antiretroviral beta-blocker.
What is the Prognosis of Kaposi Sarcoma?
The prognosis of Kaposi sarcoma is dependent on the extent of disease.
What is Conjunctiva Pathology?
Conjunctiva pathology covers the wide scope and forms of the diseases of the conjunctiva.
Scarring is a common conjunctival pathology.
What is Conjunctival Scarring?
Conjunctival scarring is cicatricial condition of the conjunctiva associated with the tissue shrinkage and mostly with distortion of fornices and the lid. Conjunctival scarring can be due to chlamydia trachomatis infection, chemicals like alkalis, cicatricial pemphigoid, and tear deficiency like Sjogren’s syndrome.
What is Pinguecula?
Pinguecula is an abnormal growth of the tissue on the conjunctiva. There may be a yellow limbus associated with submucosal elevation on the conjunctiva due to actinic damage.
What is Pterygium?
Pterygium is a common ocular surface lesion emanating in the limbal conjunctiva within the palpebral fissure with progressive involvement of the cornea.
Limbus associated submucosal elevation on the conjunctiva due to actinic damage.
What are Conjunctival Neoplasms?
Conjunctival neoplasms include:
- Melanocytic neoplasms.
- Squamous neoplasms.
- Conjunctival intraepithelial neoplasia
- Squamous cell carcinoma
- Mucoepidermoid carcinoma.
- Conjunctival nevi
- Conjunctival melanoma
- Inflamed juvenile nevus
- Primary acquired melanosis with atypia.
What is Pathology of the Sclera?
Pathology of the sclera deals with the varieties of disorder that alters the proper function of the sclera.
Pathology of the sclera may include:
- Necrotizing scleritis due to rheumatoid arthritis.
What Conditions are Associated with Blue Sclera?
Conditions that are associated with blue sclera are:
- Congenital melanosis oculi
- Nevus of Ota
- Osteogenesis imperfecta
- Scleritis (tyndall effect)
- Staphyloma (increased intraocular pressure)
What is Cornea Pathology?
Corneal pathology deals with the clinical conditions involving the cornea
Particular conditions that may cause corneal pathology include:
- Keratitis
- Corneal ulcers
- Corneal degenerations
- And corneal dystrophies
What is Keratitis?
Keratitis is inflammation of the cornea caused by disease, injury, or infection. Contacts can cause keratitis by over wearing of contact lenses.
What is the Pathology of Keratitis?
The pathology of Keratitis is irritation of the cornea caused by a number of factors such as allergy, bacteria, fungi, viral infection and injury to the cornea.
How does Keratitis Present?
Keratitis presents with pain in the eye, and photophobia.
How is Keratitis Diagnosed?
Keratitis is diagnosed by histological examination, and medical history.
How is Keratitis Treated?
Keratitis is treated with antibiotics, eye drops, and surgery if indicated.
What is the Prognosis of Keratitis?
The prognosis of Keratitis gets better with medications and eradication of risk factors.
What is a Corneal Ulcer?
Corneal ulcers are loss of tissue of the cornea resulting in open soreness.
What is the Pathology of Corneal Ulcer?
The pathology of corneal ulcer is vitamin A deficiency, fungal, viral and amoebic infection of the cornea.
How does Corneal Ulcer Present?
Corneal ulcer presents with itchy eyes, pus-like discharge from the eyes, and watery eyes.
How is Corneal Ulcer Diagnosed?
Corneal ulcer is diagnosed by fluorescein eye stain, histological examination, etc.
How is Corneal Ulcer Treated?
Corneal ulcer is treated with antibacterial, antifungal, and antiviral eye drops and medications, and corneal transplant.
What is the Prognosis of Corneal Ulcer?
The prognosis of corneal ulcer is the patient may respond to treatment but may lead to partial loss of vision.
What are Corneal Degenerations?
Corneal degenerations are the gradual degeneration of the cornea tissue.
What are Band Keratopathies?
Band keratopathies are the degeneration of the cornea and/or the conjunctiva characterized by deposition.
Examples include:
- Actinic band keratopathy
- Calcific band keratopathy
What is Actinic Band Keratopathy?
Actinic band keratopathy is the degeneration of cornea and/ or conjunctiva characterized by globules of varying sizes found in the Bowman’s membrane, sub-epithelium and cornea stroma.
What is the Pathology of Actinic Band Keratopathy?
The pathology of actinic band keratopathy is deposits in the Bowman’s membrane, cornea stroma and sub-epithelium.
How does Actinic Band Keratopathy Present?
Actinic band keratopathy presents asymptomatic but reduces visual acuity in severe cases.
How is Actinic Band Keratopathy Diagnosed?
Actinic band keratopathy is diagnosed by histological examination, and physical examination.
How is Actinic Band Keratopathy Treated?
Actinic band keratopathy is treated with superficial keratectomy, lamellar keratoplasty, penetrating keratoplasty, and phototherapeutic keratectomy.
What is the Prognosis of Actinic Band Keratopathy?
The prognosis of actinic band keratopathy generally disappears after some time.
What is Calcific Band Keratopathy?
Calcific band keratopathy is a cornea degeneration that is most often composed of dust-like calcium deposits in the sub-epithelium and anterior stroma.
What is the Pathology of Calcific Band Keratopathy?
The pathology of calcific band keratopathy is calcium deposits in the anterior stroma, epithelial basement membrane and bowman’s layer.
How does Calcific Band Keratopathy Present?
Calcific band keratopathy presents with ocular irritation, redness, and photophobia.
How is Calcific Band Keratopathy Diagnosed?
Calcific band keratopathy is diagnosed by history and slit lamp examination.
How is Calcific Band Keratopathy Treated?
Calcific band keratopathy is treated with surgery, antibiotics, eye drops, steroids, and eye drops.
What is the Prognosis of Calcific Band Keratopathy?
The prognosis of calcific band keratopathy is generally favorable but it is important to treat the underlying condition to reduce recurrence.
What is Keratoconcus?
Keratoconus is an uncommon corneal disorder whereby there is thinning and steepening of the central cornea or paracentral cornea.
What is the Pathology of Keratoconus?
The pathology of Keratoconus is corneal scarring, fragment of bowman’s layer, thinning of overlying epithelial and stroma.
How does Keratoconcus Present?
Keratoconcus presents with Munson’s sign, asymmetric refractive error, progressive astigmatism, breaks in bowman’s membrane.
How is Keratoconus Diagnosed?
Keratoconus is diagnosed by slit lamp examination, video keratography, ultrasound pachymetry, physical examination.
How is Keratoconus Treated?
Keratoconus is treated with soft toric contact lenses, corneal collagen cross-linking, cycloplegic agent, and surgery.
What is the Prognosis of Keratoconus?
The prognosis of Keratoconus is with proper treatment, patients retain normal vision but in most cases with lenses.
What is Pseudophakic Bullous Keratopathy?
Pseudophakic bullous keratopathy is the development of irreversible corneal edema after intraocular lens implantation or cataract surgery.
What is the Pathology of Pseudophakic Bullous Keratopathy?
The pathology of pseudophakic bullous keratopathy is damage to the endothelial leading to the reduction in corneal transparency.
How does Pseudophakic Bullous Keratopathy Present?
Pseudophakic bullous keratopathy presents with epithelial bullae, increased corneal thickness, endothelial fold, and corneal edema.
How is Pseudophakic Bullous Keratopathy Diagnosed?
Pseudophakic bullous keratopathy is diagnosed by histology of recent intraocular surgery, and slit lamp examination.
How is Pseudophakic Bullous Keratopathy Treated?
Pseudophakic bullous keratopathy is treated with administration of hypertonic saline drops, antibiotic drops, lubricating drops, use of bandage contact lens, cornea culture, and corneal transplant.
What is the Prognosis of Pseudophakic Bullous Keratopathy?
The prognosis of pseudophakic bullous keratopathy is a good prognosis with appropriate penetrating keratoplasty.
What is Bullous keratopathy and stromal edema Aka Fuchs Endothelial Dystrophy?
Bullous keratopathy and stromal edema aka Fuchs endothelial dystrophy is the swelling of the cornea due to build of fluid in the endothelial layer.
What is the Pathology of Fuchs Endothelial Dystrophy?
The pathology of Fuchs endothelial dystrophy is loss of endothelial cells and presence of guttata.
How does Fuchs Endothelial Dystrophy Present?
Fuchs endothelial dystrophy presents with vascular ingrowth to the cornea, stromal edema, epithelial microcytes, epithelial bullae.
How is Fuchs Endothelial Dystrophy Diagnosed?
Fuchs endothelial dystrophy is diagnosed by pachymetry, and specular microscopy.
How is Fuchs Endothelial Dystrophy Treated?
Fuchs endothelial dystrophy is treated with hypertonic saline ointment or drops, bandage contact lens, penetrating keratoplasty, descemet membrane endothelial keratoplasty.
What is the Prognosis of Fuchs Endothelial Dystrophy?
The prognosis of Fuchs endothelial dystrophy is an excellent prognosis especially after surgery.
What are Stromal Dystrophies?
Stromal dystrophies are inherited non-inflammatory bilateral cornea disorders. It primarily affects the stroma but extends to the cornea overtime causing a form of cloudiness.
What are Corneal Dystrophies?
Corneal dystrophies are a group of inherited eye disorders characterized by abnormal deposition in the cornea.
What is Anterior Segment Pathology?
Anterior segment pathology is a spectrum of disease affecting the development of the frontal segment of the eye.
Examples of anterior segment pathology include:
- Cataract
- Glaucoma
- Endophthalmitis
- Panophthalmitis
What is Cataract?
Cataract is the clouding of the clear lens of the eye.
Examples of cataract include:
- Lenticular opacity
- Age-related cataract (nuclear sclerosis)
- Posterior subcapsular cataract
- Morganium cataract.
What is the Pathology of Cataract?
The pathology of cataract is diffusion of toxin with the ocular fluid supplied to the crystalline lens leading to development of opacification.
How does Cataract Present?
Cataract presents with blurred vision, and vision loss.
How is Cataract Diagnosed?
Cataract is diagnosed by comprehensive dilated eye examination, brightness acuity test, corneal topography, endothelial cell count.
How is Cataract Treated?
Cataract is treated with a balanced diet, UV blocking sunglasses, phacoemulsification, and extracapsular cataract extraction if indicated.
What is the Prognosis of Cataract?
The prognosis of cataract is an excellent prognosis in the case of a cataract extraction, although primary pathology plays an important role in the final visual prognosis.
What is Glaucoma?
Glaucoma is an abnormal condition of increased intraocular pressure that may progress to vision loss.
Glaucoma is characterized by visual field changes and cup of the optic nerve.
The types of glaucoma include:
- Angle-closure glaucoma
- Open-angle glaucoma
- Primary open-angle glaucoma
- Secondary open-angle glaucoma
- Ghost cell glaucoma
- Pigmentary glaucoma
- Melanocytic glaucoma
- Neovascular glaucoma.
What is the Pathology of Glaucoma?
The pathology of glaucoma is poorly understood but may include all that causes increase in the intraocular pressure.
How does Glaucoma Present?
Glaucoma presents with subtle findings that may be asymptomatic and patients may experience distortion vision, peripheral vision loss, and blurred vision.
How is Glaucoma Diagnosed?
Glaucoma is diagnosed by fundoscopic examination, tonometry, gonioscopy, and visual field testing.
How is Glaucoma Treated?
Glaucoma is treated with beta-blocker, prostaglandin, latanoprost, and trabeculoplasty.
What is the Prognosis of Glaucoma?
The prognosis of glaucoma is good for most patients with adequate treatment. Glaucoma may lead to permanent vision loss if not treated.
What is Endophthalmitis?
Endophthalmitis is Inflammation within the vitreous humor.
What is the Pathology of Endophthalmitis?
The pathology of endophthalmitis is ocular blood barrier and intraocular colonization breakdown.
How does Endophthalmitis Present?
Endophthalmitis presents with hypopyon, and martin-farina sign.
How is Endophthalmitis Diagnosed?
Endophthalmitis is diagnosed by CT scan, ultrasound sound, anterior segment OCT, and fundus fluorescein angiogram.
How is Endophthalmitis Treated?
Endophthalmitis is treated with intravitreally injected steroids and antibiotics, vancomycin and ceftazidime injection, pars plana vitrectomy, and evisceration if indicated.
What is the Prognosis of Endophthalmitis?
The prognosis of endophthalmitis depends on the causative organism, nature of disease, and the patient’s systemic stability.
What is Panophthalmitis?
Panophthalmitis is inflammation that involves the choroid, retina, and sclera that extends into the orbit.
What is the Pathology of Panophthalmitis?
The pathology of panophthalmitis is often developed from endophthalmitis.
How does Panophthalmitis Present?
Panophthalmitis presents with hypopyon worsen, conjunctiva chemosis, eyelid edema, purulent discharge restricted and painful ocular movement.
How is Panophthalmitis Diagnosed?
Panophthalmitis is diagnosed by ultrasonography, and contrast enhanced MRI.
How is Panophthalmitis Treated?
Panophthalmitis is treated with intravitreal and periocular injection of combined antibiotics and dexamethasone.
What is the Prognosis of Panophthalmitis?
The prognosis of panophthalmitis is fair.
What is Uvea Pathology?
Uvea pathology deals with the spectrum of diseases affecting the uvea tract.
Uvea pathology includes:
- Uveitis
- Uveal neoplasms
What is Uveitis?
Uveitis is the inflammation of the middle layer of the eye known as the uvea layer. The most common is the iritis (anterior uveitis), others include granulomatous uveitis, and sympathetic ophthalmia.
What is the Pathology of Uveitis?
The pathology of uveitis is turgidity of the tissues of the uvea layer of the eye due to substance accumulation.
How does Uveitis Present?
Uveitis presents with light sensitivity, redness, and blurred vision.
How is Uveitis Diagnosed?
Uveitis is diagnosed by ophthalmoscopy, tonometry, slit lamp examination, radiography, and CT scan.
How is Uveitis Treated?
Uveitis is treated with steroids, immunosuppressant drugs, antibiotics, antiviral medications, vitrectomy, and medication release implant.
What is the Prognosis of Uveitis?
The prognosis of uveitis is excellent within months.
What are Uveal Neoplasms?
Uveal neoplasms include:
- Uveal nevi
- Uveal melanoma
What are Uveal Nevi?
Uveal nevi are benign lesions of the uvea layer of the eye. Uvea nevi rarely produces glaucoma.
What is the Pathology of Uveal Nevi?
The pathology of uveal nevi is moles of unclear deposits on the eyeball and other hyperpigmentation spots.
How does Uveal Nevi Present?
Uveal nevi presents with visible freckles in the eye.
How is Uveal Nevi Diagnosed?
Uveal nevi is diagnosed by fundoscopy.
How is Uveal Nevi Treated?
Uveal nevi is treated with local excision, or argon laser photoablation.
What is the Prognosis of Uveal Nevi?
The prognosis of uveal nevi is typically fine.
What are Uveal melanomas?
Uveal melanomas are cancers of the eye involving the tissues of the uvea.
What is the Pathology of Uveal Melanoma?
The pathology of uveal melanoma is malignant proliferation of melanocytes in the uvea.
How does Uveal Melanoma Present?
Uveal melanoma presents with proptosis, photopsia, diplosia, metamorphopsia and may be asymptomatic in some cases.
How is Uveal Melanoma Diagnosed?
Uveal melanoma is diagnosed by ophthalmoscopy, and biomicroscopy.
How is Uveal Melanoma Treated?
Uveal melanoma is treated with photocoagulation photodynamic therapy, proton beam radiotherapy, transpupillary thermotherapy, and brachytherapy enucleation.
What is the Prognosis of Uveal Melanoma?
The prognosis of uveal melanoma is poor.
What is Retina Pathology?
Retina pathology is a broad spectrum of pathologies solely affecting the retina of the eye.
Retina pathology includes:
- Retinal detachment
- Retinal vascular disease
- Retinopathy of prematurity
What is Retinal Detachment?
Retinal detachment is separation of the neurosensory retina from the retinal pigment epithelium.
What is Retinal Vascular Disease?
Retinal vascular disease is a clinical condition with abnormal vasculatures of the retina.
Examples of retinal vascular diseases include:
- Retinopathy of prematurity
- Retrolental fibroplasia
- Sickle retinopathy
- Radiation vasculitis
- Retinal vasculitis
- Retinal artery occlusion
- Retinal vein occlusion
What is Retinopathy of Prematurity?
Retinopathy of prematurity is a potential blindness disorder primarily affecting prematurely born infants.
What is the Pathology of Retinopathy of Prematurity?
The pathology of retinopathy of prematurity is incomplete outward growth of the blood vessels from the central part of the retina.
How does Retinopathy of Prematurity Present?
Retinopathy of prematurity presents with birth weight less than 1.5kg, tortuosity of vessels.
How is Retinopathy of Prematurity Diagnosed?
Retinopathy of prematurity is diagnosed by dilated fundus examination with scleral depression.
How is Retinopathy of Prematurity Treated?
Retinopathy of prematurity is treated with oral propranolol, intravitreal injection of bevacizumab, scleral buckling, vitrectomy.
What is the Prognosis of Retinopathy of Prematurity?
The prognosis of retinopathy of prematurity is fair, but it can progress to a more severe state with improper or no treatment.
What is Retrolental Fibroplasia?
Retrolental fibroplasia is an abnormal replacement of the sensory retina by fibrous tissue and blood vessels.
What is the Pathology of Retrolental Fibroplasia?
The pathology of retrolental fibroplasia is replacement of retina by fibrous tissue and also blood vessels.
How does Retrolental Fibroplasia Present?
Retrolental fibroplasia presents with birth weight less than 1.5kg, tortuosity of vessels.
How is Retrolental Fibroplasia Diagnosed?
Retrolental fibroplasia is diagnosed by dilated fundus examination with scleral depression.
How is Retrolental Fibroplasia Treated?
Retrolental fibroplasia is treated with oral propranolol, intravitreal injection of bevacizumab, scleral buckling, and vitrectomy.
What is the Prognosis of Retrolental Fibroplasia?
The prognosis of retrolental fibroplasia is poor if not properly managed.
What is Sickle Cell Retinopathy?
Sickle cell retinopathy is an ocular manifestation of the spectrum of sickle cell disease.
What is the Pathology of Sickle Cell Retinopathy?
The pathology of sickle cell retinopathy is trapping of the sickle shaped red blood cell in blood vessels of the eye.
How does Sickle Cell Retinopathy Present?
sickle cell retinopathy presents with comma shaped blood vessels in the bulbar conjunctiva.
How is Sickle Cell Retinopathy Diagnosed?
Sickle cell retinopathy is diagnosed by fluorescein angiography, spectral domain optical coherence tomography, and funduscopic examination.
How is Sickle Cell Retinopathy Treated?
Sickle cell retinopathy is treated with hyperbaric oxygen therapy, hydroxyurea, hydroxycarbamide treatment, intravitreal anti-vascular endothelial growth factor, scatter laser coagulation, and surgery.
What is the Prognosis of Sickle Cell Retinopathy?
The prognosis of sickle cell retinopathy is some do not survive beyond infancy, reduced life expectancy as symptoms manifest. New treatments are improving life expectancy.
What is Radiation Vasculitis?
Radiation vasculitis is an inflammatory condition of blood vessels induced by exposure to radiation treatment of another medical condition.
What is the Pathology of Radiation Vasculitis?
The pathology of radiation vasculitis is irritation of smooth muscle, endothelial and immune cells.
How does Radiation Vasculitis Present?
Radiation vasculitis presents with ischemia, ischemic stroke, transient ischemic attack, and dizziness.
How is Radiation Vasculitis Diagnosed?
Radiation vasculitis is diagnosed by physical examination, medical history, magnetic resonance imaging, and computed tomography (CT) angiography.
How is Radiation VasculitisTreated?
Radiation vasculitis is treated with medications such as aspirin.
What is the Prognosis of Radiation Vasculitis?
The prognosis of radiation vasculitis is good.
What is Retinal Vasculitis?
Retinal vasculitis is the inflammatory condition of the retina vasculatures.
What is the Pathology of Retinal Vasculitis?
The pathology of retinal vasculitis is autoimmune disease induced by antecedent infection with microbes cross reacting with antigens.
How does Retinal Vasculitis Present?
Retinal vasculitis presents with retinal ischemia, frosted branch angiitis, retinal necrosis, intraretinal infiltrates, and perivascular sheathing.
How is Retinal Vasculitis Diagnosed?
Retinal vasculitis is diagnosed by slit-lamp biomicroscopy, and indirect ophthalmoscopy.
How is Retinal Vasculitis Treated?
Retinal vasculitis is treated with intravitreal corticosteroid, intravitreal immunosuppressants, and antimicrobial therapy.
What is the Prognosis of Retinal Vasculitis?
The prognosis of retinal vasculitis is good prognosis with adequate immunosuppressive therapy, but poor visual outcome in a complicated state.
What is Retinal Artery Occlusion?
Retinal artery occlusion is an obstruction of retina arterial blood supply.
What is the Pathology of Retinal Artery Occlusion?
The pathology of retinal artery occlusion is obstruction of retina artery lumen by resulting in restricted blood flow.
How does Retinal Artery Occlusion Present?
Retinal artery occlusion presents with pale optic disc, retinal pigment epithelial mottling, thinned vessel, and attenuated vessels.
How is Retinal Artery Occlusion Diagnosed?
Retinal artery occlusion is diagnosed by slit-lamp biomicroscopy,
How is Retinal Artery Occlusion Treated?
Retinal artery occlusion is treated with symptomatic management.
What is the Prognosis of Retinal Artery Occlusion?
The prognosis of retinal artery occlusion is poor, and often proceeds to vision loss in severe cases.
What is Retinal Vein Occlusion?
Retinal vein occlusion is a vascular disease characterized by the engorgement and dilation of retinal veins.
What is the Pathology of Retinal Vein Occlusion?
The pathology of retinal vein occlusion is obstruction of retina veins lumen causing a restricted blood flow.
How does Retinal Vein Occlusion Present?
Retinal vein occlusion presents with dark spots, lines floating in vision, pain and pressure in the eye.
How is Retinal Vein Occlusion Diagnosed?
Retinal vein occlusion is diagnosed by fluorescein angiography.
How is Retinal Vein Occlusion Treated?
Retinal vein occlusion is treated with anti-vascular endothelial growth factor, focal laser therapy, laser surgery, hyperbaric oxygen therapy, and sublingual isosorbide dinitrate.
What is the Prognosis of Retinal Vein Occlusion?
The prognosis of retinal vein occlusion is fair. Vision may be restored in some patients, while some may not see improvements.
What is Age Related Macular Degeneration?
Age related macular degeneration is the loss of central vision induced by the degeneration of the macular of the retina manifesting after age 50.
What is the Pathology of Age Related Macular Degeneration?
The pathology of age related macular degeneration is degeneration involving the retinal photoreceptors, pigment epithelium and Bruch’s membrane.
How does Age related Macular Degeneration Present?
Age related macular degeneration presents with blurry vision, distorted vision, partial vision loss, and neovascularization.
How is Age related Macular Degeneration Diagnosed?
Age related macular degeneration is diagnosed by Amsler grid test, pupillary dilation test, optical coherence tomography, and fluorescein angiography.
How is Age Related Macular Degeneration Treated?
Age related macular degeneration is treated with anti-VEGF medications, vitamin supplementation, and laser therapy.
What is the Prognosis of Age Related Macular Degeneration?
The prognosis of age related macular degeneration can last for years or life-long.
What is Retinitis Pigmentosa?
Retinitis pigmentosa is severe vision impairment induced by a rare, inherited degenerative retina disorder.
What is the Pathology of Retinitis Pigmentosa?
The pathology of retinitis pigmentosa is a degenerative disease involving the deposition of pigments on the peripheral of the retina.
How does Retinitis Pigmentosa Present?
Retinitis pigmentosa presents with central vision loss, gradual loss of peripheral vision, night vision loss, and color vision impairment.
How is Retinitis Pigmentosa Diagnosed?
Retinitis pigmentosa is diagnosed by electroretinography, genetic testing, visual field testing, and optical coherence tomography.
How is Retinitis Pigmentosa Treated?
Retinitis pigmentosa is treated with controlled quantities of VIT. A, eye drop, and ARGUS II implantation when indicated.
What is the Prognosis of Retinitis Pigmentosa?
The prognosis of retinitis pigmentosa is fair.
What is Retinitis?
Retinitis is the general term that covers all inflammatory conditions of the retina.
What is the Pathology of Retinitis?
The pathology of retinitis is accumulation of substance causing swelling of the retina cells or the vasculatures.
How does Retinitis Present?
Retinitis presents with night blindness, tunnel vision, color vision impairment, and photophobia.
How is Retinitis Diagnosed?
Retinitis is diagnosed by visual field test, electroretinogram, genetic test, and ophthalmoscopy.
How is Retinitis Treated?
Retinitis is treated with retina implantation, acetazolamide, sunglasses, intravitreal clindamycin and dexamethasone, and laser therapy.
What is the Prognosis of Retinitis?
The prognosis of retinitis is poor if left untreated. With treatment, some vision recovery may be possible.
What are Retinal Neoplasms?
Retinal neoplasms are benign or malignant abnormal retina tissue proliferation.
Examples of retinal neoplasms include:
- Retinoblastoma
- Retinal lymphoma
- Retinal capillary hemangioma
- Retinal astrocytic hamartoma
What is Retinoblastoma?
Retinoblastoma is eye cancer that originates from the retina.
What is the Pathology of Retinoblastoma?
The pathology of retinoblastoma is mutational inactivation of both alleles of RB1 gene mapping to chromosome 13q14 and encodes retinoblastoma protein acting as tumor suppressor.
How does Retinoblastoma Present?
Retinoblastoma typically presents in affected children with light induced white coloration of the pupil, different directional eye focus, redness, and swelling of the eye.
How is Retinoblastoma Diagnosed?
Retinoblastoma is diagnosed by eye examination, ultrasound image test, CT scan, MRI.
How is Retinoblastoma Treated?
Retinoblastoma is treated with intra-arterial chemotherapy, intravitreal chemotherapy, laser therapy, cryotherapy, radiation therapy, and surgery.
What is the Prognosis of Retinoblastoma?
The prognosis of retinoblastoma is fair.
What is Retinal Lymphoma?
Retinal lymphoma is a severe malignant neoplasm associated with cerebral disease.
What is the Pathology of Retinal Lymphoma?
The pathology of retinal lymphoma is malignancy often associated with B-cells.
How does Retinal Lymphoma Present?
Retinal lymphoma presents with swelling in the eye, redness, decreased or lost vision, and floaters.
How is Retinal Lymphoma Diagnosed?
Retinal lymphoma is diagnosed by vitreous biopsy, MRI, B-scan ultrasound imaging, and neuroimaging.
How is Retinal Lymphoma Treated?
Retinal lymphoma is treated with systemic chemotherapy, radiotherapy, vitrectomy, lenalidomide and rituximab.
What is the Prognosis of Retinal Lymphoma?
The prognosis of retinal lymphoma is poor with overall survival time of 3 years after diagnosis.
What is Optic Nerve Pathology?
Optic nerve pathology deals with the spectrum of diseases targeted towards the nerve of vision.
Examples of optic nerve pathology include:
- Anterior ischemic optic neuropathy
- Papilledema
- Optic nerve damage
- Optic neuritis
- Other optic neuropathies
What is Anterior Ischemic Optic Neuropathy?
Anterior ischemic optic neuropathy is optic nerve ischemia or infarction that can result in transient or segmental vision loss.
What is Papilledema?
Papilledema is edema of the optic nerve due to compression or pressure.
What is Optic Nerve Damage?
Optic nerve damage is the disruption of the normal function of the optic nerve due to trauma, inflammation, diseases or deterioration.
What are Other Optic Neuropathies Associated With?
Other optic neuropathies are associated with:
Nutritional deficiencies
Toxins
Methanol
What is Optic Neuritis?
Optic neuritis is vision loss due to optic nerve demyelination. Optic neuritis is often seen in patients that have multiple sclerosis.
What is the Pathology of Optic Neuritis?
The pathology of optic neuritis is inflammatory demyelination of optic nerve caused by immune disease. Myelin is destroyed, exposing and causing the axon to poorly conduct impulses.
How does Optic Neuritis Present?
Optic neuritis presents with blurry vision or vision loss, eye pain, or color blindness.
How is Optic Neuritis Diagnosed?
Optic neuritis is diagnosed by an eye examination, color vision measurement, swinging flashlight test to check the afferent pupillary response, and optical coherence tomography.
How is Optic Neuritis Treated?
Optic neuritis is treated with administration of IV steroid, oral steroid, IV methylprednisolone, and adrenocorticotropic hormone.
What is the Prognosis of Optic Neuritis?
The prognosis of optic neuritis is visual recovery occurs within a month after treatment starts.
What is Phthisis Bulbi?
Phthisis bulbi is a clinical condition representing the end stage ocular response to eye diseases damage or injury causing scarring, inflammation, atrophy and eventually disorganization of the globe and the intraocular contents.
What is the Pathology of Phthisis Bulbi?
The pathology of phthisis bulbi is the proliferative reaction of a number of cells, internal disorganization, and inflammatory reaction.
How does Phthisis Bulbi Present?
Phthisis bulbi presents with intraocular inflammation, hypotony, microphthalmos, enophthalmos, and choroidal detachment.
How is Phthisis Bulbi Diagnosed?
Phthisis bulbi is diagnosed by physical examination, ocular history, and imaging tests.
How is Phthisis Bulbi Treated?
Phthisis bulbi is treated with administration of steroids, antibiotics, immune suppressing medications, and prosthesis.
What is the Prognosis of Phthisis Bulbi?
The prognosis of phthisis bulbi is curable in children with prompt treatment, but may lead to end stage eye if not treated.